Abstract
To ascertain whether THA in patients with high dislocation after childhood sepsis would relieve pain and improve function, we assessed the rate of postoperative infection, improvement in Harris hip and WOMAC scores, and improvement in range of motion after the THA in 62 patients (62 hips) with high dislocation (Crowe Type 4) after childhood sepsis. The revision rate and the incidence of complications also were assessed. The mean age of the patients was 47.5 years. The minimum followup was 13 years (mean, 15.2 years; range, 13–17 years). One patient had persistent infection. The mean preoperative Harris hip score of 55 points improved to 89 points at the final followup, and the mean preoperative WOMAC score of 65 points improved to 42 points. The mean combined preoperative arc of range of motion of 197° improved to 275°. Four cups (6%) and three stems (5%) were revised. Complications developed in nine hips (15%), but the rate of infection was low. Improved surgical technique and design of components provided favorable results for total hip replacement performed for complications of childhood sepsis in these young and active patients.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Patients with high dislocation of the hip (Crowe Type 4) [6] secondary to childhood pyogenic arthritis have distinctive anatomic abnormalities that complicate THA. These include high-riding of the femoral neck stump relative to the normal location of the acetabulum, frequently severe soft tissue contractures resulting from prior infection and multiple surgeries, altered directions of abductor muscles, and altered locations of the femoral nerve, artery, and vein, and the profunda femoris artery. The key concerns in performing THA are the dysplastic acetabulum and femur, restoration of abductor function, and leg length. The shallow dysplastic acetabulum may require a small acetabular component of 40 mm or less. Narrowness of the femoral canal and increased anterior bowing of the proximal third of the femur make canal preparation difficult.
Hybrid or cemented THA or the first generation of cementless THA in patients with high dislocation has been associated with high complication and revision rates [6, 8, 10, 13, 14, 19, 23, 26, 27]. The rate of osteolysis has been reported between 13% and 58.5% with an average followup from 5.5 to 10.8 years [21, 22, 24, 27–30]. Dislocation rates of 3% to 18% [12–14, 17, 22], and revision rates of one or both components between 5% and 15% with average followup from 5.5 to 10.8 years have been reported [5, 9, 22, 24, 25].
The main goals of THA are pain relief and improvement in function. To ascertain whether THA was successful in patients with high dislocation (Crowe Type 4) after childhood sepsis we asked five questions: (1) whether recurrence of infection would be high; (2) whether Harris hip and WOMAC scores would improve; (3) whether preoperative range of motion (ROM) of the hip would improve and limb length would be restored; (4) whether the revision rate would be high; and (5) whether the complication rate would be high.
Materials and Methods
We retrospectively identified 80 patients with high dislocations of the hip (Crowe Type 4), presumably secondary to childhood pyogenic arthritis treated by THA between January 1990 and December 2000. Thirteen patients were excluded because we could not identify culture results to confirm pyogenic infection at the time of the remote septic arthritis. This left 67 patients for review. Of these, five patients were lost to followup 2 years after surgery. This resulted in 62 patients for review. The infecting organism of the original infection was Staphylococcus aureus in 53 patients (85%), Pneumococcus in three (5%), Hemophilus influenzae bacillus in three (5%), Salmonella in one (2%), meningococcus in one (2%), and Escherichia coli in one (2%). There were 22 men and 40 women, with a mean age of 47.5 years (range, 22–66 years). Their mean body mass index was 24.1 kg/m2 (range, 17.5–31.1 kg/m2). The minimum followup was 13 years (mean, 15.2 years; range, 13–17 years) (Table 1). The study was approved by our Institutional Review Board, and all patients provided informed consent.
Table 1.
Demographics of patients
| Parameters | Values |
|---|---|
| Gender (male/female) | 22/40 |
| Age (years) | 47.5 (range, 22–66; SD, 10.12) |
| Height (cm) | 157.5 (range, 141–175; SD, 7.65) |
| Weight (kg) | 59.7 (range, 41–90; SD, 10.15) |
| Body mass index (kg/m2) | 24.1 (range, 17.5–31.1; SD, 3.51) |
| Followup (years) | 15.2 (range, 13–17) |
SD = standard deviation.
The mean interval between resolution of active infection in the hip and THA was 37.8 years (range, 11–41 years). Limb-length discrepancy was measured before and after surgery using a tape measure from the anterior-superior iliac spine to the medial malleolus and a scanogram. Eight weeks before THA, aspiration was attempted in all patients. If no fluid was obtained from the joint, we performed washings with saline solution. A complete blood cell count and measurement of the erythrocyte sedimentation rate and C-reactive protein levels were performed preoperatively. Intraoperatively, we cultured aspirates, smears, and excised specimens for growth of aerobic, anaerobic, and tubercle bacilli. Frozen sections were performed intraoperatively on suspicious tissues. Granulation tissues with numerous acute inflammatory cells (more than five polymorphonuclear cells per high-power field), areas of necrosis, and presence or absence of an organism were assessed. Permanent histologic preparations stained with hematoxylin and eosin were examined for evidence of bacterial or tuberculous infection. If radiolucent areas were present on the preoperative radiographs, we performed an intraoperative biopsy for culture. During the operation, antibiotics were withheld until material from deep tissues had been obtained for culture and then cephalosporin (Cefazolin, DongA Pharmaceutical Company, Seoul, Korea, a daily dose of 4 g) was administered intravenously for 2 days. We did not consider the sensitivities of the previous pathogen to select antibiotics because the interval between infection and THA was long.
All operations were performed through a posterolateral approach. After clearing the pulvinar and fat from the true acetabulum, assessment was made of the available bone stock. This included palpation of the thickness of the anterior column between the index finger placed in the iliac fossa underneath the iliopsoas muscle and the thumb in the acetabular recess and by similar palpation of the thickness of the posterior column. We used the thickness of the anterior column to determine how much bone could be removed while still maintaining sufficient bone stock to provide integrity for the reconstruction. We began reaming with very small reamers (ie, 36 or 38 mm outer diameter), and carefully and gradually, the acetabular recess was enlarged to create a hemispheric recess as large as possible, fully containing the cementless acetabular component. If this was achieved, a standard technique was used to introduce the hemispheric porous-coated cementless acetabular component in the optional attitude of 45° abduction and 20° or 30° anteversion and to fix that acetabular component with screws. If we were not able to obtain an acetabular recess of sufficient volume to encompass an acetabular component of sufficient size, we followed these guidelines: After a trial acetabular component was placed in the true acetabulum after reaming of the acetabulum, the amount of posterosuperior segmental deficit with a lack of posterosuperior coverage of the component was estimated. If 60% of the porous surface was in contact with viable host bone and the acetabular component was rigidly fixed, allografting was not performed. If less than 60% of the porous surface was in contact with viable host bone, we performed a structural femoral head allograft. Forty hips (67%) required a structural allograft. The femoral head allograft was shaped to contour closely to the lateral portion of the wing of the ilium after exposure of that cortex stripping off the abductor muscles. Once the graft was fixed with two cancellous screws with bolts, additional reaming of the acetabular recess was able to establish continuity of the contour of the recess from the intact viable host bone to the adjacent graft. Finally, a cementless Duraloc 1200 series (DePuy, Warsaw, IN) acetabular component was press-fit after underreaming of the acetabulum 1 mm and multiple screws were inserted to augment the fixation. We used conventional ultrahigh-molecular-weight polyethylene (UHMWPE) made of ram-extruded 415 GUR in all hips. UHMWPE was irradiated and packaged in air. The inner diameter of the UHMWPE liner was 28 mm in all hips regardless of the external diameter of the acetabular component, which ranged from 48 mm to 58 mm.
Subtrochanteric segmental resection 3 to 5 cm in length was required to reduce the femoral head into the acetabular component in all hips. We used a cementless AML fully porous-coated stem (DePuy) with a 28-mm cobalt-chrome alloy femoral head in 59 hips and a 28-mm alumina-ceramic head was used in three hips. The AML femoral components were inserted with a press fit. Although all hips had altered anatomy, the bone quality was good in these young patients.
In all patients, preoperative and perioperative laboratory findings, including complete blood cell count, erythrocyte sedimentation rate, and C-reactive protein values, were within normal limits. Also, cultures for pyogenic bacteria and tubercle bacilli of preoperative aspirates were negative in all hips. The results of frozen sections that were performed intraoperatively and the permanent histologic sections were negative for bacterial or tuberculous infections and there were no inflammatory infiltrates suggestive of infection.
All patients were allowed to stand within 2 days and walk with partial weightbearing (50% of normal weightbearing) on crutches for 6 weeks followed by gradual return to full weightbearing. Clinical evaluations were performed using the Harris hip score [18] and the patient-assessed WOMAC [3] at 6 weeks, 3 months, 6 months, and 1 year after the operation and yearly thereafter. All patients were assessed at similar intervals. We assessed the level of activity of the patients after THA with the Tegner and Lysholm activity score [31]. This activity grading scale, which is used to numerically grade work and sports activities, was used as a complement to the functional score. The patients were given a score, according to the activities in which they engaged in daily life, ranging from 0 points for a hip-related disability to 10 points for participation in competitive sports at a national level.
A supine anteroposterior radiograph of the pelvis with both hips in neutral rotation and 0° abduction was obtained of every patient. Consistent patient positioning was ensured using a radiographic frame. This frame is constructed so it can be placed at the end of a standard radiograph table. Plastic polypropylene orthoses are secured to a plastic backboard through a vertical slot. A wing nut allows adjustment for the backboard through a vertical slot, and allows adjustment for various limb lengths. Rotation and abduction remain constant. Cross-table lateral radiographs also were obtained of each hip. Radiographic evaluations were done by one observer (SML) at each followup. We analyzed the radiographs at the final followup for the presence of radiolucent lines and osteolytic lesions around the acetabular component (in Zones I, II, and III according to the system of DeLee and Charnley [8]) and the femoral component (in Zones 1 through 14 according to the system of Gruen et al. [16]). Stability of the femoral component was classified as bone ingrown, stable fibrous ingrown, or unstable [11]. Fixation by bone ingrowth was defined as an implant with no subsidence and minimal or no radiopaque line formation around the stem. An implant was considered to have a stable fibrous ingrowth when no progressive migration but an extensive radiopaque line forms around the stem. An unstable implant was defined as one with definite evidence of either progressive subsidence or migration in the canal. We determined the percentage of host bone coverage of the acetabular component on anteroposterior and lateral radiographs of both hips. Loosening of the acetabular component was diagnosed when there was a change in the position of the component or a continuous radiolucent line that was greater than 2 mm wide on anteroposterior and lateral radiographs [12]. Osteolysis was defined as any discrete localized radiolucency that had been absent on radiographs obtained immediately after the THA. Heterotopic ossification was evaluated using the method of Brooker et al. [4].
We determined differences in continuous variances (Harris hip score, WOMAC score, range of motion, BMI) between preoperative and postoperative results using Student’s paired t-test, and in categorical variances (details of functional evaluation and deformity according to the Harris hip score) and limb-length discrepancies between preoperative and postoperative evaluations using chi square test. All statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS), version 14.0 (SPSS, Chicago, IL) using two Student’s two-tailed t tests and a significance level of α = 0.05. We used Kaplan-Meier curves in the analysis of the rate of survival of the prostheses with revision as the end point for failure [20], and the confidence interval at certain times was calculated with the formula of Greenwood [15].
Results
Recurrence of infection after THA in these patients was rare. The one hip that had an 8-year interval between infection and THA had recurrence of infection. The infecting organism during childhood was H. influenzae in this hip and it was Staphylococcus epidermidis, which was sensitive to methicillin after THA. Therefore, this hip had a new infection with no correlation with childhood sepsis.
Contemporary cementless THA with subtrochanteric segmental shortening in the patients with high dislocation of the hip (Crowe Type 4) secondary to childhood pyogenic infection resulted in improved pain (p < 0.001) and function scores (p < 0.001) at the latest followup. The total Harris hip score was 55 points (range, 31–72 points) preoperatively, which improved to 89 points (range, 30–100 points) at the latest followup (Table 2). Also, absence of deformity (fixed adduction deformity less than 10°, leg-length discrepancy less than 1.25 inches, and permanent flexion contracture less than 30°) and ROM of the hip (flexion contracture, abduction, external and internal rotation), except flexion improved (p = 0.0002 and p < 0.001, respectively) at the final followup (Table 2). The preoperative WOMAC score was improved (p = 0.023) at the final followup. The mean preoperative WOMAC score was 65 points (range, 58–70 points; standard deviation [SD], 5.7 points) and it was 42 points (range, 28–59 points; SD, 12.7 points) at the latest followup (Table 2).
Table 2.
Clinical and functional results of THA according to the Harris hip rating system [14]
| Followup | Pain | Function | Deformity | Range of motion (degrees) | Total hip score (points) | WOMAC score (points) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Pain | Gait | Support | Distance walked | Stairs | Socks/tie shoes | Sitting | Enter public transportation | Total | Absence of deformity | Permanent flexion | Flexion | Abduction | Adduction | External rotation | Internal rotation | ||
| Average | 19.7 | 0.7 | 10.4 | 7.5 | 1.9 | 2.7 | 4.9 | 0.8 | 28.9 | 2.7 | −13.5 | 94.8 | 21.0 | 32.2 | 27.4 | 21.6 | 55.4 | 65 |
| Minimum | 10 | 0 | 0 | 2 | 1 | 0 | 3 | 0 | 16 | 0 | −47 | 30 | −35 | 0 | 0 | −25 | 31 | 58 |
| Maximum | 24 | 5 | 11 | 11 | 4 | 4 | 5 | 1 | 41 | 4 | 5 | 135 | 60 | 60 | 60 | 100 | 72 | 70 |
| SD | 12.3 | 1.8 | 2.2 | 2.9 | 0.8 | 1.1 | 0.3 | 0.4 | 5.2 | 1.9 | 15.9 | 31.7 | 23.0 | 18.0 | 17.6 | 23.9 | 16.2 | 5.7 |
| Final followup | ||||||||||||||||||
| Average | 42.4 | 7.3 | 8.7 | 9.7 | 2.9 | 3.2 | 5.0 | 1.0 | 37.7 | 4.0 | 0.0 | 105.3 | 44.9 | 34.4 | 52.5 | 38.2 | 89.1 | 42 |
| Minimum | 10 | 0 | 0 | 2 | 0 | 0 | 5 | 1 | 11 | 4 | 0 | 40 | 20 | 10 | −20 | −20 | 30 | 28 |
| Maximum | 44 | 11 | 11 | 11 | 4 | 4 | 5 | 1 | 47 | 4 | 0 | 135 | 60 | 60 | 60 | 60 | 100 | 59 |
| SD | 6.3 | 3.0 | 4.1 | 2.7 | 1.5 | 1.4 | 0.0 | 0.0 | 11.0 | 0.0 | 0.0 | 21.4 | 10.4 | 11.2 | 16.6 | 22.4 | 14.9 | 12.7 |
| t test | < 0.001 | < 0.001 | 0.04 | 0.002 | 0.001 | 0.080 | 0.320 | 0.010 | 0.0001 | 0.0002 | < 0.001 | 0.113 | < 0.001 | 0.55 | < 0.001 | 0.004 | < 0.001 | 0.023 |
SD = standard deviation.
Ranges of motion had improved at final followup. The mean preoperative ROM were: flexion contracture, 13.5°; flexion, 94.8°; abduction, 21°; adduction, 32.2°; external rotation, 27.4°; and internal rotation, 21.6°. Mean ROM at the final followup were: flexion contracture, 0°; flexion, 105.3°; abduction, 44.9°; adduction, 34.4°; external rotation, 52.5°; and internal rotation, 38.2° (Table 2). The limb-length discrepancies were partly restored after surgery. Preoperative limb-length discrepancies by scanogram measurements ranged from 3 to 8 cm (mean, 4.5 cm). The mean limb-length discrepancy by scanogram measurements at the latest followup was 2.6 cm (range, 1.9–4.8 cm).
All but three patients had an activity score of 5 or 6 points. The remaining three patients had a score of 1 point because of their preexisting low back pain.
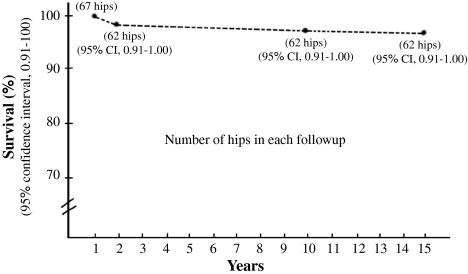
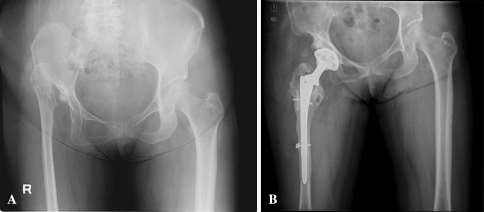
The 15-year survival rates of the acetabular and femoral components were 94% and 95% (95% confidence interval, 0.91–1.00), respectively (Fig. 1). Two hips (3%) had coverage of the acetabular component less than 60% by host bone. These hips had aseptic loosening of the acetabular component and were revised. One hip (1.6%) had septic loosening of the acetabular component. Two undersized femoral stems with aseptic loosening were revised with a larger Solution cementless femoral stem (DePuy). One femoral component (1.6%) had septic loosening and was revised. The remaining 59 femoral components were embedded solidly (Fig. 2). Femoral head allograft appeared well incorporated to host bone at the final followup. However, all 40 femoral head allografts were resorbed partially, yet partial resorption of the femoral head allograft did not jeopardize the structural integrity of the acetabular component. No hip had complete resorption of the femoral head allograft. Fifty-eight acetabular and 59 femoral components were fixed solidly in a satisfactory position (Fig. 2). A radiolucent line less than 1 mm was noted in Zone 1 of the acetabulum between the allograft-cup junction in 20 hips (32%) and in the Zones I and III in five hips (8%). The remaining 37 hips had no visible radiolucent line. We observed osteolyses in Zones I and/or II of the acetabulum in 38 hips that were between 0.5 cm2 and 1.2 cm2. In the femur, all osteolyses were located in Zones 1 and 7 of the femur, and were between 1 cm2 and 2.5 cm2. No hip had distal osteolysis.
Fig. 1.
The rate of survival of the components without removal or revision for any reason is shown. Recurrence of infection after THA in these patients was rare. Preoperative Harris hip score and WOMAC score improved at the latest followup and ROM and limb-length discrepancy improved at the final followup. Four cups (6%) and three stems (5%) were revised. Complications developed in nine hips (15%).
Fig. 2A–B.
(A) A preoperative anteroposterior radiograph of both hips of a 57-year-old woman shows an absent femoral head and neck with high dislocation of the greater trochanter and severe dysplastic acetabulum of the right hip and right pelvis. (B) The postoperative view obtained 10 years after surgery shows the Duraloc 1200 series cementless acetabular component is embedded well in a satisfactory position. There is a radiolucent line less than 2 mm in Zones I and III, but the acetabular component is solidly fixed. An AML femoral stem has osteolysis in Zones 1 and 7, but it is embedded solidly in a satisfactory position. The osteotomy site for subtrochanteric segmental resection is healed well.
Nine of 62 hips (15%) had complications. Peroneal nerve palsy occurred in two patients (3.2%) who had leg lengthening of 2.5 cm and 3 cm. Both patients had spontaneous resolution 1 year after the index operation. Three patients (4.8%) had dislocation of the femoral head. Two underwent closed reduction and wore an abduction brace for 3 months after which, there were no additional dislocations. One patient had a recurrent dislocation and the acetabular component was revised without additional recurrence. Three patients (4.8%) had linear calcar fractures that were fixed with a Dall-Miles cable (Howmedica, Rutherford, NJ). The fractures healed completely and osseous integration of the stem was achieved by the latest followup. One patient had skin-edge necrosis at the incision site. It healed well after débridement and closure.
Discussion
The main goals of THA are pain relief and improvement of function. To ascertain whether THA in patients with high dislocation after childhood sepsis would relieve pain and improve function of the hip, we questioned whether recurrence of infection would be high, whether Harris hip and WOMAC scores would improve, whether preoperative ROM would improve, and whether the revision and complication rates would be high.
There are some limitations of this study. First, the hip scoring system is prone to intraobserver variability. However, the chance-corrected kappa coefficient that was calculated to determine intraobserver agreement of hip scoring in this series was 0.71–0.82. Second, we have no interobserver variability and this can lead to bias in integrating radiolucent lines and loosening of the components. Although we have no interobserver variability, the chance-corrected kappa coefficient that was calculated to determine intraobserver agreement of radiographic measurements in this series was 0.75–0.86.
In a previous study [27], histopathologic examination of the operative specimens did not yield any evidence of bacterial infection in any of the patients, including one patient (two hips) who had subsequent reactivation of infection. Although no dormant bacilli were found in the two hips, histologic and bacteriologic sampling should be thorough and extensive to maximize the chances of identifying residual bacteria [27]. In another series [22], two of 47 hips (4%) underwent a resection arthroplasty because of persistent infection. In that series, the interval between active infection and THA in two hips was 7 years. It was recommended there be a period of absent infection more than 10 years before THA is performed [22]. In two other studies [21, 27], it also was recommended that the period of absent infection be more than 10 years before THA is performed. In the current series, one hip (2%) underwent resection arthroplasty because of persistent infection. Antibiotic-impregnated cement for femoral fixation may have been beneficial if the bacteria were sensitive to the antibiotics mixed in the cement.
In two previous studies [26, 27], preoperative pain and functional scores improved after THA in young, active patients with high dislocations of the hip (Crowe Type 4) after childhood pyogenic infection. In the studies of high dislocation of the hip after developmental dysplasia [2, 17, 22, 28], preoperative pain and functional scores were reported to have improved considerably after THA. In the current series, we observed preoperative pain and functional scores improved considerably after technically difficult THAs in young, active patients with high hip dislocation after childhood sepsis. Because of the extensive fibrosis and contracture of soft tissues from the previous infection and multiple operations (average incision and drainage of the hip was 3.5 times [range, 0–8 times]), the patients did not obtain as good a ROM as usual after THA. Nevertheless, the majority achieved functional improvement. Because of severe contracture of abductor muscles, it was very difficult to reduce the femoral head into the acetabular component fixed in the true acetabulum. All hips required stripping of the abductor muscles from the outer table of the ilium to release the contracted abductor muscles. However, no hip required abductor release at the iliac crest to bring the femoral head to the acetabular component.
In one study [7], aseptic loosening of the acetabular component occurred in 18 (11%) of the 162 hips with osteoarthrosis secondary to childhood pyogenic arthritis after an average of 10.8 years. In another, aseptic loosening of the acetabular component occurred in none of 24 hips with an average of 6.9 years followup after THA with a Harris-Galante porous-coated acetabular component (Zimmer, Warsaw, IN) to treat congenital dislocation of hips (Crowe Type 4) in patients who were on average 52 years old [1]. We had a revision rate of 5% (three of 62 hips). In another study, 18 (15%) of 123 hips had revision of both components because of aseptic loosening and/or osteolysis [27]. Use of undersized stems and poor-quality UHMWPE were thought to be factors in the failure of fixation of the components [27]. We revised two undersized stems (3%) because of aseptic loosening and one hip had both components revised because of infection. Therefore, the revision rate of the femoral stem in the current series was low because of satisfactory stem fill in the femoral canal. One hip required episiotomy of a severely hypoplastic femur to insert the smallest regular femoral component. This particular hip also had satisfactory stem fill in the femoral canal.
We identified osteolysis in 61% (38 of 62 hips). This rate is similar to the rate of 58.5% (72 of 123 hips) [27] but higher than the rate of 13% (30 of the 226 hips) reported in other studies [21, 24, 28–30]. It was suggested osteolysis was strongly associated with an increased rate of penetration of the acetabular UHMWPE liner [21, 24, 28–30]—a view we support.
The prevalence of nerve palsy is reportedly between 3% to 9% in series ranging from 23 to 66 THAs in patients who had congenital dislocation of the hip [2, 6, 22]. Peroneal nerve palsy occurred in one hip (0.8%) in a series of 123 THAs in patients who had childhood pyogenic arthritis [7]. Most peroneal nerve palsies resolved spontaneously 1 year after the index operation [7]. In the current series, peroneal nerve palsy occurred in two hips (3.2%). Both patients had spontaneous resolution of peroneal nerve palsies 1 year after the index operation. In these two patients, closed reduction of the hip was very difficult as a result of overzealous lengthening of the leg. Therefore, generous subtrochanteric resection and soft tissue release to reduce the femoral head into the acetabular component easily are mandatory to avoid nerve palsy.
Rates of dislocation of 3% to 11% have been reported among patients who had congenital dislocation of the hip [12–14, 17, 22]. In the current series, three hips (4.8%) dislocated within 3 months after the operation. Two patients were managed successfully with closed reduction and an abduction brace for 3 months. One patient required revision of the inadequate position of the acetabular component.
In one study [27], three femoral fractures (2% [three of 123 hips]) occurred in patients with high dislocation of the hip after childhood pyogenic arthritis. All fractures were at the middle level of the stem. The patients were seen within 7 months after the index operation and were treated successfully with open reduction and internal fixation. In another study [22], two hips (5% [two of 42 hips]) had a linear calcar fracture and these fractures were fixed with a Dall-Miles cable (Howmedica). The fractures in these hips healed completely and osseous integration of the stem was achieved at the latest followup. In the current study, three hips (4.8%) had linear calcar fractures and these fractures were fixed with a Dall-Miles cable. These three fractures healed completely and osseous integration of the stem was achieved at the latest followup. Difficulty often was encountered fitting the stem in the hypodysplastic femoral canal, which frequently fractured. Preoperative planning is important to select the correct size and type of prosthesis.
We recommend a bulk allograft if less than 60% of the acetabular component is covered by host bone, because two hips (3%) with less that 60% coverage of the acetabular component by host bone in the current series had aseptic loosening of the acetabular component and were revised. We believe the purpose of bone grafting, particularly in young patients, is not only to provide structural support to the acetabulum, but also to provide additional pelvic bone stock should subsequent revision become necessary.
Improved surgical technique and design of the cementless femoral and acetabular components provided a 15-year survival rate of the acetabular and femoral components of approximately 95% in young, active patients with technically difficult THAs. There was no recurrence of infection after THA in the patients in whom infection had been absent for more than 10 years.
Acknowledgments
We thank Sang-Mi Lee, BA, for radiographic evaluation and data analysis.
Footnotes
Each author certifies that he or she has no commercial association (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Anderson MJ, Harris WH. Total hip arthroplasty with insertion of the acetabular component without cement in hips with total congenital dislocation or marked congenital dysplasia. J Bone Joint Surg Am. 1999;81:347–354. doi: 10.2106/00004623-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Anwar MM, Sugano N, Masuhara K, Kadowaki T, Takaoka K, Ono K. Total hip arthroplasty in the neglected congenital dislocation of the hip: a five- to 14-year follow-up study. Clin Orthop Relat Res. 1993;295:127–134. [PubMed] [Google Scholar]
- 3.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 4.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement: incidence and method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 5.Chandler HP, Reineck FT, Wixson RL, McCarthy JC. Total hip replacement in patients younger than thirty years old: a five-year follow-up study. J Bone Joint Surg Am. 1981;63:1426–1434. [PubMed] [Google Scholar]
- 6.Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61:15–23. [PubMed] [Google Scholar]
- 7.Davlin LB, Amstutz HC, Tooke SM, Dorey FJ, Nasser S. Treatment of osteoarthrosis secondary to congenital dislocation of the hip: primary cemented surface replacement compared with conventional total hip replacement. J Bone Joint Surg Am. 1990;72:1035–1042. [PubMed] [Google Scholar]
- 8.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 9.Dorr LD, Takei GK, Conaty JP. Total hip arthroplasties in patients less than forty-five years old. J Bone Joint Surg Am. 1983;65:474–479. [PubMed] [Google Scholar]
- 10.Dunn HK, Hess WE. Total hip reconstruction in chronically dislocated hips. J Bone Joint Surg Am. 1976;58:838–845. [PubMed] [Google Scholar]
- 11.Engh CA, Jr, Culpepper WJ, 2nd, Engh CA. Long-term results of use of the anatomic medullary locking prosthesis in total hip arthroplasty. J Bone Joint Surg Am. 1997;79:177–184. doi: 10.1302/0301-620X.79B2.7640. [DOI] [PubMed] [Google Scholar]
- 12.Fredin H, Sanzen L, Sigurdsson B, Unander-Scharin L. Total hip arthroplasty in high congenital dislocation: 21 hips with a minimum five-year follow-up. J Bone Joint Surg Br. 1991;73:430–433. doi: 10.1302/0301-620X.73B3.1670444. [DOI] [PubMed] [Google Scholar]
- 13.Garcia-Cimbrelo E, Munuera L. Low-friction arthroplasty in severe acetabular dysplasia. J Arthroplasty. 1993;8:459–469. doi: 10.1016/S0883-5403(06)80017-3. [DOI] [PubMed] [Google Scholar]
- 14.Garvin KL, Bowen MK, Salvati EA, Ranawat CS. Long-term results of total hip arthroplasty in congenital dislocation and dysplasia of the hip: a follow-up note. J Bone Joint Surg Am. 1991;73:1348–1354. [PubMed] [Google Scholar]
- 15.Greenwood M. A report on the natural duration of cancer. The Series Report on Public Health and Medical Subjects. No 33. London, England: His Majesty’s Stationary Office; 1926:1–26.
- 16.Gruen TA, McNeice GM, Amstutz HC. ‘Modes of failure’ of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 17.Harley JM, Wilkinson JA. Hip replacement for adults with unreduced congenital dislocation: a new surgical technique. J Bone Joint Surg Br. 1987;69:752–755. doi: 10.1302/0301-620X.69B5.3316239. [DOI] [PubMed] [Google Scholar]
- 18.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 19.Hartofilakidis G, Stamos K, Ioannidis TT. Low friction arthroplasty for all untreated congenital dislocation of the hip. J Bone Joint Surg Br. 1988;70:182–186. doi: 10.1302/0301-620X.70B2.3346284. [DOI] [PubMed] [Google Scholar]
- 20.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 21.Kim Y-H. Total arthroplasty of the hip after childhood sepsis. J Bone Joint Surg Br. 1991;73:783–786. doi: 10.1302/0301-620X.73B5.1894666. [DOI] [PubMed] [Google Scholar]
- 22.Kim Y-H, Kim J-S. Total hip arthroplasty in adult patients who had developmental dysplasia of the hip. J Arthroplasty. 2005;20:1029–1036. doi: 10.1016/j.arth.2004.06.033. [DOI] [PubMed] [Google Scholar]
- 23.Kim Y-H, Kim J-S, Cho S-H. Primary total hip arthroplasty with a cementless porous-coated anatomic total hip prosthesis: 10-to 12- year results of prospective and consecutive series. J Arthroplasty. 1999;14:538–548. doi: 10.1016/S0883-5403(99)90074-8. [DOI] [PubMed] [Google Scholar]
- 24.Kim Y-H, Kim J-S, Cho S-H. A comparison of polyethylene wear in hips with cobalt-chrome or zirconia heads: a prospective, randomized study. J Bone Joint Surg Br. 2001;83:742–750. doi: 10.1302/0301-620X.83B5.10941. [DOI] [PubMed] [Google Scholar]
- 25.Kim Y-H, Kim VE. Results of the Harris-Galante cementless hip prosthesis. J Bone Joint Surg Br. 1992;74:83–87. doi: 10.1302/0301-620X.74B1.1732272. [DOI] [PubMed] [Google Scholar]
- 26.Kim Y-H, Kim VE. Uncemented porous-coated anatomic total hip replacement results at six years in a consecutive series. J Bone Joint Surg Br. 1993;75:6–13. doi: 10.1302/0301-620X.75B1.8421036. [DOI] [PubMed] [Google Scholar]
- 27.Kim Y-H, Oh S-H, Kim J-S. Total hip arthroplasty in adult patients who had childhood infection of the hip. J Bone Joint Surg Am. 2003;85:198–204. doi: 10.1302/0301-620X.85B2.13289. [DOI] [PubMed] [Google Scholar]
- 28.Mackenzie JR, Kelly SS, Johnston RC. Total hip replacement for coxarthrosis secondary to congenital dysplasia and dislocation of the hip: long-term results. J Bone Joint Surg Am. 1996;78:55–61. doi: 10.2106/00004623-199601000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Numair J, Joshi AM, Murphy JC, Porter ML, Hardinge K. Total hip arthroplasty for congenital dysplasia or dislocation of the hip: survivorship analysis and long-term results. J Bone Joint Surg Am. 1997;79:1352–1360. doi: 10.2106/00004623-199709000-00009. [DOI] [PubMed] [Google Scholar]
- 30.Sochart DH, Porter ML. The long-term results of Charnley low-friction arthroplasty in young patients who have congenital dislocation, degenerative osteoarthritis, or rheumatoid arthritis. J Bone Joint Surg Am. 1997;79:1599–1617. doi: 10.2106/00004623-199711000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]