Abstract
This study examined the clinical and pathological features after a microvascular anastomosis of a rat femoral artery using four different suture techniques. Sixty Sprage-Dawely rats were divided randomly into 4 groups. Fifteen bisected arteries (one from each animal) in Group I, II, III and IV were sutured with the simple interrupted suture, continuous suture, sleeve suture and cuff suture, respectively. The anastomosis times in Group I, II, III and IV were 28.67, 14.67, 15.47 and 15.93 min, respectively. Immediate bleeding that stopped without intervention (grade I) was observed in 67%, 73% and 60% of the anastomosed vessels in Groups II, III and IV, respectively, while 60% of the vessels in Group I showed light bleeding that was inhibited by gentile pressure (grade II). All vessels examined appeared to be patent at 5 and 15 min after the anastomosis. On the 7th day postoperatively, the vessels of Group I showed the highest patency rate (93%) compared with Groups II (67%), III (73%) and IV (87%). Moreover, there were more pronounced pathological changes in Group I than in the other groups. These changes included endothelial loss, endothelial proliferation, degeneration and necrosis of the tunica media. Suture materials surrounded by an inflammatory reaction were also observed. In conclusion, the simple interrupted suture is preferable for microvascular anastomosis due to its highest patency rate. The other techniques investigated can be good alternatives because of their short anastomotic time and moderate pathological changes.
Keywords: anastomosis, microsurgery, pathology, suture
Introduction
Suitable suture techniques, which reduce the surgery time and vessel wall trauma with little or no pathological complications, form the basis of surgical safety after microvascular anastomosis and are welcomed by microsurgeons [6]. The conventional interrupted suture technique is considered the gold standard for microvessel anastomosis but has certain disadvantages, such as being time consuming as well as having considerable intimal and medial damage [15]. Surgeons are constantly developing new techniques to overcome some of the disadvantages associated with the conventional interrupted suture.
This study compared both clinically and pathologically the continuous, sleeve and autogenous arterial cuff suturing techniques with the conventional interrupted technique in the rat femoral artery.
Materials and Methods
Materials
Sixty Sprage-Dawley rats, weighing 250-350 g, were obtained from and housed at the Animal House, Faculty of Medicine, Assiut University, Egypt. All procedures were performed according to the National Bylaws on the care and use of laboratory animals in the Microsurgical Skill Laboratory of the Continued Medical Education Center of the Faculty of Medicine, Assiut University, Egypt.
Methods
Suture techniques
The animals were divided into 4 groups containing 15 animals each. In all groups, the animals were anesthetized by an intraperitoneal injection of thiopental sodium (Intraval; EIPICO, Egypt). At ×10 magnification, one femoral artery/animal was exposed and skeletonized in the standard manner using a groin incision, and the vessel spasm was neutralized with 2% lidocaine (Debocaine; El-Nasr Chemical, Egypt). Double approximating microvascular clamps were applied proximally and distally to the vessel, which was then divided. The bisected ends were flushed with heparinzed saline (10 U/2 ml). The adventitia of the vessel stumps was trimmed off and the vessel ends were dilated gently using jeweler's forceps. The prepared vessel ends in groups I, II, III and IV were anastomosed using conventional interrupted, continuous, sleeve suture, and autogenous arterial cuff suture techniques, respectively. 11/0 monofilament polymide sutures, 50-mm in diameter and 4.1 mm in length, and a 3/8 circle needle (Ethilon; Ethicon, Germany) under microscopic (Leica MS-5; Leica, Germany).
Anastomotic time
The time elapsed from the first stitch to the last was recorded for every arterial anastomosis in all 4 groups.
Anastomotic leakage
After releasing the clamps, the leakage of blood at the anastomotic site was assessed and graded for each sutured vessel. Grade I leakage was immediate bleeding that stopped without intervention. Grade II was light bleeding that was stopped by gentile pressure. Grade III was heavy bleeding that required reclamping and additional suturing.
Patency rate
The patency was evaluated in all sutured vessels 5 and 15 min after completing the anastomosis as well as on the 7th postoperative day using a milking test, and were classified as being either patent or non-patent. Patency of the anastomotic site was indicated if the milking test showed immediate refilling, while slow refilling suggested vessel spasm, partial thrombosis or technical error. Finally, no refilling indicated thrombosis or severe technical error.
Histopathology
On the 7th postoperative day, five patent specimens of the operated femoral arteries, 1 cm in length, which included the anastomotic sites, were taken from each group for a histopathology examination. The tissue specimens were fixed in 10% neutral buffered formalin, dehydrated in a graded series of alcohol, cleared with methyl benzoate and embedded in paraffin wax. Five micron thick cross- and longitudinal sections were cut and stained with hemotoxylin and eosin [2]. The stained sections were examined for any endothelial injury and proliferation, medial necrosis, the presence and location of the suture materials and the degree of inflammatory reaction.
Scanning electron microscopy
For further assessment, two anastomoses from each group were also obtained one week after surgery, and fixed in a solution containing paraformaldhyde (2.5%) and gluteraldhyde (2.5%) in a phosphate buffer (pH 7.3) for 24 h. The specimens were washed in 0.1 M of phosphate buffer, dehydrated in a graded series of ethanol, dried in liquid carbon dioxide and then sputter coated with gold palladius. The lumen of the prepared vessels was then examined by scanning electron microscopy (JSM-5400 LV; JEOL, Japan) operated at 20 KV in the Electron Microscopy Unit of Assiut University.
Statistics
Statistical analysis was performed using one way ANOVA and multiple comparisons were carried out using a Newman-Keulus test. A value of p < 0.05 was considered significant.
Results
Anastomotic time
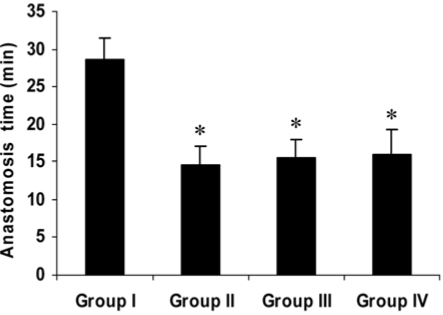
The mean anastomotic times in Group I, II, III and IV were 28.67 ± 2.82, 14.67 ± 2.47, 15.47 ± 2.50 and 15.93 ± 3.33 min, respectively (Fig. 1). The mean time elapsed for Group I was the longest of all 4 techniques, which presented a time saving of approximately 50%.
Fig. 1.
Anastomosis time for the different suture techniques. The continuous, sleeve and cuff techniques resulted in a significant reduction of the anastomotic time compared with the interrupted technique (*p < 0.01). †Group I: simple interrupted suture, Group II: continuous suture, Group III: sleeve suture, Group IV: cuff suture.
Anastomotic leakage
Transient bleeding that stopped without any intervention (grade I) was observed in 40, 67, 73 and 60% of Group I, II, III and IV, respectively. On the other hand, light bleeding that inhibited by gentle pressure (grade II) was observed in 60, 33, 27 and 40% of the anastomosed vessels in Group I, II, III and IV, respectively. None of the anastomosed vessels showed bleeding that required re-clamping and additional suturing (grade III).
Patency rate
All the repaired vessels were patent 5 and 15 min after anastomoses. On the 7th postoperative day, the anastomosed vessels in Group I showed the highest patency rate (93%). Anastomosed vessels in Group II, III and IV showed a patency rate of 67%, 73% and 87%, respectively.
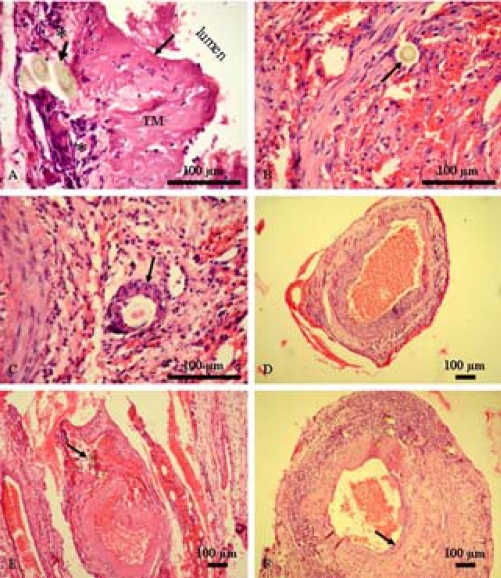
Histopathology
The histopathology examination of the anastomosed vessels showed considerable variations between the different suture techniques (Table 1). Vessels anastomosed using the simple interrupted suture showed the most pronounced histopathological changes compared with the other techniques. Generally, these histopathological changes included endothelial injury (Fig. 2A), endothelial proliferation (Fig. 2F), medial vacuolation and necrosis (Fig. 2A), the presence of suture materials either in the wall (Fig. 2A) or in the lumen of blood vessels (Fig. 2B) and a slight to moderate inflammatory reaction, particularly around the suture materials (Fig. 2C). There was also slight to moderate narrowing of the lumen of the anastomosed vessels in Group II, III and IV (Fig. 2D, E & F).
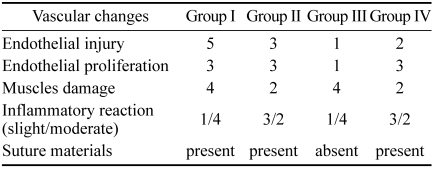
Table 1.
The pathological findings observed after femoral artery anastomosis using the different suture techniques
*Group I: simple interrupted suture, Group II: continuous suture, Group III: sleeve suture, Group IV: cuff suture.
Fig. 2.
Histopathological findings after an anastomosis of the femoral arteries using the different suture techniques. (A) Simple interrupted suture; Longitudinal section showing a loss of endothelial cells (thin arraow), vacuolated and necrosed tunica media (TM) and the presence of suture materials (thick arrow) surrounded by inflammatory cells (asterisk). (B) Simple interrupted suture; Transverse section showing suture materials in the lumen (arrow) surrounded by endothelial cells. (C) Simple interrupted suture; Transverse section showing an inflammatory cellular reaction surrounding the suture material (arrow). (D) Continuous suture; Transverse section showing slight narrowing of the lumen. (E) Sleeve suture; Transverse section showing narrowing of the lumen and the presence of suture materials in the wall (arrow). (F) Cuff suture; Transverse section showing slight narrowing of the lumen and endothelial proliferation (arrow). H&E stain.
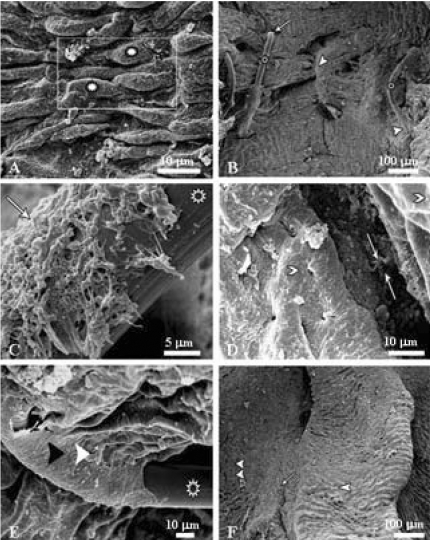
Scanning electron microscopy
The endothelial lining of the normal femoral artery appeared to be formed of spindle-shaped cells with a bulging central portion (Fig. 3A). According to the presence of suture materials inside the lumen of the sutured vessels, the microvascular anastomotic techniques were classified into intra-luminal and extra-luminal. The intra-luminal sutures showed the presence of suture materials in the lumen of the vessels sutured with the simple interrupted, continuous and cuff suture techniques with entrance and exit holes (Fig. 3B). Moreover, a fibrin network was observed around the entrance and exit sites (Fig. 3C). A gap between the two arterial ends (Fig. 3D) and signs of regeneration consisting of re-endothelialization (Fig. 3E) were also observed. On the other hand, the extra-luminal type was observed only with the sleeve suture technique with no suture materials in the lumen, no intimal damage and no fibrin network (Fig. 3F).
Fig. 3.
Scanning electron micrographs after femoral artery anastomosis using the different suture techniques. (A) Normal femoral artery showing spindle-shaped endothelial cells (asterisk). (B) Simple interrupted suture showing suture threads (asterisk), intimal holes (arrow) and signs of regeneration (arrowhead). (C) Simple interrupted suture showing fibrin network (arrow) partially covering the suture thread (asterisk). (D) Continuous suture showing a gap filled with fibrin between the two arterial ends (arrows) and normal endothelium at both sides (arrowheads). (E) Simple interrupted suture showing signs of regeneration consisting of endothelial cells (arrowhead) covering the suture thread (asterisk). (F) Sleeve suture showing the proximal (arrowhead) and distal (double arrowhead) segments with neoendothelization (arrow).
Discussion
The most important clinical requirements for successful microvascular anastomosis are a short anastomotic time, reduced blood leakage and high patency rate [16]. In this study, the continuous suture technique saved considerable anastomotic time compared with the simple interrupted suture. The fast speed in performing the suture technique is advantageous in reducing the level of tissue anoxia, trauma to the vessel wall and tissue desiccation [12]. Moscona and Owen [14] and Chen et al. [3] reported that a simple continuous suture technique could save 50% of the anastomotic time in 0-8 mm diameter arteries in an end-to-end anastomosis and vein graft interposition, respectively, when compared with the simple interrupted technique. Regarding the other two suture techniques, Lauritzen and Bagge [11] and Hung et al. [8] reported respectively, that the time needed to perform an end-to-end anastomosis using sleeve and cuff suture technique was significantly shorter than the interrupted suture technique, which is in accordance with the current results.
None of the anastomosed vessels showed grade III anastomotic leakage regardless of the technique used. On the other hand, 60% of the anastomosed vessels using the simple interrupted suture showed grade II blood leakage, which was stopped by gentle pressure compared with 33%, 27% and 40% for the continuous, sleeve and cuff suture techniques, respectively. Chen et al. [3] also reported that a lower percentage of rat femoral arteries anastomosed using the continuous suture technique showed blood leakage compared with the case treated using the simple interrupted suture. Lauritzen [10] and Hung et al. [8] observed that the simple interrupted suture showed considerable leakage compared with the sleeve and cuff suture in anastomosed rat vessels, respectively.
The patency of the anastomosed vessels is the most important criterion for a successful outcome. Similar to the results reported by Chen et al. [3], the present study showed a 100% patency for the different suture techniques at 5 and 15 min after the anastomoses, which excluded technical errors that usually appear during that early period. On the other hand, the patency rate for the simple interrupted suture technique one week after the anastomoses was higher than the other three suture techniques. This is in agreement with the results reported by Cobbett [5] and Tetik et al. [18], who showed that the simple interrupted suture technique yielded a higher patency rate than the continuous silk suture in an anastomosing aorta and femoral arteries in rats, respectively. Narrowing of the anastomotic site and the greater amount of suture materials that come in contact with the blood stream may underlie the lower patency produced by the simple continuous suture. Similarly, Sully et al. [17] reported that the patency rate of sleeve anastomosis in a series of femoral arteries in rabbits was significantly lower than that achieved using the conventional end-to-end anastomosis.
Regarding the cuff suture technique, these results are in agreement with those reported by Hung et al. [8], who did not observed any significant difference in immediate and late patency between the simple interrupted suture and cuff suture. Although there was some degree of endothelial proliferation in that technique, it did not affect the patency rate even though this pathological finding would be expected if even a trivial endothelial injury occurs. Harris et al. [7] showed high patency rates in 0.8-1 mm rat femoral arteries with only four sutures and cuff technique. In the small vessels, Kanajia [9] reported that the cuff technique was superior to the simple interrupted suture because it produced 98% patency in 0.5 mm vessels compared with the interrupted technique (0% patency). It is believed that the patency rate depends not only on the technique or the degree of the endothelial injury but also on the surgeon's competence, vessel size, size matching of the two vessel ends, and the coagulation cascade stimulation.
Pathological changes, particularly thromboses, are significant risks accompanying microvascular anastomosis [4]. This study showed that the simple interrupted suture produced considerable pathological changes compared with the other suture techniques. Pathological alterations due to the simple interrupted suture have been reported in anastomosed rabbit femoral arteries, and are manifested by endothelial loss and necrosis of the tunica media and tunica adventitia [13]. Acland and Trachtenberg [1] attributed the intimal damage to mechanical trauma and wound irritants that may be toxic to the endothelial lining. Moreover, Schubert et al. [15] reported that needle stitch trauma and intraluminal suture potentially cause vascular wall damage, thrombosis and intimal hyperplasia in a simple interrupted suture. There was less pathology produced by the simple continuous suture than with the simple interrupted suture. This can explain the short anastomotic time with the consequently less ischemia produced by the clamps. With the exception of marked luminal stenosis, which decreased gradually as a result of medial atrophy of both vessels, the sleeve suture technique showed moderate pathological changes. Wieslander and Aberg [19] reported that an end-in-end microvascular anastomosis resulted in considerable luminal stenosis in the central arteries of the ear of a rabbit. The present study showed that the cuff suture technique had a lower frequency of pathological changes. Hung et al. [8] also reported only slight changes between the two overlapping vessels in the cuff suture. As with the continuous and sleeve sutures, the cuff suture produced minimal stenosis. Consistent results were reported by Schubert et al. [15] in chicken jugular veins anastomosed using the modified cuff technique.
In conclusion, regardless of the pathological changes that healed correctly after anastomosis, this study recommends the simple interrupted suture for anastomosing arteries with a diameter of 0.8-1.0 mm because it showed the highest patency rate, which is the essential criterion that guarantees a successful anastomosis compared with the other techniques. Sleeve and cuff suture techniques might be successful alternatives for a conventional interrupted suture based on the short anastomotic time and moderate pathological changes.
Acknowledgments
The authors wish to thank Prof. Salah H. Afifi, Department of Pathology, Faculty of Veterinary Medicine, Assiut University for proof reading this manuscript.
References
- 1.Acland RD, Trachtenberg L. The histopathology of small arteries following experimental microvascular anastomosis. Plast Reconstr Surg. 1977;60:868–875. doi: 10.1097/00006534-197712000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Bancroft JD, Stevens A. Theory and Practice of Histological Techniques. 3rd ed. Edinburgh: Churchill Livingstone; 1990. pp. 113–305. [Google Scholar]
- 3.Chen YX, Chen LE, Seaber AV, Urbaniak JR. Comparison of continuous and interrupted suture techniques in microvascular anastomosis. J Hand Surg [AM] 2001;26:530–539. doi: 10.1053/jhsu.2001.22933. [DOI] [PubMed] [Google Scholar]
- 4.Ching S, Thoma A, Monkman S, Kelton JG. Inhibition of microsurgical thrombosis by the platelet glycoprotein IIb/IIIa antagonist SR121566A. Plast Reconstr Surg. 2003;112:177–185. doi: 10.1097/01.PRS.0000066171.65354.AE. [DOI] [PubMed] [Google Scholar]
- 5.Cobbett J. Small vessel anastomosis. A comparison of suture techniques. Br J Plast Surg. 1967;20:16–20. doi: 10.1016/s0007-1226(67)80003-1. [DOI] [PubMed] [Google Scholar]
- 6.Furka I, Brath E, Nemeth N, Miko I. Learning microsurgical suturing and knotting techniques: comparative data. Microsurgery. 2006;26:4–7. doi: 10.1002/micr.20201. [DOI] [PubMed] [Google Scholar]
- 7.Harris GD, Finseth F, Buncke HJ. The microvascular anastomotic autogenous cuff. Br J Plast Surg. 1981;34:50–52. doi: 10.1016/0007-1226(81)90097-7. [DOI] [PubMed] [Google Scholar]
- 8.Hung LK, Au KK, Ho YF. Comparative study of artery cuff and fat wrap in microvascular anastomosis in the rat. Br J Plast Surg. 1988;41:278–283. doi: 10.1016/0007-1226(88)90112-9. [DOI] [PubMed] [Google Scholar]
- 9.Kanaujia RR. Micro-arterial anastomosis using only two sutures and an autogenous cuff. J Hand Surg [Br] 1988;13:44–49. doi: 10.1016/0266-7681_88_90050-2. [DOI] [PubMed] [Google Scholar]
- 10.Lauritzen C. A new and easier way to anastomose microvessels. An experimental study in rats. Scand J Plast Reconstr Surg. 1978;12:291–294. doi: 10.3109/02844317809013008. [DOI] [PubMed] [Google Scholar]
- 11.Lauritzen C, Bagge U. A technical and biomechanical comparison between two types of microvascular anastomoses. An experimental study in rats. Scand J Plast Reconstr Surg. 1979;13:417–421. doi: 10.3109/02844317909013091. [DOI] [PubMed] [Google Scholar]
- 12.Lee BY, Thoden WR, Brancato RF, Kavner D, Shaw W, Madden JL. Comparison of continuous and interrupted suture techniques in microvascular anastomosis. Surg Gynecol Obstet. 1982;155:353–357. [PubMed] [Google Scholar]
- 13.Lidman D, Daniel RK. The normal healing process of microvascular anastomoses. Scand J Plast Reconstr Surg. 1981;15:103–110. doi: 10.3109/02844318109103422. [DOI] [PubMed] [Google Scholar]
- 14.Moscona AR, Owen ER. Continuous anastomotic technique in microsurgery. Isr J Med Sci. 1978;14:979–983. [PubMed] [Google Scholar]
- 15.Schubert HM, Hohlrieder M, Falkensammer P, Jeske HC, Moser PL, Kolbitsch C, Biebl M. Bipolar anastomosis technique (BAT) enables "fast-to-do", high-quality venous end-to-end anastomosis in a new vascular model. J Craniofac Surg. 2006;17:772–778. doi: 10.1097/00001665-200607000-00032. [DOI] [PubMed] [Google Scholar]
- 16.Simsek T, Eroglu L, Engin MS, Kaplan S, Yildiz L. End-to-end microvascular anastomosis in the rat carotid artery using continuous horizontal mattress sutures. J Reconstr Microsurg. 2006;22:631–640. doi: 10.1055/s-2006-956237. [DOI] [PubMed] [Google Scholar]
- 17.Sully L, Nightingale MG, O'Brien BM, Hurley JV. An experimental study of the sleeve technique in microarterial anastomoses. Plast Reconstr Surg. 1982;70:186–192. doi: 10.1097/00006534-198208000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Tetik C, Unal MB, Kocaoglu B, Erol B. Use of continuous horizontal mattress suture techniques in microsurgery: an experimental study in rats. J Hand Surg. 2005;30:587–595. doi: 10.1016/j.jhsa.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 19.Wieslander JB, Aberg M. Stenosis following end-in-end microarterial anastomosis: an angiographic comparison with the end-to-end technique. J Microsurg. 1982;3:151–155. doi: 10.1002/micr.1920030305. [DOI] [PubMed] [Google Scholar]