Abstract
Precise evaluation of acetabular cup version is necessary for patients with recurrent hip dislocation after THA. We retrospectively studied 42 patients, who underwent THAs, with multiple cross-table lateral radiographs and CT scans to determine whether radiographic or CT measurement of acetabular component version is more accurate. One observer measured cup version on all radiographs. CT scans were interpreted by one observer. Twenty radiographs were measured twice each by two observers to determine intraobserver and interobserver reliability. We implanted cups in four model pelvises using navigation and compared measurements of anteversion made with radiographs and CT scans. Intraclass correlation coefficients (ICC) for anteversion measurements of two observers were 0.9990 and 0.9998, respectively, when comparing measurements of identical radiographs (intraobserver). Paired values for two observers measuring the same radiograph had an ICC of 0.9686 (interobserver) compared with 0.7412 for measurements from serial radiographs of the same component. The ICC comparing radiographic versus CT-based measurements was 0.6981. CT measurements had stronger correlations with navigated values than radiographic measurements. Accuracy of anteversion measurements on cross-table radiographs depends on radiographic technique and patient positioning whereas properly performed CT measurements are independent of patient position.
Level of Evidence: Level III, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Correct anteversion of the acetabular component in THA is essential for prosthetic stability [17, 21, 28] and to minimize wear [13, 15, 30]. Anteversion has been defined in relation to different planes and landmarks, giving rise to the terms true (anatomic) anteversion, planar (radiographic) anteversion, and operative anteversion. True anteversion is the angle between the projection of the acetabular axis onto the transverse plane and the left-right axis, planar anteversion is the angle between the acetabular axis and the coronal plane, and operative anteversion is the angle between the projection of the acetabular axis onto the sagittal plane and the cranial-caudal axis [1, 24, 33]. Planar anteversion is the form discussed in this article. Anteversion can be measured from standardized anteroposterior (AP) views [11, 27, 31] or, most commonly, from cross-table lateral radiographs [33].
A cross-table lateral radiograph is difficult to obtain owing to the necessity and potential discomfort of flexing the contralateral hip, the possibility of pelvic flexion or extension, which will affect the apparent version of the cup, and uncertainty regarding the exact location of the cup position when centering the xray beam. Additionally, ideal inclination of the beam will vary with each patient depending on the inclination of the cup [6, 10, 33]. Despite these potential sources for inaccuracy, cross-table lateral radiographs are widely used for evaluation of version and continue to be used as sole measures of anteversion [5, 25, 29]. The previously mentioned sources of inaccuracy are mitigated when version is calculated using CT scans, specifically those related to patient positioning and centering of the beam [22]. Instead of requiring an individualized optimal beam orientation to best evaluate the position of the cup, evaluation of version with CT scans requires reformatting to provide views of the acetabular cup in the appropriate planes.
We addressed four questions: (1) What is the variation in the measurements of version from film to film on sequential cross-table lateral radiographs in patients with well-fixed components? (2) What are the intraobserver reliability and interobserver reliability of radiographic measurements of version? (3) Are version measurements obtained from radiographs and CT scans of the same patients similar? (4) How will radiographic and CT measurements of version compare in an in vitro scenario with no variability of pelvic tilt and/or rotation?
Materials and Methods
We retrospectively reviewed radiographs and CT scans of 51 patients who had undergone THA. Patients were eligible for inclusion in this study if they had a radiographically well-fixed THA. The patients eligible for the study were those scheduled for routine followups during a 3-week period with one senior arthroplasty surgeon not otherwise involved with the study. In addition, a selected group of patients who underwent cross-table radiographs and CT scans for evaluation of recurrent hip instability were included. Radiographic fixation was determined by an arthroplasty surgeon (AGDV) who had not been involved in the surgeries. Eligible patients were included only if they had multiple cross-table lateral radiographs available with no interval surgeries or had at least one cross-table lateral radiograph and a CT scan (performed to evaluate version) within 2 years of each other with no interval surgeries. The study was approved by our Institutional Review Board.
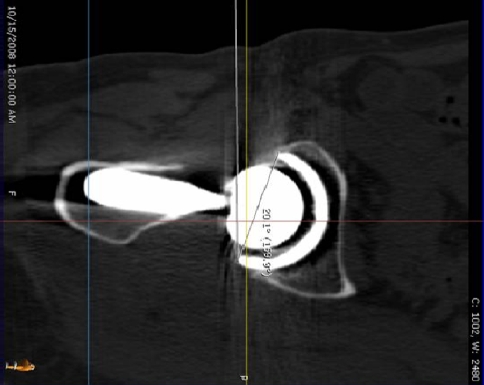
All standardized cross-table radiographs and CT scans were performed by the same group of radiology technicians. The CT scans were interpreted by a specialized musculoskeletal radiologist (BG) according to a preestablished protocol using 1-mm CT cuts reformatted using software accompanying the IDT 16 detector Phillips multislice CT (Phillips Healthcare, Andover, MA). First, the position of the pelvis is standardized for rotation and pelvic tilt by reformatting the image to make the plane defined by the posterior border of the distal sacrum and the posterior border of the ischium horizontal. Second, a plane orthogonal to the line drawn from the most medial point of the cup to the most lateral point of the cup is created. Images in this plane, which differs from a parasagittal plane by the angle of inclination, allow for measurement of cup anteversion regardless of the degree of inclination by referencing off a vertical line (Fig. 1). Prior studies have confirmed CT as an accurate method to determine anteversion of acetabular cups after THA [22, 27]. In addition, the CT scan provided measurement of femoral stem version that was not used for this study.
Fig. 1.
A reformatted CT scan shows the angle used to determine acetabular cup version.
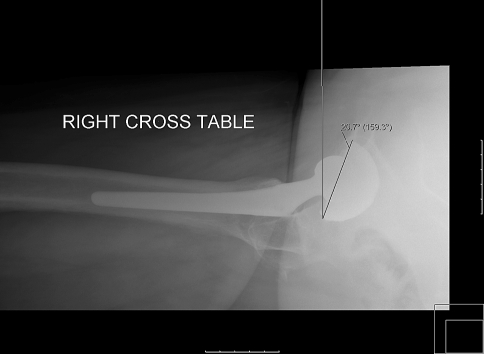
The version of the acetabular component on cross-table lateral radiographs was the angle formed by the long axis of the ellipsoid projection of the cup base and a vertical line on the film (Fig. 2). The long axis of the cup is a line connecting the most superior with the most inferior points of the ellipse formed by the base of the cup. If the beam is directed along the base of the cup, the ellipsoid projection becomes a straight line (when minor axis collapses to zero) and the angle this makes with a vertical line then is measured as the version. These angles were measured using the Eisenlohr X-Caliper® device (Eisenlohr Technologies, Davis, CA), which provides measurements to a tenth of a degree.
Fig. 2.
A cross-table lateral radiograph shows measurement of the acetabular cup version.
One observer (CKK) measured 84 cross-table radiographs from the 42 patients included in the study (Table 1). For patients with more than two cross-table radiographs, the two most recent radiographs were used. In addition, 20 randomly selected cross-table lateral radiographs were measured four times, in a nonsupervised fashion, by two observers: a fourth-year orthopaedic surgery resident (CKK) and a fully trained orthopaedic surgeon (AGDV). Two separate measurements for each radiograph were made by each observer in two reading sessions 1 month apart to evaluate intraobserver and interobserver reliability (Table 2). We compared the anteversion measurements from radiographs and CT scans (Table 3) and calculated Pearson’s correlation coefficient of the paired data points (radiograph vs CT).
Table 1.
Measurements of cup version for patients with two or more cross-table lateral radiographs
| Patient | Cup version (degrees) | ||
|---|---|---|---|
| Radiograph 1 | Radiograph 2 | Range | |
| 1 | 23.1 | 19 | 4.1 |
| 2 | 33.2 | 55.4 | 22.2 |
| 3 | 22 | 10.9 | 11.1 |
| 4 | 30.5 | 20.4 | 10.1 |
| 5 | 23.1 | 29.9 | 6.8 |
| 6 | 15.8 | 9.5 | 6.3 |
| 7 | 31.8 | 23.1 | 8.7 |
| 8 | 31.6 | 39.1 | 7.5 |
| 9 | 1.3 | 3.1 | 1.8 |
| 10 | 21.2 | 17.4 | 3.8 |
| 11 | 25.9 | 26.7 | 5.3 |
| 12 | 11.4 | 10.6 | 0.8 |
| 13 | 14.8 | 18 | 3.2 |
| 14 | 37.6 | 27.6 | 10 |
| 15 | 24.7 | 33.3 | 8.6 |
| 16 | 26.5 | 19 | 7.5 |
| 17 | 27.7 | 28 | 0.3 |
| 18 | 22.5 | 20.9 | 1.6 |
| 19 | 18.9 | 16.6 | 2.3 |
| 20 | 34 | 27.8 | 6.2 |
| 21 | 21.5 | 21.5 | 0 |
| 22 | 8.3 | 14.3 | 6 |
| 23 | 41.4 | 39.5 | 1.9 |
| 24 | 24.1 | 14 | 10.1 |
| 25 | 30.6 | 30.7 | 0.1 |
| 26 | 20.1 | 5 | 15.1 |
| 27 | 36.1 | 43 | 6.9 |
| 28 | 27.6 | 26.4 | 1.2 |
| 29 | 23.3 | 19.8 | 3.5 |
| 30 | 26.2 | 15.6 | 10.6 |
| 31 | 45.3 | 35.2 | 10.1 |
| 32 | 41.1 | 24.6 | 16.5 |
| 33 | 35.3 | 22 | 13.3 |
| 34 | 46.6 | 33.2 | 13.4 |
| 35 | 35.4 | 33.6 | 1.8 |
| 36 | 23.3 | 19.8 | 3.5 |
| 37 | 12.7 | 24.8 | 12.1 |
| 38 | 34.3 | 32.2 | 2.1 |
| 39 | 26.5 | 15.4 | 11.1 |
| 40 | 0.2 | 7.8 | 7.6 |
| 41 | 17.6 | 20.3 | 2.7 |
| 42 | 11.5 | 5.7 | 5.8 |
All angles are presented with the convention that positive values indicate anteversion and negative values indicate retroversion.
Table 2.
First and second measurements of cup version on cross-table lateral radiographs
| Radiograph | Cup version (degrees) | |||
|---|---|---|---|---|
| Observer 1 | Observer 2 | |||
| First | Second | First | Second | |
| 1 | 14.1 | 15.1 | 13.7 | 13.8 |
| 2 | 38.5 | 38.8 | 38.9 | 39.3 |
| 3 | 26 | 25.9 | 27.6 | 28.5 |
| 4 | 17.7 | 18 | 20 | 19.8 |
| 5 | 4.8 | 4.9 | 4.7 | 4.4 |
| 6 | 6.4 | 6.6 | 7.7 | 7.4 |
| 7 | 32.5 | 31.6 | 37 | 35.8 |
| 8 | 33.9 | 34.3 | 37.8 | 36.9 |
| 9 | 41.1 | 41.4 | 38.4 | 38.7 |
| 10 | 34.6 | 34.8 | 45.9 | 45.3 |
| 11 | 29.7 | 31.2 | 36.1 | 35.3 |
| 12 | 28.9 | 28.7 | 33.1 | 33.5 |
| 13 | 10.4 | 11 | 12.6 | 12.2 |
| 14 | 0.2 | 0.4 | 0.3 | 0.4 |
| 15 | 7 | 7.3 | 7 | 6.9 |
| 16 | 25.9 | 26 | 28.3 | 28.3 |
| 17 | 13.5 | 13.2 | 15 | 15.4 |
| 18 | 15.1 | 15.6 | 17.3 | 17.8 |
| 19 | 16.9 | 16 | 19.1 | 18.3 |
| 20 | 6.2 | 6.2 | 7.6 | 7.5 |
Table 3.
Comparison of cup version measurements in 15 paired CT and cross-table lateral radiographs
| Patient | Cup version (degrees) | ||
|---|---|---|---|
| Cross-table | CT | Difference | |
| 1 | 51.2 | 31 | 20.2 |
| 2 | 33.6 | 20 | 13.6 |
| 3 | 45.3 | 28 | 17.3 |
| 4 | 32.5 | 30 | 2.5 |
| 5 | 53.4 | 28 | 25.4 |
| 6 | 29 | 9 | 20 |
| 7 | 52.6 | 44 | 8.6 |
| 8 | 3.8 | −13 | 16.8 |
| 9 | 5 | 0 | 5.0 |
| 10 | 34 | 27 | 7.0 |
| 11 | 21.5 | 20 | 1.5 |
| 12 | 8.3 | 19 | −10.7 |
| 13 | 41.4 | 39 | 2.4 |
| 14 | 14 | 15 | 1.0 |
| 15 | 30.6 | 29 | 1.6 |
All angles are presented with the convention that positive values indicate anteversion and negative values indicate retroversion.
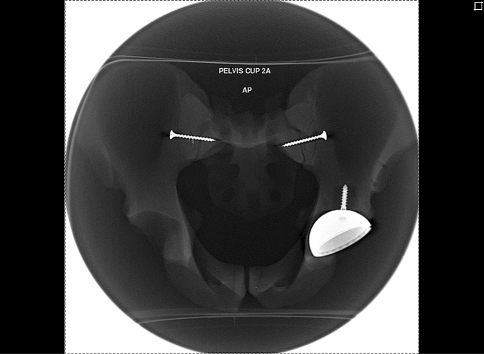
To control for pelvic tilt and rotation that may introduce variability in the measurements, we conceived the following in vitro scenario: Four Sawbones® pelvises (Pacific Research Labs, Inc, Vashon, WA) were fixed with the ischial tuberosities and the coccyx firmly secured to a base. Using the Smith and Nephew IntraOperative Navigation™ system (Smith and Nephew, Inc, Memphis, TN), all four Sawbones® pelvises underwent left acetabular component placement with screw fixation to ensure maintenance of cup position during the experiment (Fig. 3). A range of inclination values and version values were used (Table 4) and recorded. After recording version and inclination values, the pelvises underwent plain radiography and CT. Two serial cross-table lateral radiographs (Fig. 4) were taken by each of two radiology technicians who were blinded to the cup position but could position the pelvises based on the anterior-superior iliac spine, a common landmark used in patients. Cup version on radiographs and CT scans then were measured in a blinded manner by two observers (CKK, AGDV) and a musculoskeletal radiologist (BG), respectively, using the techniques previously described.
Fig. 3.
An AP radiograph was obtained of a model pelvis after performing navigated placement of the left acetabular cup.
Table 4.
Cup version measurements for Sawbones® pelvises scans
| Pelvis | Cup version (degrees) | Navigated abduction (degrees) | |||||
|---|---|---|---|---|---|---|---|
| Navigated value | Attending: Tech 1 | Attending: Tech 2 | Resident: Tech 1 | Resident: Tech 2 | CT scan | ||
| 1 | 10 | 6 | 7.6 | 5.2 | 3 | 3.5 | 45 |
| 2 | 19 | 10.8 | 7 | 8.5 | 7 | 10 | 31 |
| 3 | −12 | −23.5 | −25.4 | −22.7 | −26.1 | −17.6 | 47 |
| 4 | 0 | −13.5 | −10.8 | −6.8 | −7.4 | −5.9 | 53 |
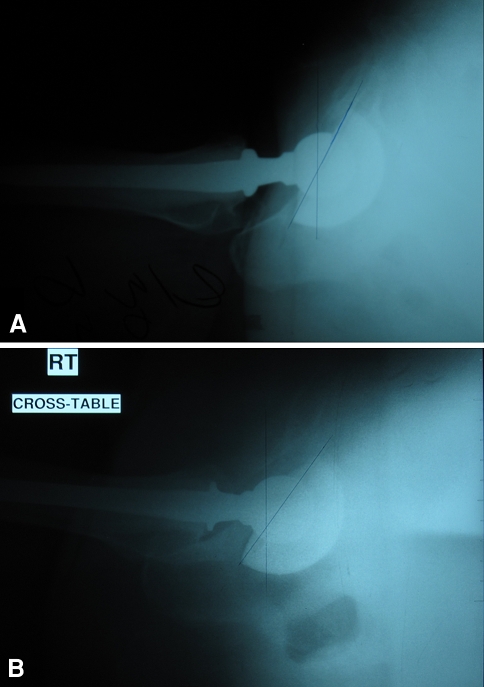
Fig. 4.
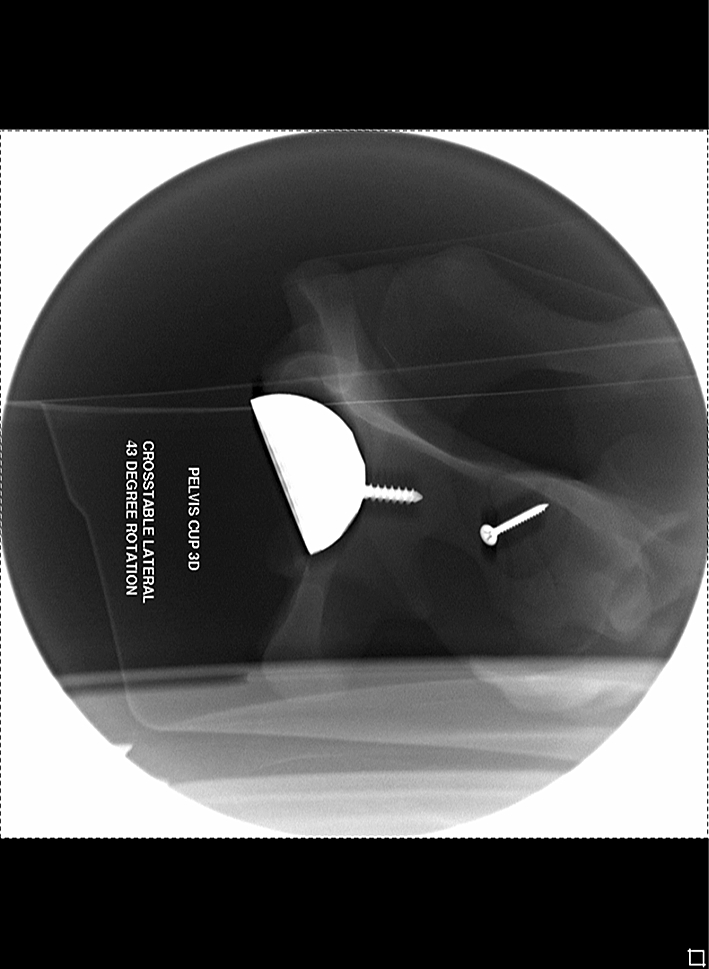
This cross-table lateral radiograph of a model pelvis after navigated placement of the left acetabular cup shows apparent retroversion of the cup.
Based on the radiographic measurements of version, we calculated the ICC which provides information regarding the global agreement between measurements made on multiple cross-table lateral radiographs of the same acetabular component and describes interobserver and intraobserver reliability. Agreement of version measurements obtained from the radiographs and CT scans was calculated as the difference between the paired measurements and using Pearson’s correlation coefficient. Finally, version measurements from radiographs and CT scans in our in vitro experiment that controlled for pelvic tilt and rotation were compared using ICC. The ICC values were graded using previously described semiquantitative criteria [23]: excellent for a p value of 0.90 to 1.0, good for 0.70 to 0.89, fair/moderate for 0.50 to 0.69, low for 0.25 to 0.49, and poor for 0.0 to 0.24. Statistical analysis was performed with SPSS® software (SPSS Inc, Chicago, IL).
Results
We found a substantial difference in the measurements of serial radiographs for the same patient made by one observer. Among the 42 patients measured, a difference of 10° or greater was detected in 12 (28%) (Fig. 5; Table 1). The ICC comparing each measurement was 0.7412 with a 95% confidence interval for measurement error of ± 7.3°, meaning an isolated radiographic anteversion measurement of 10º has a true value between 2.7º and 17.3º with 95% confidence.
Fig. 5A–B.
The measured anteversion of the two serial cross-table lateral radiographs of the same patient with well-fixed components and no interval surgeries are (A) 27.6° and (B) 37.6°.
The ICCs for serial measurements of the same radiographs were 0.9990 and 0.9992 for the two measuring physicians separately (intraobserver reliability), with a 95% confidence interval for measurement error attributable to variation by one observer of 0.54° (Table 2). Paired values for two observers measuring the same radiograph had an ICC of 0.9686 (interobserver reliability), with a 95% confidence interval for measurement error attributable to variation between observers of 3.2° (Table 2).
Measurements of version on radiographs correlated (ICC = 0.69) with those on CT (Table 3). The radiographs averaged 8.7° more anteversion (range, 10.7° less anteversion to 25° more anteversion) than the CT measurements.
Measurements of version in the in vitro experiment correlated (ICC = 0.862) with those on CT scans and radiographs (ICC for each observer 0.779 and 0.786) (Table 4).
Discussion
Cup version can affect the stability of a THA [4, 6]. Several studies have established guidelines for a safe zone of cup anteversion that surgeons strive to stay within [2, 17, 21]. A precise, reliable measure is necessary for clinical, research, and medicolegal reasons, particularly in the unfortunate event that a patient experiences a dislocation and a decision is made to perform revision surgery. Cross-table radiographs traditionally have been used for measurement of cup version, as plain film is relatively inexpensive and has the benefit of ease of interpretation without need for reformatting or digital manipulation of the images. We acknowledge radiographs are an attractive modality for characterization of component position owing to their ubiquity, low radiation exposure, and low cost; however, concerns regarding accuracy, repeatability, and the inability to evaluate the femoral component using standard radiographs are substantial limitations. Although convenient, consistent cross-table lateral radiographs are difficult to obtain for the reasons described above, leading us to evaluate the precision and accuracy of radiographic measurements. We therefore sought to (1) describe the variation in the measured version angles on sequential cross-table lateral radiographs in the same patient, (2) determine the intraobserver and interobserver reliability of radiographic measurements of version, (3) compare measurements obtained from radiographs and CT scans, and (4) determine which study would provide the most accurate measurement in an ideal, in vitro scenario which controlled for pelvic tilt and rotation.
There are limitations to our study. First, there is no gold standard that can be used to validate radiographic or CT-based values in vitro or in vivo. CT, however, can be considered an acceptable standard for measurement owing to control over pelvic rotation and/or tilt. Second, intraoperative measures of version were shown to be inaccurate [21], and were not recorded for this cohort of patients. Third, we did not perform multiple CT scans on the same patients because of concern for radiation exposure; thus, we have no repeatability data for the CT scans with which we can compare the cross-table lateral radiograph repeatability data. Fourth, there is an intrinsic error in measurements based on computer navigation [2, 8, 21], which we used as a third measure of anteversion to compare with CT-derived values. To diminish error, navigated cup placement was performed by one operator under ideal in vitro conditions. Additionally, we thought these values have relevance to our study as navigated values reference from extraarticular landmarks in the pelvic bony anatomy (pubic tubercles and anterior-superior iliac crests) to set a reference plane for the pelvis, similar to the manner in which CT measurements are taken, and thus should be independent of the position of the pelvis. Finally, because the tangent to the face of an acetabular cup changes with inclination, the xray beam angle for optimal cross-table lateral radiographs will change with cup inclination, a factor not likely considered when radiographs are obtained. The protocol at our institution for obtaining cross-table lateral radiographs dictates a cephalad beam angle of 45° respective to the transverse plane with the hip in question farthest from the beam. This is most appropriate for inclinations of 45°, and less optimal radiographs will be obtained when inclination varies. Although 45° inclination is within the safe range identified by Lewinnek et al. [17], Hassan et al. [11] and Wines and McNicol [32] reported approximately 40% of THAs considered by surgeons to fall within this 20° safe range were, in fact, outside. Standard radiographs taken with a standard cephalad tilt are not optimal for all THAs. Although intensive training of radiology technicians to customize radiographs based on component position and patient factors may improve these results, this has not yet been explicitly attempted and would involve considerable time and cost. In our institution, there has been a trend to evaluate cup version using CT. CT is readily available in most institutions and the potential differential charge ($1442 for CT versus $648 for radiographs in our institution) may be offset by an improved ability to discern acetabular component malposition and to evaluate the version of the femoral stem, which is not possible using radiographs. Final cost effectiveness, however, cannot be determined based on the current study nor have other studies attempted to address this question.
As the acetabular components had not migrated in the interval between studies, one would expect measurements made from serial radiographs obtained by the same group of radiology technicians would be similar. In this case, the ICC should approach 1.0, not including allowances made for measurement error and operator error. As can be seen from the interobserver and intraobserver reliability data, the measurement error is relatively small compared with the error seen on serial radiographs of the same acetabular component: 0.97, which represents excellent agreement between different observers, versus 0.74, which represents only good agreement for measurement of serial radiographs. We found high interobserver reliability for radiographic measurement of cup position, a finding that was observed in other studies of anteversion measured from radiographs (Table 5). Measurement error makes up only a small amount of the difference seen between measurements of serial radiographs. In a comparison of alternate methods of measuring anteversion, Arai et al. [3] described the relationship between version measured from cross-table radiographs and values using AP radiographs of the hip using the method of Lewinnek et al. [17]. Arai et al. [3] described a systematic bias in the measurement of version using cross-table lateral radiographs in patients with a stiff contralateral hip presumably because efforts to flex the stiff contralateral hip tended to flex the pelvis. Although they pointed out a limitation to cross-table lateral radiographs, they did not describe variation in serial radiographs of the same patient, only variation between patients attributable to one particular patient characteristic, and provide no interobserver or intraobserver analysis. Kalteis et al. [14], although describing the accuracy of anteversion measurements from AP radiographs compared with CT instead of cross-table lateral radiographs, did present interobserver and intraobserver analysis (Table 5), and a discussion of inability to control pelvic tilt as a major limitation of radiographic anteversion measurements.
Table 5.
Reported interobserver reliability for radiographic version measurements*
| Study | Measurement compared across different observers | ICC for interobserver reliability | Mean measurement error ± SD for interobserver reliability |
|---|---|---|---|
| Hassan et al. [10] (1995) | Anteversion from AP radiographs of ex vivo cup | 0.97–0.99 | |
| Current study | Anteversion from cross-table lateral radiograph | 0.9686 | |
| Kalteis et al. [14] (2006) | Anteversion from AP pelvis radiograph | 2.3º ± 2.3º | |
| Liaw et al. [18] (2006) | Anteversion from AP pelvis radiograph | 1.0º ± 0.7º | |
| Liaw et al. [19] (2008) | Anteversion from AP pelvis radiograph | 0.5º ± 0.7º | |
| Hayakawa et al. [12] (2008) | Anteversion from AP pelvis radiograph | 1.4° ± 3.1° | |
| Current study | Anteversion from cross-table lateral radiograph | 2.4º ± 2.4º |
* Several studies have commented on the reliability of the measurement of anteversion using either AP or cross-table lateral radiographs; ICC = intraclass correlation coefficient; SD = standard deviation; AP = anteroposterior.
Notable differences exist between the CT and radiograph measurements of version. Although there is no gold standard to validate either measurement method, the discrepancy between CT and cross-table lateral films casts doubt on the radiographic measurements, given the low ICC for serial plain film measurements discussed above and correction of pelvic tilt and rotation using reformatted CT. Mian et al. [22] provided an early description of using CT after THA to measure acetabular component anteversion. Although describing their method of anteversion calculation using CT as “highly accurate” based on an in vitro model, they provided no data to support this claim. In an experiment similar to ours, Marx et al. [20] evaluated anteversion values measured from AP radiographs using several techniques in comparison to CT-based values and reported considerable difference between CT-based and radiograph-based values, with the radiographs tending to underestimate the anteversion by between 6° and 14°. Like the current study, that study had no gold standard and thus was able to comment only on differences between measurement methods, not on improved accuracy of one method over another because of this limitation.
We designed an experiment in which acetabular components were fixed in model pelvises and imaged in a standard position using CT scans and radiographs. Version and inclination values determined using the navigation software were recorded based on a pelvic reference plane and compared with radiographic and CT-based measurements. There is published evidence regarding the accuracy of navigated cup placement. Dorr et al. [7] studied blinded surgeon estimates and computer-navigated values of cup placement compared with postoperative CT scans and found computer-navigated values were more precise than surgeon estimates. Precision in the computer-navigated anteversion values was approximately three times better than precision seen in the estimate of cup anteversion made by an experienced surgeon in that study. Similarly, Nogler et al. [26] and Haaker et al. [9] studied conventional cup placement with navigated cup placement via postoperative CT scanning. With surgeons in both studies attempting to place the acetabular component with 45° abduction and 20° anteversion, these studies also showed cups placed with computer navigation were more accurately placed, had lower standard deviations, and had fewer outliers. In our experiment several conditions mitigate factors described as compromising navigated results in vivo. In particular, we assume landmark identification and landmark registration errors would be less in our study compared with in vivo scenarios where the presence of soft tissues may interfere with these processes. Additionally, the standardization of dimensions in manufactured artificial pelvises eliminates concerns about compensating for differential pelvic tilt as described by Dorr et al. [7] and Lembeck et al. [16]. Comparisons of measurements from radiographs and CT scans with navigated values were performed in absolute terms and using Pearson’s correlation coefficient, which helps to eliminate biases that could come from differing definitions of anteversion. Statistical analysis of these measurements suggests CT measurement is more accurate than the radiographic measurements from either observer. Correlation between CT measurements and radiographic measurements was only moderate and the ICC between navigated values and CT measurements was greater than those of radiographic measurements from either observer (0.862 versus 0.779 and 0.786).
Evaluation of cup version is performed routinely by many surgeons after THA and is indicated for all patients who have experienced a dislocation. Measurement of the version of the acetabular component using CT has several advantages. The measurement is not dependent on patient position and a CT scan is more comfortable for the patient as the opposite extremity does not have to be elevated. The version of the cup can be compared with version of the anatomic acetabular cavity in cases of unilateral arthroplasty. The position of the cup can be assessed in relation to the entire pelvis, giving information about pelvic tilt, which is assumed to be standard in cross-table lateral radiographs. Finally, femoral component version, which can be the cause of recurrent dislocation, can be accurately measured via comparison with the knee epicondylar axis, preparing the surgeon to perform a femoral component revision if retroversion is encountered. Although a cross-table lateral radiograph is easily obtained and inexpensive, serial cross-table radiographs in well-fixed acetabular components showed substantial differences in version. We believe higher correlations between computer-navigated version measurements and CT-based measurements when compared with measurements taken from cross-table lateral radiographs supports use of CT scans over cross-table radiographs when a precise measurement of cup version is needed. Obtaining a CT scan to evaluate component version is especially important in patients with recurrent dislocation in which revision surgery is indicated and the surgeon must decide on different surgical plans. Information provided by CT can help identify patients who will benefit from retaining the acetabular shell and changing the insert geometry and/or the head diameter and others that may require revision and reorientation of a well-fixed shell. Although cost considerations and radiation exposure may prohibit use of CT-based measurements on a routine basis, the surgeon and researcher should be aware of the limitations and variability of radiographic measurements. We recommend use of CT scans when planning revision surgery for a patient with recurrent dislocations after THA where accurate characterization of acetabular and femoral implant positions is critical for decision making.
Acknowledgments
We thank Dr. Thomas P. Sculco for allowing use of his patients in this study, Clara Hilario for assistance in the computer navigation laboratory, and Gregory Schack of Smith and Nephew for donating the computer navigation system and acetabular components used in the study.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ackland MK, Bourne WB, Uhthoff HK. Anteversion of the acetabular cup. J Bone Joint Surg Br. 1986;68:409–413. doi: 10.1302/0301-620X.68B3.3733807. [DOI] [PubMed] [Google Scholar]
- 2.Ali Khan MA, Brakenbury PH, Reynolds IS. Dislocation following total hip replacement. J Bone Joint Surg Br. 1981;63:214–218. doi: 10.1302/0301-620X.63B2.7217144. [DOI] [PubMed] [Google Scholar]
- 3.Arai N, Nakamura S, Matsushita T. Difference between 2 measurement methods of version angles of the acetabular component. J Arthroplasty. 2007;22:715–720. doi: 10.1016/j.arth.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 4.Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stockl B. Reducing the risk of dislocation after total hip arthroplasty. J Bone Joint Surg Br. 2005;87:762–769. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 5.Calvert GT, Devane PA, Fielden J, Adams K, Horne JG. A double-blind, prospective, randomized controlled trial comparing highly cross-linked and conventional polyethylene in primary total hip arthroplasty. J Arthroplasty. 2008 Jun 9. [Epub ahead of print]. [DOI] [PubMed]
- 6.D’Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW., Jr The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315–332. doi: 10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Dorr LD, Malik A, Wan Z, Long WT, Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res. 2007;465:92–99. doi: 10.1097/BLO.0b013e3181560c51. [DOI] [PubMed] [Google Scholar]
- 8.Goergen TG, Resnick D. Evaluation of acetabular anteversion following total hip arthroplasty: necessity of proper centering. Br J Radiol. 1975;48:259–260. doi: 10.1259/0007-1285-48-568-259. [DOI] [PubMed] [Google Scholar]
- 9.Haaker RG, Tiedjen K, Ottersbach A, Rubenthaler F, Stockheim M, Stiehl JB. Comparison of conventional versus computer-navigated acetabular component insertion. J Arthroplasty. 2007;22:151–159. doi: 10.1016/j.arth.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 10.Hassan DM, Johnston GH, Dust WN, Watson LG, Cassidy D. Radiographic calculation of anteversion in acetabular prostheses. J Arthroplasty. 1995;10:369–372. doi: 10.1016/S0883-5403(05)80187-1. [DOI] [PubMed] [Google Scholar]
- 11.Hassan DM, Johnston GH, Dust WN, Watson G, Dolovich AT. Accuracy of intraoperative assessment of acetabular prosthesis placement. J Arthroplasty. 1998;13:80–84. doi: 10.1016/S0883-5403(98)90079-1. [DOI] [PubMed] [Google Scholar]
- 12.Hayakawa K, Minoda Y, Aihara M, Sakawa A, Ohzono K, Tada K. Acetabular component orientation in intra- and postoperative positions in total hip arthroplasty. Arch Orthop Trauma Surg. 2008 Apr 22. [Epub ahead of print]. [DOI] [PubMed]
- 13.Hirakawa K, Mitsugi N, Koshino T, Saito T, Hirasawa Y, Kubo T. Effect of acetabular cup position and orientation in cemented total hip arthroplasty. Clin Orthop Relat Res. 2001;388:135–142. doi: 10.1097/00003086-200107000-00020. [DOI] [PubMed] [Google Scholar]
- 14.Kalteis T, Handel M, Herold T, Perlick L, Paetzel C, Grifka J. Position of the acetabular cup: accuracy of radiographic calculation compared to CT-based measurement. Eur J Radiol. 2006;58:294–300. doi: 10.1016/j.ejrad.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear and component migration. J Arthroplasty. 1998;13:530–534. doi: 10.1016/S0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 16.Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76:517–523. doi: 10.1080/17453670510041501. [DOI] [PubMed] [Google Scholar]
- 17.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmermann JR. Dislocation after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 18.Liaw CK, Hou SM, Yang RS, Wu TY, Fuh CS. A new tool for measuring cup orientation in total hip arthroplasties from plain radiographs. Clin Orthop Relat Res. 2006;451:134–139. doi: 10.1097/01.blo.0000223988.41776.fa. [DOI] [PubMed] [Google Scholar]
- 19.Liaw CK, Yang RS, Hou SM, Wu TY, Fuh CS. Measurement of the acetabular cup anteversion on the simulated radiographs. J Arthroplasty. 2008 Apr 2. [Epub ahead of print]. [DOI] [PubMed]
- 20.Marx A, Knoch M, Pfortner J, Wiese M, Saxler G. Misinterpretation of cup anteversion in total hip arthroplasty using planar radiography. Arch Orthop Trauma Surg. 2006;126:487–492. doi: 10.1007/s00402-006-0163-0. [DOI] [PubMed] [Google Scholar]
- 21.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty: causes and prevention. Clin Orthop Relat Res. 1990;261:159–170. [PubMed] [Google Scholar]
- 22.Mian SW, Truchly G, Pflum FA. Computer tomography measurement of acetabular cup anteversion and retroversion in total hip arthroplasty. Clin Orthop Relat Res. 1992;276:206–209. [PubMed] [Google Scholar]
- 23.Munro BH. Correlation. In: Munro BH, editor. Statistical Methods for Healthcare Research. 3. Philadelphia, PA: Lippincott-Raven; 1997. pp. 224–245. [Google Scholar]
- 24.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 25.Najarian BC, Kilgore JE, Markel DC. Evaluation of component positioning in primary total hip arthroplasty using an imageless navigation device compared with traditional methods. J Arthroplasty. 2008;24:15–21. doi: 10.1016/j.arth.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 26.Nogler M, Kessler O, Prassl A, Donnelly B, Streicher R, Sledge JB, Krismer M. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin Orthop Relat Res. 2004;426:159–163. doi: 10.1097/01.blo.0000141902.30946.6d. [DOI] [PubMed] [Google Scholar]
- 27.Olivecrona H, Weidenhielm L, Olivecrona L, Beckman MO, Stark A, Noz ME, Maguire GQ, Zeleznik MP, Svensson L, Jonson T. A new CT method for measuring cup orientation after total hip arthroplasty. Acta Orthop Scand. 2004;75:252–260. doi: 10.1080/00016470410001169. [DOI] [PubMed] [Google Scholar]
- 28.Ritter MA. Dislocation and subluxation of the total hip replacement. Clin Orthop Relat Res. 1976;121:92–94. [PubMed] [Google Scholar]
- 29.Sah AP, Estok DM., II Dislocation rate after conversion from hip hemiarthroplasty to total hip arthroplasty. J Bone Joint Surg Am. 2008;90:506–516. doi: 10.2106/JBJS.G.00479. [DOI] [PubMed] [Google Scholar]
- 30.Schmalzried TP, Guttmann D, Grecula M, Amstutz H. The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am. 1994;76:677–688. doi: 10.2106/00004623-199405000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Seradge H, Nagle KR, Miller RJ. Analysis of version in the acetabular cup. Clin Orthop Relat Res. 1982;166:152–157. [PubMed] [Google Scholar]
- 32.Wines AP, McNicol D. Computer tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21:696–701. doi: 10.1016/j.arth.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 33.Yao L, Yao J, Gold RH. Measurement of acetabular version on the axiolateral radiograph. Clin Orthop Relat Res. 1995;316:106–111. [PubMed] [Google Scholar]