Abstract
Background
This study evaluated the clinical results of arthroscopically assisted single and double bundle tibial inlay reconstructions of an isolated posterior cruciate ligament (PCL) injury.
Methods
This study reviewed the data for 14 patients who underwent a single bundle tibial inlay PCL reconstruction (Group A) and 16 patients who underwent a double bundle tibial inlay PCL reconstruction (Group B) between August 1999 and August 2002. The mean follow-up period in groups A and B was 90.5 months and 64 months, respectively.
Results
The Lysholm knee scores in groups A and B increased from an average of 43.3 ± 7.04 and 44.7 ± 5.02 preoperatively to 88.1 ± 7.32 and 88.7 ± 9.11 points at the final follow-up, respectively. In group A, stress radiography using a Telos device showed that the preoperative mean side-to-side differences (SSDs) of 9.5 ± 1.60 mm at 30° of flexion and 9.8 ± 1.70 mm at 90° of flexion were improved to 2.8 ± 1.19 mm and 3.0 ± 1.1 mm, respectively. In group B, the preoperative SSDs of 10.4 ± 1.50 mm at 30° of flexion and 10.7 ± 1.60 mm at 90° of flexion improved to 2.7 ± 1.15 mm and 2.6 ± 0.49 mm, respectively. There was no significant difference in the clinical scores and radiologic findings between the two groups.
Conclusions
Single bundle and double bundle PCL reconstructions using the tibial inlay technique give satisfactory clinical results in patients with an isolated PCL injury, and there are no significant differences in the clinical and radiological results between the two techniques. These results suggest that it is unnecessary to perform the more technically challenging double bundle reconstruction using the tibial inlay technique in an isolated PCL injury.
Keywords: Posterior cruciate ligament, Reconstruction, Tibial inlay, Single bundle, Double bundle
A posterior cruciate ligament (PCL) injury is relatively rare but its incidence can range from 3% to 38% of acute knee injuries.1) In particular, an isolated injury is even less common, which has resulted in a lack of evidence-based literature regarding treatment, and unsubstantiated debate about optimal treatment. The general consensus appears to be that isolated PCL tears do well when treated nonsurgically,2) and although some encouraging results have been obtained for nonsurgical treatment, several studies concluded that the symptomatic posterior abnormal laxity increases and the incidence of osteoarthritis is higher in patients treated conservatively at a long term follow-up.3-5) Recently, favorable results were reported for the surgical treatment of an isolated PCL injury,6-7) but these studies focused on the clinical comparisons between single transtibial and tibial inlay techniques. Moreover, the clinical relevance of a variety of advocated reconstructive procedures based on biomechanical data is contraversial.1,4,8) The tibial tunnel method is used most commonly to treat PCL injuries but several studies have reported that the tibia inlay method has biomechanically significant advantages.8-10) In addition, others reported that the double bundle technique might mimic the function of a normal PCL more closely and may be superior to a single bundle reconstruction.11-13) Therefore, to the best of our knowledge, no clinical study has compared the outcomes of single bundle and double bundle tibial inlay reconstructions in patients with an isolated PCL injury. The authors examined whether the double bundle method can restore more closely the normal laxity of the PCL than the single bundle method if the tibial inlay technique is used instead of the transtibial technique in patients with an isolated PCL injury. It was suggested that the outcome of the single bundle tibial inlay technique is likely to be similar to that of the double bundle tibial inlay technique.
METHODS
Between August 1999 to August 2002, 78 patients with isolated PCL injuries were treated at our institution. Among them, 43 patients were treated using conservative methods. The data of the other 35 patients treated with a PCL reconstruction was reviewed retrospectively to determine the clinical and radiological outcomes of single and double bundle tibial inlay techniques for the treatment of patients with an isolated PCL injury. Thirty patients with complete follow-up documentation were included for analysis. Five patients were lost to follow-up for geographic reasons and an unknown address within 5 months after surgery. Selection of the original 35 patients was limited to patients with an isolated PCL injury without a positive anterior drawer sign, a positive Lachmann test, varus or valgus instability, excessive external tibial rotation compared to the contralateral normal knee, genu recurvatum or a pivot shift. The patients had at least grade II laxity (> 5 mm translation by the posterior drawer test versus the intact side). Patients with posterolateral, posteromedial or anterior instability, and those suspected of having a multiligament injury were excluded. The study protocol was approved by the institutional review board. The 30 patients included in the analysis were followed up for a minimum of 4 years after the single bundle tibial inlay PCL reconstruction (Group A) or double bundle tibial inlay PCL reconstruction (Group B). There were 14 patients in group A and 16 in group B. In group A, the average time from injury to reconstruction was 11.3 months (range, 3 to 36 months), and the average age of the patients was 34 years (range, 20 to 61 years). Eleven of the 14 patients were male and 3 were female. The patients were examined clinically and radiographically after an average follow-up of 90.5 months (range, 74 to 101 months). In terms of the injury mechanisms, 11 were motor-vehicle accident cases and 3 were sports-related injuries.
In group B, the average time from the injury to reconstruction was 7.1 months (range, 3 to 32 months). The mean age of the patients was 36 years (range, 18 to 52 years), and 15 were male and 1 was female. The patients were examined clinically and radiographically after an average follow-up of 64 months (range, 55 to 76 months). The mechanisms of injury were; 12 motor vehicle accidents, 2 falling injuries, and 2 sports-related injuries.
The PCL reconstruction was performed under the following indicators: 1) pain or instability during the daily activities of living, such as sprinting and climbing stairs despite non-surgical management for more than 3 months, and 2) a PCL injury with a > 8 mm side-to-side difference in posterior displacement measured using a Telos device (SE2000, Telos GmbH, Marburg, Germany). The surgical indicator for an isolated PCL injury is generally a posterior displacement ≥ 10 mm.14) However, recent improvements in surgical techniques have increased the number of satisfactory clinical outcomes after a surgical reconstruction with an 8 mm to 10 mm posterior displacement.15) Therefore, a minimum side-to-side difference in posterior displacement of 8 mm was determined to be the indication for surgery, and most grade II patients had a posterior displacement of ≥ 8 mm.
In terms of the associated injuries, 2 patients in group A had a meniscal injury. One of these two had chondromalacia grade II of the medial femoral condyle, and the other had chondromalacia III of the patellofemoral joint. In group B, 1 patient had a meniscal injury, and 2 patients had chondromalacia III of the patellofemoral joint. With respect to graft selection, group A included 10 bone-patellar tendon-bone (BPTB) allografts and 4 achilles tendon allografts, and the 16 group B cases all received 16 achilles tendon allografts. The preoperative and final follow-up Lysholm scores, Tegner activity scores,16) and the posterior drawer tests at 90° were evaluated by two surgeons. The postoperative ratings were assessed by another two surgeons who were blinded to the identity of the treatment group. Subjective assessments of the posterior drawer test findings were evaluated using a traditional grading system, i.e., grade I (0 mm to 5 mm), grade II (6 mm to 10 mm), grade III (> 10 mm). Grade I was awarded for ≤ 5 mm of abnormal posterior displacement of the tibia with respect to the femur with the anterior border of the tibial plateau anterior to the femoral condyles. Grade II indicated 6 mm to 10 mm of abnormal displacement with the anterior border of the tibial plateau flush with the femoral condyles, and Grade III denoted abnormal posterior displacement of the tibial plateau of > 10 mm and with the anterior border of the tibial plateau left behind with the femoral condyles. Three surgeons assessed the lateral stress radiographs of each knee at 30° and 90° of flexion. Stress radiography was performed both preoperatively and postoperatively using a Telos device. A 20-N posterior load was applied to the proximal tibia, and the findings were compared with the ipsilateral lateral radiographs to determine the side-to-side differences (Figs. 1 and 2). The radiographs were measured individually by each of the three surgeons, and the degree of laxity was calibrated by the mean of the side-to-side differences, as measured by each of the three surgeons. A Wilcoxon's signed rank test was used to determine the differences between the preoperative and postoperative data, including the clinical and radiological data within each group, and a Mann-Whitney U-test was used to measure the differences between the preoperative and postoperative data of the patients who underwent either the single bundle tibial inlay technique (group A) or double bundle tibial inlay technique (group B). A p-value < 0.05 was considered significant. All analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA).
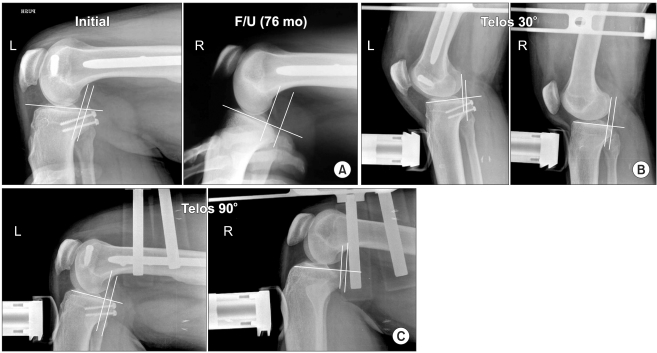
Fig. 1.
Thirty-two year old man who was involved in a motor vehicle accident. Single bundle posterior cruciate ligament reconstruction was performed using the tibial inlay technique. (A) Stress view, preoperative and follow-up (F/U) 76 months. (B) Posterior stress roentgenography using the Telos stress device at 30° of flexion showed grade 1 posterior instability at both the preoperative and follow-up 76 months. (C) Posterior stress roentgenography using the Telos stress device at 90° of flexion showed grade 1 posterior instability at both the preoperative and follow-up 76 months.
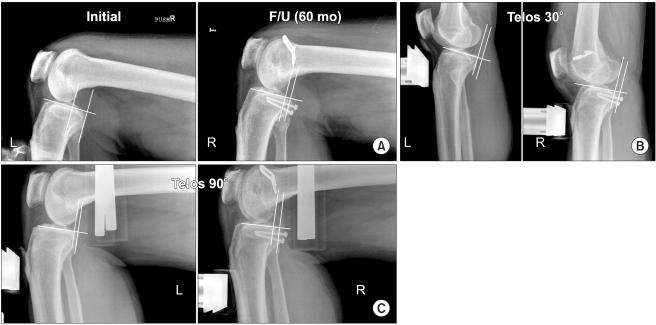
Fig. 2.
Forty-six year old man who was involved in a motor vehicle accident. A double bundle posterior cruciate ligament reconstruction was performed using the tibial inlay technique. (A) Stress view, preoperative and follow-up 60 months. (B) Posterior stress roentgenography using the Telos stress device at 30° of flexion showed grade 1 posterior instability both preoperatively and at the 60 months follow-up. (C) Posterior stress roentgenography using the Telos stress device at 90° of flexion showed grade 1 posterior instability preoperatively and at the 60 months follow-up.
Surgical Technique
Group A: Arthroscopically assisted single bundle tibial inlay technique (Fig. 3)
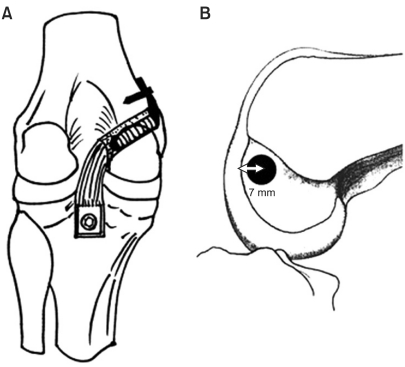
Fig. 3.
(A) The illustration shows posterior view of a single bundle tibial inlay posterior cruciate ligament reconstruction. (B) Lateral view of femoral tunnel position in the medial femoral condyle. The center of a 10 mm diameter femoral tunnel was placed 7 mm proximal to the margin of the articular cartilage of the medial femoral condyle at 11 o'clock in the left knee joint, or at 1 o'clock in the right knee joint.
Fourteen patients underwent a single bundle tibial inlay PCL reconstruction. The knee was placed supine with the patient in the lateral decubitus position. The graft tendon was prepared after diagnostic arthroscopy and confirmation of the PCL injury. For femoral tunnel preparation, the tip of the anterior cruciate ligament (ACL) tibial guide was placed 7 mm proximal to the margin of the articular cartilage of the medial femoral condyle at the 11 o'clock position in the left knee joint, or at the 1 o'clock position in the right knee joint. The sleeve of the ACL guide was placed on the medial femoral condyle, and a guide pin was then inserted in an outside-in direction. A longitudinal skin incision (about 3 cm long) was then made on the medial femoral condyle along the guide pin. The vastus medialis obliquus muscle was undermined to expose the outer aperture of the posterior femoral tunnel. Under arthroscopic visualization, the femoral tunnel was reamed using a 10 mm cannulated headed reamer. The edge of the femoral tunnel was chamfered to reduce the concentration of stress on the graft. A wire loop was then passed through the femoral tunnel into the joint space. To prepare the tibial inlay site, the interval between the medial head of the gastrocnemius muscle and the semimembranosus was first identified using the posterior approach. A blunt dissection and release of the medial head of the gastrocnemius muscle were then performed to expose the capsule of the posterior knee. The capsule was then incised and the footprint of the PCL was identified. A groove for the inlay graft was made (1 cm in width and 2 cm in length) within the footprint of the PCL using an osteotome and rongeur. Finally, the bone plug of the inlay graft was fixed firmly using a 4.0 mm cancellous screw and washer. The graft was secured to the prepositioned 18-guage wire and drawn from the posterior aspect of the knee through an intercondylar notch into the femoral tunnel. Tension was applied to the graft in the femoral tunnel while moving the knee 20 times through the full range of motion. The graft was then fixed with an absorbable interference screw and a staple with an achilles allograft and a nonabsorable interference screw with a BPTB allograft with the knee in 90° of flexion while applying an anteriorly directed force to maintain the normal anterior tibial step.
Group B: Arthroscopically assisted double bundle tibial inlay technique (Fig. 4)
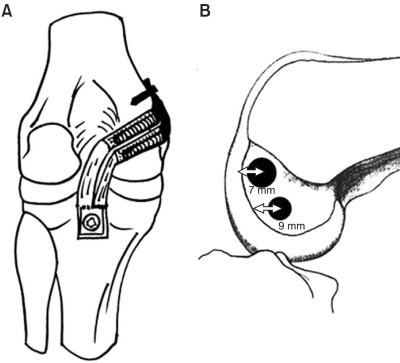
Fig. 4.
(A) The illustration shows the posterior view of double bundle tibial inlay posterior cruciate ligament reconstructions. (B) Lateral view of the femoral tunnel position in the medial femoral condyle. The center for the 9 mm diameter anterolateral femoral tunnel was placed 7 mm proximal to the margin of the articular cartilage of the medial femoral condyle at the 11 o'clock position in the left knee joint, or at the 1 o'clock position in the right knee joint, and the center for 8 mm diameter posteromedial femoral tunnel, at 9 mm proximal to the margin of the articular cartilage at the 3 o'clock position on the right (9 o'clock on left). The distance between femoral tunnels must be > 4 mm to avoid tunnel bridge collapse.
All 16 patients underwent a double bundle tibial inlay PCL reconstruction using an achilles tendon allograft. The grafts were split sagittally to obtain a 9 and 7 mm diameter bundle. A similar technique to that described for the single bundle tibial inlay was used except for the femoral tunnel position. For an anterolateral bundle reconstruction, the tip of the ACL tibial guide was placed 7 mm proximal to the margin of the articular cartilage of the medial femoral condyle at either the 11 o'clock position in the left knee joint, or at the 1 o'clock position in the right knee joint. For the posteromedial bundle, the tip of the ACL tibial guide was placed 9 mm proximal to the margin of the articular cartilage at the 3 o'clock position on the right (9 o'clock on the left). The distance between femoral tunnels must be > 4 mm to avoid tunnel bridge collapse. After guide pin insertion, the anterolateral and posteromedial tunnel was reamed using a 9 mm and 8 mm headed reamer, respectively. Two wire loops was then passed through the femoral tunnel into the joint space. After tibial site preparation, as described for the single bundle technique, both grafts were secured to two prepositioned 18-guage wires and then drawn from the posterior aspect of the knee through the intercondylar notch into the femoral tunnel. Tension was applied to the anterolateral graft in the femoral tunnel while moving the knee 20 times through the full range of motion, and fixed with a biointerference screw and a staple from the outside with the knee in 90° of flexion while applying an anteriorly directed force to maintain a normal anterior tibial step. Once more, tension was applied to the posteromedial bundle in the posterior femoral tunnel while moving the knee 20 times through the full range of motion. Femoral fixation of the posteromedial bundle was obtained using an absorbable interference screw fixed from the outside in a near extension position. Its free end was also fixed using a staple on the cortex of the medial femoral condyle.
Postoperative Rehabilitation
To prevent posterior translation of the tibia after surgery, all patients were immobilized with the long leg cast in the full extended position. Quadriceps muscle strengthening and straight leg raising exercises were started from the first day after surgery. At 3 weeks after surgery, the long leg cast was removed, and a full extension knee brace was applied. Approximately 3 to 4 weeks postoperatively, active knee flexion exercise and partial weight bearing were allowed. At 3 months postoperatively, the knee braces were removed, and full weight bearing was allowed. Low impact sports activities were permitted at 6 months.
RESULTS
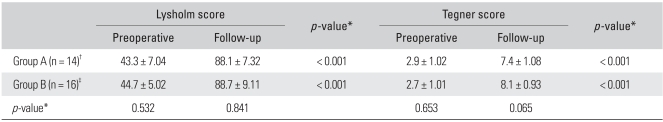
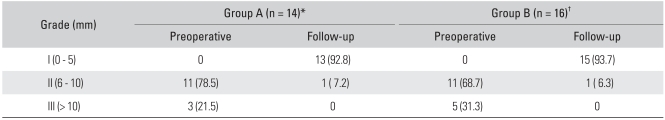
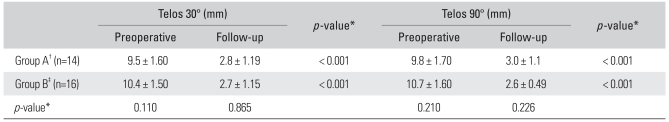
There were no statistically significant differences in age and gender between the 2 groups but there were significant differences in the time interval between the injury and reconstruction and the follow-up period. In group A, the average Lysholm knee scores increased (p < 0.001) from 43.3 ± 7.04 (range, 32 to 57) preoperatively to 88.1 ± 7.32 (range, 71 to 98) points at the final follow-up. The mean Tegner activity level scores increased (p < 0.001) from 2.9 ± 1.02 points (range, 1 to 5 points) preoperatively to 7.4 ± 1.08 points (range, 5 to 9 points) at the final follow-up (Table 1). The preoperative PCL laxity, as determined using the posterior drawer test at 90° of flexion, showed that all group A patients had at least Grade II PCL laxity, i.e., 11 knees had grade II abnormal laxity (6 to 10 mm), and 3 knees had grade III abnormal laxity (> 10 mm). All patients showed improvement to a lower grade postoperatively. One knee in 3 patients with grade III laxity improved to grade II and the other 13 patients improved to grade I (Table 2). The stress radiography vs. ipsilateral radiographs in group A using the Telos device revealed a preoperative mean side-to-side difference (SSD) of 9.5 ± 1.60 mm (range, 6 to 12 mm) at 30° of flexion and 9.8 ± 1.70 mm (range, 7 to 13 mm) at 90° of flexion, which improved (p < 0.001) to 2.8 ± 1.19 mm and 3.0 ± 1.1 mm, respectively (Table 3).
Table 1.
Comparison of the Lysholm Functional and Tegner Activity Scores of the Two Study Groups
*Wilcoxon signed rank test, Mann-Whitney U-test, p < 0.05. †Group A: Single bundle tibial inlay posterior cruciate ligament (PCL) reconstruction. ‡Group B: Double bundle tibial inlay PCL reconstruction.
Table 2.
Comparison of the Knee Laxity as Determined by the Posterior Drawer Test at 90° of Flexion
Values are presented as number (%).
PCL: Posterior cruciate ligament.
*Group A: Single bundle tibial inlay PCL reconstruction. †Group B: Double bundle tibial inlay PCL reconstruction.
Table 3.
Side-to-Side Differences Determined Using a Telos Stress Device at 30 and 90° of Flexion
PCL: Posterior cruciate ligament.
*Wilcoxon signed rank test, Mann-Whitney U-test, p < 0.05. †Group A: Single bundle tibial inlay PCL reconstruction. ‡Group B: Double bundle tibial inlay PCL reconstruction.
For group B, the average Lysholm knee scores increased (p < 0.001) from 44.7 ± 5.02 (range, 34 to 53) preoperatively to 88.7 ± 9.11 (range, 71 to 98) at the final follow-up. The Tegner activity levels increased (p < 0.001) from 2.7 ± 1.01 points preoperatively (range, 1 to 5) to 8.1 ± 0.93 points (range, 6 to 10 points) at the final follow-up (Table 1). PCL laxity according to the posterior drawer test at 90° of flexion showed that all group B patients had at least Grade II PCL laxity, i.e. 11 knees with grade II instability (6 to 10 mm) and 5 knees with grade III instability (> 10 mm). All patients showed improvement to a lower grade after surgery. One knee in the patients with grade III laxity improved to grade II laxity, and the other 15 patients improved to grade I (Table 2). Stress radiography versus ipsilateral radiographs of group B using the Telos device showed preoperative mean SSD of 10.4 ± 1.50 mm (range, 8 to 13 mm ) at 30° of flexion and 10.7 ± 1.60 (range, 7 to 13 mm) at 90° of flexion, which improved (p < 0.001) to 2.7 ± 1.15 mm and 2.6 ± 0.49 mm, respectively (Table 3).
There was no significant difference in the clinical scores or radiographic findings between groups A and B (Tables 1 and 3).
One patient in group A and 2 patients in group B showed approximately 10° of knee flexion limitation compared to the contralateral sides. Two patients in group A and 1 patient in group B showed quadriceps atrophy. All these patients complained of mild anterior knee pain. Pain around the staple developed in 2 patients, which disappeared after removing the staple. No other complications, such as neurovascular injury, metal failure and infections were observed during the minimum 4 year follow-up period.
DISCUSSION
The treatment principles of a posterior cruciate ligament injury are relatively less well established that those of other knee injuries. The general consensus is that surgical treatment is needed in cases with other combined ligament injuries,17,18) and that non-surgical treatment is sufficient for isolated injuries.2) However, many studies reported that patients with an isolated PCL injury show symptomatic posterior abnormal laxity and a higher incidence of osteoarthritis at the medial femoral articular cartilage and patellofemoral joint after conservative treatment in the long term.3-5)
Accordingly, several studies have concluded that surgery is essential for an isolated PCL injury.6,19) Fanelli et al.14) recommended a surgical reconstruction of an isolated PCL injury when the posterior tibial drop back is greater than the flat tibial step-off and there is an associated bony or meniscal injury, or when there is progressive functional degeneration in the knee. Seon and Song7) included 12 patients with grade II in their 43 patients. In the present study, most patients (73%) were rated as grade II, and 8 patients in Grade III were also included. Many surgical techniques for PCL reconstructions have been described.1,4,8) However, no current surgical procedure has been able to consistently correct the abnormal posterior laxity or provide consistent functional results.
The transtibial PCL reconstruction technique and its modifications are commonly used.1,4) However, several authors have introduced a PCL reconstruction using a new tibial inlay technique due to the technical difficulties, ineffective in situ graft tensioning and possibly late failure caused by abrasive graft wear. They have demonstrated that the tibial inlay method has biomechanically significant advantages than transtibial techniques.8-10) However, other biomechanical and cadaveric studies have produced inconsistent results.20-22) Moreover, although several studies have evaluated a surgical reconstruction of PCL deficiencies,4,8,23-26) they failed to present well-controlled data concerning the surgical treatment of isolated PCL injuries.
Recently surgical treatment results for patients with an isolated PCL injury and associated symptoms, such as, pain, swelling, or giving way during strenuous activity, have been reported.6,7,27) MacGillivray et al.6) found that a transtibial reconstruction is indistinguishable from the tibial inlay technique but neither modality consistently restores the anteroposterior stability to its original state when the single bundle technique is used.
Recently, the advancements in our understanding of PCL anatomical structures have caused the focus to shift to a double bundle PCL reconstruction for restoring the PCL anatomy. Several authors have reported that the double bundle technique may mimic the function of the normal PCL more closely and be better than a single bundle reconstruction.12,28) In a recent study conducted in an in vivo clinical setting, Hatayama et al.28) reported no significant difference between the single bundle and double bundle transtibial techniques in terms of their short-term stabilities. In a prospective, nonrandomized comparison of single bundle and double bundle transtibial reconstructions, Wang et al.29) did not detect any significant difference between the two techniques at a minimum of two years postoperatively. For a tibial inlay reconstruction, Bergfeld et al.30) compared single and double-bundle reconstructions using the tibial inlay technique of the posterior cruciate ligament based on cadaveric studies. They reported no differences in posterior tibial translation and concluded that it unnecessary to perform a double-bundle reconstruction of the posterior cruciate ligament if a tibial inlay construct is used. However, they did not evaluate the rotational stability, and the model they used was an isolated posterior cruciate ligament deficiency model with intact posterolateral corner structures. Whiddon et al.31) compared a posterior tibial translation and external rotation after a single and double bundle tibial inlay reconstruction of the posterior cruciate ligament in both a posterolateral corner deficient and repaired cadaver model. They found that a double bundle reconstruction offers measurable benefits in terms of the rotational stability and posterior translation in the setting of an untreated posterolateral corner injury. However, no in vivo study has compared the clinical results of a single and double bundle tibial inlay PCL reconstruction, particularly in patients with an isolated PCL injury. Initially, this study examined whether the double bundle method could more closely restore the normal laxity of the PCL than the single bundle method if the tibial inlay technique was used for patients with an isolated PCL injury instead of the transtibial technique. With a minimum follow-up of 4 years, the preoperative side-to-side difference in the two groups in this study was 9.8 ± 1.70 mm and 10.7 ± 1.60 mm at 90° of flexion, which decreased to 3.0 ± 1.1 and 2.6 ± 0.49 mm after surgery, respectively. These results concur with those of Seon and Song,7) in which 11.0 ± 1.7 mm and 3.3 ± 1.6 mm SSD was recorded before and after surgery, respectively, for a single tibial inlay reconstruction of an isolated PCL injury. In this study, all patients were satisfied and the postoperative SSD was similar in the two groups. This suggests that a double-bundle PCL reconstruction may not have any advantages over a single-bundle PCL reconstruction, as shown in Bergfield's cadaveric studies,30) and that a single bundle tibial inlay reconstruction may be sufficient when using the tibial inlay method in an isolated PCL injury.
Our study had several limitations. First the number of patients enrolled was small, and 5 patients were lost during the follow-up, which could have biased the results. These 5 patients included 1 patient in group A and 4 in group B. Second, there was a difference in not only the time interval between the injury and reconstruction but also in the follow-up period. These differences may have affected the outcome. Finally, this study is limited by its retrospective and nonrandomized nature.
Single bundle and double bundle PCL reconstructions using the tibial inlay technique produce satisfactory clinical results in patients with an isolated PCL injury. There were no significant differences in the clinical and radiologic results between the two techniques. Therefore, these results suggest that it is unnecessary to perform a more technically challenging double bundle reconstruction using the tibial inlay technique in an isolated PCL injury.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
References
- 1.Fanelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: part II. Arthroscopy. 1995;11(5):526–529. doi: 10.1016/0749-8063(95)90127-2. [DOI] [PubMed] [Google Scholar]
- 2.Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries: a prospective study. Am J Sports Med. 1999;27(3):276–283. doi: 10.1177/03635465990270030201. [DOI] [PubMed] [Google Scholar]
- 3.Boynton MD, Tietjens BR. Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am J Sports Med. 1996;24(3):306–310. doi: 10.1177/036354659602400310. [DOI] [PubMed] [Google Scholar]
- 4.Clancy WG, Jr, Shelbourne KD, Zoellner GB, Keene JS, Reider B, Rosenberg TD. Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament: report of a new procedure. J Bone Joint Surg Am. 1983;65(3):310–322. [PubMed] [Google Scholar]
- 5.Keller PM, Shelbourne KD, McCarroll JR, Rettig AC. Non-operatively treated isolated posterior cruciate ligament injuries. Am J Sports Med. 1993;21(1):132–136. doi: 10.1177/036354659302100122. [DOI] [PubMed] [Google Scholar]
- 6.MacGillivray JD, Stein BE, Park M, Allen AA, Wickiewicz TL, Warren RF. Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year follow-up. Arthroscopy. 2006;22(3):320–328. doi: 10.1016/j.arthro.2005.08.057. [DOI] [PubMed] [Google Scholar]
- 7.Seon JK, Song EK. Reconstruction of isolated posterior cruciate ligament injuries: a clinical comparison of the transtibial and tibial inlay techniques. Arthroscopy. 2006;22(1):27–32. doi: 10.1016/j.arthro.2005.08.038. [DOI] [PubMed] [Google Scholar]
- 8.Berg EE. Posterior cruciate ligament tibial inlay reconstruction. Arthroscopy. 1995;11(1):69–76. doi: 10.1016/0749-8063(95)90091-8. [DOI] [PubMed] [Google Scholar]
- 9.Bergfeld JA, McAllister DR, Parker RD, Valdevit AD, Kambic HE. A biomechanical comparison of posterior cruciate ligament reconstruction techniques. Am J Sports Med. 2001;29(2):129–136. doi: 10.1177/03635465010290020401. [DOI] [PubMed] [Google Scholar]
- 10.Markolf KL, Zemanovic JR, McAllister DR. Cyclic loading of posterior cruciate ligament replacements fixed with tibial tunnel and tibial inlay methods. J Bone Joint Surg Am. 2002;84(4):518–524. doi: 10.2106/00004623-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Harner CD, Janaushek MA, Kanamori A, Yagi M, Vogrin TM, Woo SL. Biomechanical analysis of a double-bundle posterior cruciate ligament reconstruction. Am J Sports Med. 2000;28(2):144–151. doi: 10.1177/03635465000280020201. [DOI] [PubMed] [Google Scholar]
- 12.Race A, Amis AA. The mechanical properties of the two bundles of the human posterior cruciate ligament. J Biomech. 1994;27(1):13–24. doi: 10.1016/0021-9290(94)90028-0. [DOI] [PubMed] [Google Scholar]
- 13.Shearn JT, Grood ES, Noyes FR, Levy MS. Two-bundle posterior cruciate ligament reconstruction: how bundle tension depends on femoral placement. J Bone Joint Surg Am. 2004;86(6):1262–1270. [PubMed] [Google Scholar]
- 14.Fanelli GC, Giannotti BF, Edson CJ. The posterior cruciate ligament arthroscopic evaluation and treatment. Arthroscopy. 1994;10(6):673–688. doi: 10.1016/s0749-8063(05)80067-2. [DOI] [PubMed] [Google Scholar]
- 15.Johnson DH, Fanelli GC, Miller MD. PCL 2002: indications, double-bundle versus inlay technique and revision surgery. Arthroscopy. 2002;18(9 Suppl 2):40–52. doi: 10.1053/jars.2002.36515. [DOI] [PubMed] [Google Scholar]
- 16.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43–49. [PubMed] [Google Scholar]
- 17.L'Insalata JC, Harner CD. Treatment of acute and chronic posterior cruciate ligament deficiency: new approaches. Am J Knee Surg. 1996;9(4):185–193. [PubMed] [Google Scholar]
- 18.Miller MD, Olszewski AD. Posterior cruciate ligament injuries: new treatment options. Am J Knee Surg. 1995;8(4):145–154. [PubMed] [Google Scholar]
- 19.Sekiya JK, West RV, Ong BC, Irrgang JJ, Fu FH, Harner CD. Clinical outcomes after isolated arthroscopic single-bundle posterior cruciate ligament reconstruction. Arthroscopy. 2005;21(9):1042–1050. doi: 10.1016/j.arthro.2005.05.023. [DOI] [PubMed] [Google Scholar]
- 20.McAllister DR, Markolf KL, Oakes DA, Young CR, McWilliams J. A biomechanical comparison of tibial inlay and tibial tunnel posterior cruciate ligament reconstruction techniques: graft pretension and knee laxity. Am J Sports Med. 2002;30(3):312–317. doi: 10.1177/03635465020300030201. [DOI] [PubMed] [Google Scholar]
- 21.Margheritini F, Mauro CS, Rihn JA, Stabile KJ, Woo SL, Harner CD. Biomechanical comparison of tibial inlay versus transtibial techniques for posterior cruciate ligament reconstruction: analysis of knee kinematics and graft in situ forces. Am J Sports Med. 2004;32(3):587–593. doi: 10.1177/0363546503261717. [DOI] [PubMed] [Google Scholar]
- 22.Oakes DA, Markolf KL, McWilliams J, Young CR, McAllister DR. Biomechanical comparison of tibial inlay and tibial tunnel techniques for reconstruction of the posterior cruciate ligament: analysis of graft forces. J Bone Joint Surg Am. 2002;84(6):938–944. doi: 10.2106/00004623-200206000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Cross MJ, Powell JF. Long-term followup of posterior cruciate ligament rupture: a study of 116 cases. Am J Sports Med. 1984;12(4):292–297. doi: 10.1177/036354658401200409. [DOI] [PubMed] [Google Scholar]
- 24.Hughston JC, Bowden JA, Andrews JR, Norwood LA. Acute tears of the posterior cruciate ligament: results of operative treatment. J Bone Joint Surg Am. 1980;62(3):438–450. [PubMed] [Google Scholar]
- 25.Lipscomb AB, Jr, Anderson AF, Norwig ED, Hovis WD, Brown DL. Isolated posterior cruciate ligament reconstruction: long-term results. Am J Sports Med. 1993;21(4):490–496. doi: 10.1177/036354659302100402. [DOI] [PubMed] [Google Scholar]
- 26.Schulte KR, Chu ET, Fu FH. Arthroscopic posterior cruciate ligament reconstruction. Clin Sports Med. 1997;16(1):145–156. doi: 10.1016/s0278-5919(05)70011-9. [DOI] [PubMed] [Google Scholar]
- 27.Garofalo R, Jolles BM, Moretti B, Siegrist O. Double-bundle transtibial posterior cruciate ligament reconstruction with a tendon-patellar bone-semitendinosus tendon autograft: clinical results with a minimum of 2 years' follow-up. Arthroscopy. 2006;22(12):1331–1338. doi: 10.1016/j.arthro.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 28.Hatayama K, Higuchi H, Kimura M, Kobayashi Y, Asagumo H, Takagishi K. A comparison of arthroscopic single- and double-bundle posterior cruciate ligament reconstruction: review of 20 cases. Am J Orthop (Belle Mead NJ) 2006;35(12):568–571. [PubMed] [Google Scholar]
- 29.Wang CJ, Weng LH, Hsu CC, Chan YS. Arthroscopic single-versus double-bundle posterior cruciate ligament reconstructions using hamstring autograft. Injury. 2004;35(12):1293–1299. doi: 10.1016/j.injury.2003.10.033. [DOI] [PubMed] [Google Scholar]
- 30.Bergfeld JA, Graham SM, Parker RD, Valdevit AD, Kambic HE. A biomechanical comparison of posterior cruciate ligament reconstructions using single- and double-bundle tibial inlay techniques. Am J Sports Med. 2005;33(7):976–981. doi: 10.1177/0363546504273046. [DOI] [PubMed] [Google Scholar]
- 31.Whiddon DR, Zehms CT, Miller MD, Quinby JS, Montgomery SL, Sekiya JK. Double compared with single-bundle open inlay posterior cruciate ligament reconstruction in a cadaver model. J Bone Joint Surg Am. 2008;90(9):1820–1829. doi: 10.2106/JBJS.G.01366. [DOI] [PubMed] [Google Scholar]