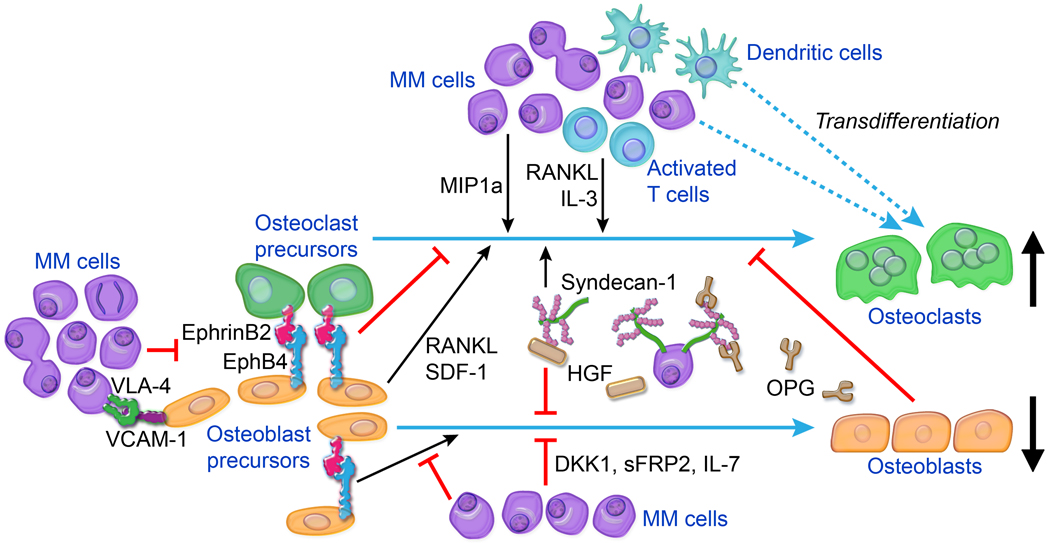
Figure 1.
Main cellular and molecular factors associated with MM-induced bone disease. Osteolytic lesions are induced by uncoupling of bone metabolism, resulting in increased bone resorption by osteoclasts and reduced bone formation by osteoblasts. Interactions between MM cells and various BM cells (e.g., osteoblast and osteoblast precursors, activated T lymphocytes, dendritic cells) result in increased production of osteoclast-activating factors (e.g., RANKL, IL-3, MIP1α) and/or osteoblast-inactivating factors (e.g., DKK1, sFRP2, IL-7). OPG levels in lytic lesions are low as a consequence of reduced osteoblast numbers and of OPG internalization and degradation by MM cells in a mechanism mediated by binding to syndecan-1 on MM cell surfaces. Syndecan-1 molecules shed from MM cells also bind and localize factors such as HGF that act on bone cells to promote osteolysis. Osteoblastogenesis is impaired by cell–cell contact mediated by VCAM-1 on MM cells and VLA-4 on osteoblast precursors and also by dysregulation of cell-surface coupling factors such as ephrinB2 and EphB4 on osteoblast precursors. Osteoclasts may form by MM cells fusing together or by dendritic cells fusing with osteoclast precursors, contributing to increased numbers of osteoclasts. Other cellular elements of BM, such as megakaryocytes, macrophages, and Th17 T lymphocytes, may also be cultivated by MM to promote bone disease (see text for details).