The purpose of this paper was to determine the dynamic pre- and postlens tear film thicknesses by using optical coherence tomography (OCT). We found that ultrahigh-resolution OCT is a promising tool for measuring the tear film.
Abstract
Purpose.
To determine the dynamic pre- and postlens tear film (PLTF and PoLTF) thicknesses by using optical coherence tomography (OCT).
Methods.
Ultrahigh-resolution OCT was used to image the tear film of 22 subjects before and after contact lens wear. A soft lens with 1 drop of artificial tears on its concave surface was inserted onto one randomly selected eye. OCT images were taken before insertion, immediately afterward, and every 2 minutes for 10 minutes. For the contralateral eye, the lens inserted was not prewetted on the concave surface. OCT images were taken before insertion, immediately afterward, and at 3 minutes. Then another drop was instilled, and images were taken immediately afterward and every 2 minutes for 10 minutes. Images were processed by custom software to yield tear film thickness.
Results.
The thickness of precorneal tear film (PCTF) was 1.9 ± 0.9 μm. The PoLTF was visualized clearly in all cases immediately after lens insertion, with 1 drop on the lens concave surface. Through the first 6 minutes after insertion, the PoLTF was greater than the PCTF. The PLTF (n = 12) and PoLTF (n = 9) were visualized immediately after lens insertion. After 3 minutes, the PLTF in most subjects and PoLTF in all subjects were invisible. The thickness of the PLTF increased after the instillation of artificial tears, whereas the PoLTF did not at any checkpoint for 10 minutes.
Conclusions.
Ultrahigh-resolution OCT is a promising tool for measuring the tear film. The PoLTF did not increase after instillation of artificial tears.
Determining the thickness of the precorneal, prelens, and postlens tear films (PCTF, PLTF, and PoLTF) is indispensable for understanding the normal physiology of the tear film and the etiology of dry eye associated with contact lens wear. More than 50% of contact lens wearers experience ocular dryness and discomfort, and some of them abandon lens wear, as intolerable dry eye symptoms affect daily life.1,2 The continuous exchange of the tears underneath the contact lens is needed for maintaining ocular health. Accordingly, the PoLTF is considered to be largely responsible for contact lens–associated dry eye, although the PLTF also contributes to it.3 Therefore, the measurement of the tear film thickness on and underneath the contact lens should be addressed. Some instruments can measure the thickness of the PCTF, PLTF, and PoLTF with good precision.4–11 However, direct cross-sectional visualization of the tear film may provide a better understanding of its role in contact lens fitting and interaction of the lens with the ocular surface.
Technological advancements in optical coherence tomography (OCT) have now made it possible to use ultrahigh-resolution (∼3 μm) spectral domain-OCT (SD-OCT) to image the tear film on contact lenses in situ.3 Thus, any tear film thicker than 3 μm theoretically can be detected. Although change in tear film are important in evaluating the fit of the contact lens on the cornea, not much information is available regarding the dynamic changes in the PLTF and PoLTF. Bruce et al.,11 King-Smith et al.,6 and Nichols et al.12–15 investigated the PCTF, PLTF, and PoLTF using interferometric methods. However, these methodologies cannot capture two-dimensional images of the anterior segment of the eye, nor can they directly visualize the tear layers on and underneath the contact lens. The goals of the present study were to use direct or indirect measurements by ultrahigh-resolution OCT to visualize the PCTF, PLTF, and PoLTF and to investigate the dynamic changes in thickness after the instillation of artificial tears.
Methods
Subjects
This prospective study was approved by the research review board of the University of Miami. Informed consent was obtained from each subject in accordance with the tenets of the Declaration of Helsinki. During screening, slit lamp evaluation after fitting a study lens (−3.00 D; base curve: 8.6 mm; silicone hydrogel contact lenses, PureVision; Bausch & Lomb, Rochester, NY) was performed by one of the investigators (CQ) to confirm the lens fitting with a centration of less than 1 mm. After a screening test, 22 subjects (14 men and 8 women; mean ± SD age, 31.4 ± 6.6 years; range, 24–46) were selected. Twelve did not wear contact lenses, and 10 wore soft lenses. None of the subjects had a history of previously diagnosed dry eye or any current ocular or systemic diseases.
Ultrahigh-Resolution Spectral Domain OCT
To detect the micrometer-thin tear layers on the cornea and the contact lens, we constructed a custom-built, high-speed, ultrahigh-resolution SD-OCT3 and used it in the present study. Briefly, the image capture rate was 48 frames per second when a light source was used that had a center wavelength of 840 nm and a broad bandwidth at 100 nm. The source was connected with a telecentric light delivery system driven by an X-Y galvanometer scanner. The power of the incident light delivered into the anterior segment was adjusted to 750 μW. The scan width was up to 15 mm with a depth of 3 mm. In theory, this OCT system has a ∼3-μm depth resolution in tears or tissues of the eye.3 The repeatability of the system was tested for the measurement of soft contact lenses. Five soft contact lenses with the same parameters as those for the lenses used in this study were immersed in a wet cell and imaged by OCT two times, with approximately a 5-hour interval between the two measurements. Three measurements of the central thickness were averaged. The repeatability was defined as the SD of the differences between the two measurement sessions in each lens. The repeatability was 0.92 μm.
The images captured by the camera were delivered to a computer workstation for processing and display. The light delivery system was mounted on a standard slit lamp that also incorporated a digital video system in the viewer. The subjects were asked to sit in front of the slit lamp and look forward horizontally. The room light was dimmed to avoid reflex tearing that might influence the results.
Experimental Procedure
The study was conducted in a consulting room with controlled temperature (15–25°C) and humidity (30%–50%). All subjects were scheduled after 10 AM to avoid the edematous cornea and the alteration of the tear film induced by sleep that might affect the result of the study.16,17 The corneal image, including the micrometer-thin tear film, of a randomly chosen initial eye was taken as the baseline in an 8-mm-width scan on the horizontal meridian with ultrahigh-resolution SD-OCT. Before insertion of a soft contact lens, 1 drop (35 μL) of artificial tears (Refresh Liquigel; Allergan, Irvine, CA) was instilled on the concave surface, and the lens was inserted on the eye. The anterior segment of the eye with the contact lens was imaged immediately after lens insertion and centration verification. It was then imaged again every 2 minutes for 10 minutes. Each image was taken after good centration verification. After that, the contact lens was removed, and 1 drop of artificial tears was instilled on the cornea so that it could be reimaged to obtain the true corneal thickness. This value was used to indirectly calculate the thickness of the PCTF and PoLTF.7,8 The subject was permitted to have a 5-minute rest to reduce the risk that manipulation of the initial eye would influence the contralateral eye.
After the 5-minute rest period, the baseline image of the contralateral eye was taken. Another silicone hydrogel contact lens with the same specification was then inserted onto this eye; however, for the second eye, no drop of artificial tears was placed on the concave surface of the lens before insertion onto the eye. The OCT images were taken immediately afterward and again 3 minutes later. A drop of artificial tears (35 μL) was then instilled on the eye with the contact lens fixed on the ocular surface. OCT images were again taken immediately after instillation and every 2 minutes for 10 minutes. The lens was then removed, and the same procedure that was performed on the initial eye was again used to obtain the true corneal thickness of the contralateral eye.
After the lenses were removed, they were soaked in the contact lens solution and imaged by OCT to obtain the lens thickness. This value was used to calculate the PLTF indirectly.7
PCTF, PLTF, and PoLTF Measurements
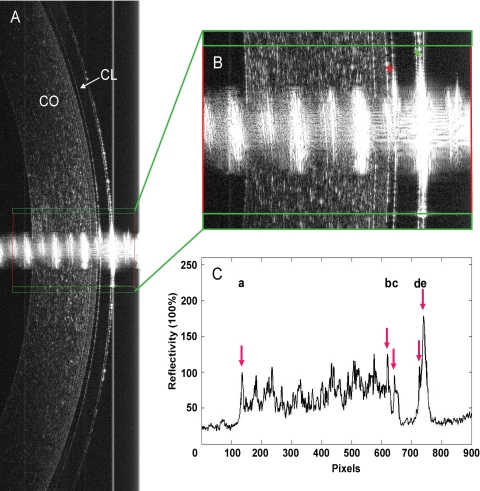
Commercial software (MATLAB; ver. 7.1; The MathWorks, Inc., Natick, MA) was used to perform the image processing and obtain the thickness of the PCTF, PLTF, PoLTF, contact lens, and central cornea (Fig. 1). The disturbance of the central specular hyperreflective reflex of each image was avoided by removing the central 50 axial scans (0.30-mm width). After that, 10 axial scans on each side of the central specular reflex were processed to yield OCT sagittal reflectivity profiles from the posterior surface of the cornea to the anterior surface of the PLTF (Figs. 1A–C). A low-pass signal filter was used to reduce the noise and smooth the reflectivity profile. The boundaries for tear film, contact lens, and cornea were identified by the peaks of the reflectivity profiles (Fig. 1C). The thickness of each layer equaled the distance in pixels between the corresponding two peaks. As shown in the magnified image (Fig. 1B), the PLTF, PoLTF, soft contact lens, and cornea were visualized clearly after lens insertion with 35 μL artificial tears on the concave surface. In the reflectivity profile, five sharp peaks were obtained, which are respectively labeled a through e, from left to right (Fig. 1C). Thicknesses of the PLTF, PoLTF, soft contact lens, and cornea, measured in pixels, were easily obtained. The tear film thickness in micrometers was then calculated by using a factor of 1.13 with the refractive index of tears as 1.343.18
Figure 1.
Image processing of ultrahigh-resolution OCT images of PLTF and PoLTF over the central location. (A, B) Immediately after a lens was inserted with 35 μL artificial tears on the concave surface, the PLTF (green *) and PoLTF (red *), soft contact lens (CL), and the cornea (CO) were clearly imaged. The central 50 axial scans (0.30 mm width) of the central specular hyperreflective reflex were removed. Ten axial scans on each side of the specular reflex were then used to yield OCT longitudinal reflectivity profiles from the posterior surface of the cornea to the anterior surface of the PLTF. (C) Processing of the image produced peaks a, the posterior surface of the cornea; b, the anterior surface of cornea or posterior surface of PoLTF; c, the anterior surface of the PoLTF or the posterior surface of the contact lens; d, the anterior surface of the contact lens or the posterior surface of PLTF; and e, the anterior surface of the PLTF. The thickness of each layer was calculated by determining the number of pixels between each two peaks and then converting them to micrometers by the factor 1.13.
However, at some points, the tear film on the cornea and the contact lens could not be visualized, because it was too thin to detect. To obtain the exact thickness of these invisible tear layers that actually existed, we used an indirect calculation. Before lens insertion, the thickness of central cornea plus the PCTF (C1) was measured. Then, the instillation of 1 drop of artificial tears outlined the cornea in images obtained by SD-OCT, so that the true central cornea thickness (C2) was obtained. Thus, the PCTF thickness was calculated as C1 − C2. The calculations for the PLTF and the PoLTF thicknesses were based on the same principle. The true thickness of the contact lens (L2) was determined from the image taken after the lens was soaked in the contact lens solution. This thickness was subtracted from the central lens thickness (L1) that included the PLTF measured during lens wear, giving the PLTF thickness as PLTF = L1 − L2. The thickness of the true cornea plus the PoLTF (C3) was measured in vivo, and consequently the PoLTF thickness was calculated as C3 – C2. As with the direct calculations of thicknesses, indirectly calculated thicknesses were initially measured in pixels and then converted to micrometers by the multiplication factor of 1.13.
Data Analysis
Paired t-tests were used for the comparison of tear film thickness between the right and left eyes at baseline. Repeated-measurements analysis of variance (Re-ANOVA) was performed to determine whether there were differences in the tear film thicknesses among the different time points. Post hoc tests were used to compare the tear film thickness between any two time points. Data are presented as the mean ± SD for all the variables at each time point. P < 0.05 was considered significant (all analyses: SPSS ver. 13.0; SPSS Inc., Chicago, IL).
Results
At baseline, there were no significant differences between the PCTF thickness in the right and left eyes (paired t-tests, P > 0.05); therefore, we averaged both PCTF thicknesses for each subject. The mean thickness of the PCTF at baseline was 1.9 ± 0.9 μm (range, 0.2–3.7 μm). After insertion of the contact lens, there were no significant differences at any of the 2-minute time points over 10 minutes in PLTF and PoLTF or the PCTF at baseline between non–contact lens wearers and experienced contact lens wearers (Re-ANOVA, P > 0.05).
Tear Film Thickness after Lens Insertion with 1 Drop of Artificial Tears Instilled on the Concave Surface
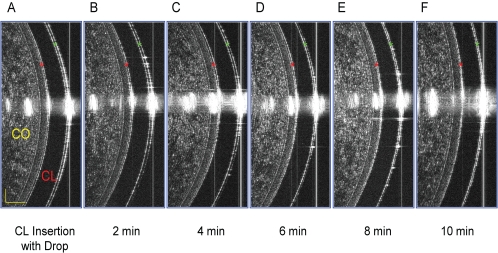
Both the PLTF and PoLTF were clearly evident and visualized immediately after lens insertion with 1 drop of artificial tears instilled on the concave surface in all subjects (Fig. 2A). Over the 10-minute period of observation, the PLTF decreased gradually with blinking (post hoc test, P < 0.05; Table 1, Figs. 2B–F, 3A). At each time point after lens insertion, except at 10 minutes, it was significantly greater than PCTF at baseline (post hoc test, P < 0.05; Table 1, Fig. 3A). Similarly, the PoLTF decreased continuously for 8 minutes after insertion (post hoc test, P < 0.05; Table 1, Figs. 2B–F, 3A). It was greater than the PCTF through the first 6 minutes after insertion (post hoc test, P < 0.05; Table 1; Fig. 3A). In six of the 22 subjects, the PoLTF was not detected after 2 minutes. In the others, it was visible for 4 (n = 5), 6 (n = 6), 8 (n = 2), and 10 (n = 3) minutes.
Figure 2.
Changes in PLTF and PoLTF after lens insertion with 1 drop of artificial tears on the concave side. (A) A soft contact lens (CL) was inserted onto the cornea (CO) with 1 drop (35 μL) of artificial tears on the concave surface of the lens. Both the PLTF (green *) and PoLTF (red *) were clearly visualized by SD-OCT immediately afterward. (B–F) After that, the PLTF and PoLTF gradually decreased. (F) At 10 minutes after lens wear, both the PLTF and PoLTF were still visible.
Table 1.
PCTF, PLTF, and PoLTF Thicknesses at Each Time Point
| Eye/Time Point | PCTF | PLTF | PoLTF |
|---|---|---|---|
| Initial eye* | |||
| Baseline | 1.7 ± 1.5 | ||
| CL insertion with drop | 18.5 ± 9.5 | 15.4 ± 9.0 | |
| 2 min | 12.6 ± 7.2 | 8.7 ± 4.8 | |
| 4 min | 8.2 ± 5.5 | 4.8 ± 2.9 | |
| 6 min | 6.0 ± 4.5 | 3.6 ± 1.9 | |
| 8 min | 4.6 ± 3.4 | 2.5 ± 2.1 | |
| 10 min | 3.2 ± 3.7 | 2.0 ± 2.2 | |
| Contralateral eye† | |||
| Baseline | 2.0 ± 1.5 | ||
| CL insertion | 6.0 ± 5.2 | 3.0 ± 2.1 | |
| 3 min | 2.3 ± 1.7 | 1.4 ± 1.5 | |
| Drop instillation | 29.5 ± 12.5 | 1.0 ± 1.2 | |
| 2 min | 15.1 ± 7.9 | 1.4 ± 1.4 | |
| 4 min | 9.5 ± 5.2 | 0.9 ± 1.2 | |
| 6 min | 7.3 ± 5.4 | 0.9 ± 1.1 | |
| 8 min | 5.3 ± 4.1 | 1.1 ± 1.1 | |
| 10 min | 4.3 ± 4.4 | 1.1 ± 1.0 |
Data are expressed as mean micrometers ± SD.
The concave surface of the contact lens contained a drop (35 μL) of artificial tears before lens insertion.
The contact lens was inserted onto the contralateral eye with no drop. Three minutes after lens insertion, 1 drop (35 μL) of artificial tears was instilled on the convex surface of the lens.
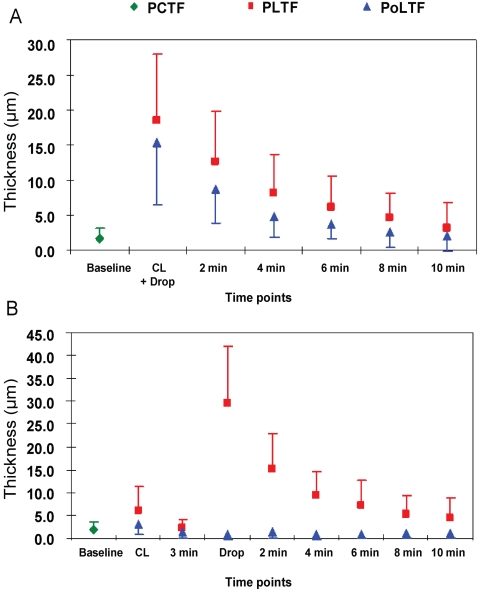
Figure 3.
Changes in PLTF and PoLTF after lens insertion. (A) 1 drop (35 μL) of artificial tears was placed on the concave surface of the lens before insertion. The PLTF and PoLTF were immediately increased compared with the precorneal tear film (PCTF, post hoc tests, P < 0.05). The PoLTF decreased continuously for the next 8 minutes (post hoc test, P < 0.05), and the PLTF decreased in a similar fashion (P < 0.05). (B) After lens insertion without prior application of a drop of artificial tears to the concave surface, the PLTF was immediately thicker than the PCTF at baseline (P < 0.05). However, the PoLTF was not different from the PCTF (P > 0.05). After 3 minutes of lens wear, both the PLTF and PoLTF decreased significantly compared with the moment of lens insertion (P < 0.05). When 35 μL artificial tears was instilled on the lens, the PLTF increased significantly and then decreased gradually in the following 8 minutes (P < 0.05). However, the PoLTF did not increase immediately after drop instillation and also did not change in the following 10 minutes (Re-ANOVA, P > 0.05).
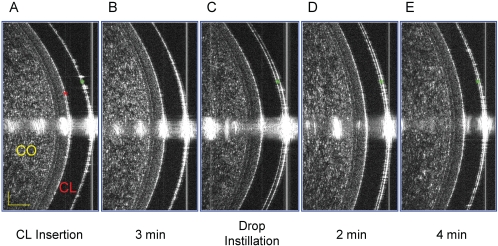
Tear Film Thickness after Lens Insertion with 1 Drop of Artificial Tears Instilled on the Convex Surface after 3 Minutes of Lens Wear
In the second eye in which the concave surface of the lens was not prewetted with artificial tears, the PLTF (n = 12) and PoLTF (n = 9) were visualized immediately on lens insertion on the cornea (Table 1, Figs. 3B, 4A). Three minutes later, the PLTF was still apparent in only two subjects, whereas the PoLTF was not apparent in any of the subjects, because it became too thin (Table 1, Figs. 3B, 4B). After instillation of a single drop of artificial tears, the PLTF clearly increased in thickness (post hoc test, P < 0.05; Table 1, Figs. 3B, 4C), but the PoLTF did not (post hoc test, P > 0.05; Table 1 Figs. 3B, 4C). After that, the PLTF gradually decreased in the following 8 minutes (post hoc test, P < 0.05, Table 1, Figs. 3B, 4D, 4E), but the PoLTF did not increase and remained undetectable (Re-ANOVA, P > 0.05; Table 1, Figs. 3B, 4D, 4E). The thinnest tear film directly detected by ultrahigh-resolution SD-OCT used in this study was 3.2 μm, which was very close to the 3-μm theoretical resolution in tears by the instrument.
Figure 4.
Changes in the PLTF and PoLTF after lens insertion followed by 1 drop of artificial tears on the convex surface of the lens. (A) A soft contact lens (CL) was inserted onto the cornea (CO) without the aid of the artificial tears. Immediately afterward, the PLTF (green *) and PoLTF (red *) were visualized by SD-OCT. (B) Three minutes later, the PLTF and PoLTF were no longer visible, as they became too thin. (C) One drop (35 μL) of artificial tears instilled onto the lens did not increase the PoLTF, whereas the PLTF was clearly increased immediately afterward. (D, E) In the following minutes, the PoLTF never increased sufficiently to become visible, and the PLTF decreased gradually with blinking.
Discussion
How to best measure the thickness of the PCTF, PLTF, and PoLTF is of considerable interest to clinicians and researchers; however, no agreement has been achieved regarding the optimal method. Doane9 developed a tear film interferometer that applied a contour plot to the measurement of the PLTF thickness. Fogt et al.10 used interferometry of spectral oscillations to determine the PLTF thickness. Bruce and Brennan11 and Bruce and Mainstone19 used biomicroscopy to observe the PoLTF in specular reflection. Prydal et al.5 found the PCTF thickness to be 34 to 45 μm by noninvasive interferometry and 41 to 46 μm by confocal microscopy. Wong et al.20 and Creech et al.21 obtained theoretical predictions of PCTF thickness as 8.0 and 10.4 μm, respectively. King-Smith et al.6 reported that the average thickness of the PCTF was 2.7 μm. Nichols and King-Smith22 found both PLTF and PoLTF to be 2.3 μm, when measured by interferometry. In contrast, Lin et al.23 reported a value of 11.5 μm for the PoLTF when determined by optical pachometry. Although the technologies and methods described above can be used to estimate tear film thickness with higher resolution than OCT, they cannot rapidly acquire large numbers of ultrahigh-resolution images that are necessary to precisely evaluate tear dynamics.
Commercial and custom-made OCT devices have been used to study many aspects of the ocular anterior segment such as the whole cornea, the epithelium, anterior chamber width, depth and angle, the flap after laser and others.24–28 The high resolution of the time domain OCT instrument, approximately 10 μm, made it useful to investigate the tear menisci and tear film.8,29 Wang et al.7,8 presented distinct images of the cornea, contact lenses, and tear film and reported PCTF, PLTF, and the PoLTF thicknesses of approximately 3.3, 3.8, and 4.6 μm, as determined by indirect calculation. Recent studies demonstrated that a high-resolution SD-OCT or an ultrahigh-resolution SD-OCT could obtain higher quality images and detect more details of the ocular anterior segment.30,31 Kaluzny et al.30 indicated that the high-resolution OCT instrument, with a 4- to 6-μm longitudinal resolution, was a promising device in contact lens research and practice. However, the tears on the contact lens surface were not included in their study, and tear films were not evident in their images. In a previous study, we used a custom-built, ultrahigh-resolution (∼3 μm) OCT instrument to precisely estimate tear menisci and tear films on and underneath contact lenses and to record the interaction between the lens edge and the ocular surface.3 In addition, we compared the fitting characteristics of two lenses with different materials, back curves, and edge designs and suggested that rational lens design might improve the fitting characteristics by improving tear exchanges around the lens edge. Therefore, the SD-OCT instrument was considered to be a promising tool for studying tear dynamics on the lens. However, because of the small subject sample in that study, conclusions regarding the true PLTF and PoLTF thickness were not drawn.
In the present study, we used ultrahigh-resolution SD-OCT and confirmed its theoretical depth resolution of 3 μm by visualizing a PLTF of 3.2 μm in one subject. As long as the tear film was thicker than 3.2 μm, it was detectable and calculated directly. In addition, the PoLTF was visualized and calculated directly immediately after lens insertion in some subjects, as suggested by Wang et al.3 To the best of our knowledge, this is the first time the PoLTF has been quantified directly from images without the aid of artificial tears. The increased tear film is mainly the result of reflex tearing,32 as we avoided applying soaking solution to the eye when the lens was inserted. In some subjects, there was no detectable increase in the PoLTF. This means only that the PoLTF did not exceed the 3-μm limit of resolution. It is possible that these subjects had poor sensitivity or good adaptability to soft contact lens wear and did not have any significant reflex tearing. Immediately after lens insertion or eye drop instillation, the PLTF and PoLTF were readily visualized. However, after 3 minutes of lens wear, they were not visible in most subjects. Thus, normally the PLTF and PoLTF during lens wear are too thin to be visible by ultrahigh-resolution OCT. The central thicknesses of the PCTF, PLTF, and the PoLTF were close to but a little thinner than those reported by King-Smith et al.,6 Nichols and King-Smith,22 and Wang et al.7 This slight difference may be due to the differences in sample size, the race of the subjects recruited, and the evident improvement of the longitudinal resolution of the instrument.
To investigate the effect of 1 drop on the PLTF and the PoLTF, we monitored these variables for 10 minutes after instillation on the lens. The results indicated that the lubricating drops used to improve ocular comfort during lens wear do not flow around the lens edge into the space between lens and cornea. Thus, the drops may relieve only the friction between eyelid and contact lens by increasing the PLTF. When the artificial tears were placed on the concave surface of lens before insertion, the PoLTF was readily apparent. However, it was quickly extruded by blinking. Thus, the PoLTF cannot be maintained during lens wear, even when extra tears are added.
The SD-OCT instrument used in the present study has opened a new era in the evaluation of the different fitting characteristics of various lens designs and materials.3 Our results suggest that soft contact lens design and materials must to be improved so that they hold the PoLTF and enhance the rate of tear exchange beneath the lens. Only in this way can the dry eye symptoms induced by contact lens wear be alleviated and the health of the ocular surface be sustained.3
In the present study, the measurements of the PCTF, PLTF, and PoLTF thicknesses were limited to the central location. Not much is known about the topographic thickness of the tear films away from the optical center; this subject will be explored in another study. The image processing of the tear films by manual manipulation and not by automated software may be another concern. We assumed that the thickness of the contact lens and the cornea used in the indirect calculations of tear films did not change during the approximately 10 minutes of lens wear. Any thickness changes in the lens and cornea that did occur could introduce measurement errors for the indirect calculations. In addition, lens decentration during imaging may be another concern. After fitting the lens on the eye, we used a slit lamp biomicroscope to evaluate the fitting, especially the centration. Good centration of less than 1 mm was achieved on each eye. Although we were aware of variation of the lens fitting during blinking, the images were taken during the first gaze. Slight decentration appeared not to have an impact on the direct visualization of the tear film; however, some variation may have been introduced into the indirect calculation. Using test lenses, we measured the variation of lens thickness. The variation of the central 1-mm zone was approximately 1.3 μm between the thinnest and thickest points. In an attempt to offset the systematic error due to decentration of the lens, we processed multiple A-scans along both sides of the apex to arrive at the results. Last, in this one-visit study, we defined normal healthy subjects as individuals without any previously diagnosed dry eye. We did not perform any tear function tests, like tear break-up time or the Schirmer test. The absence of testing may have allowed some undetected variation, if some of our subjects had subclinical dry eye. Further studies are needed to correlate the measurements with these tests.
In summary, the ultrahigh-resolution SD-OCT instrument is a novel and promising tool for evaluating the tear dynamics during contact lens wear. With this instrument, we have shown that the tears cannot be held underneath the soft contact lens, and extra lubricating drops used clinically for improving ocular comfort did not alter the PoLTF.
Acknowledgments
The authors thank Britt Bromberg, PhD, for providing editing services for this manuscript.
Footnotes
Supported by Research Grant R03 EY016420 and Center Grant P30 EY014801 from The National Institutes of Health/National Eye Institute, and by Bausch & Lomb, Allergan, and Research to Prevent Blindness.
Disclosure: Q. Chen, None; J. Wang, Bausch & Lomb (F), Allergan (F); A. Tao, None; M. Shen, None; S. Jiao, None; F. Lu, None
References
- 1.Caffery BE, Richter D, Simpson T, Fonn D, Doughty M, Gordon K. The prevalence of dry eye in contact lens wearers: part 2 of the Canadian Dry Eye Epidemiology study. Optom Vis Sci 1996;73:109 8927311 [Google Scholar]
- 2.Doughty MJ, Fonn D, Richter D, Simpson T, Caffery B, Gordon K. A patient questionnaire approach to estimating the prevalence of dry eye symptoms in patients presenting to optometric practices across Canada. Optom Vis Sci 1997;74(8):624–631 [DOI] [PubMed] [Google Scholar]
- 3.Wang J, Jiao S, Ruggeri M, Shousha MA, Chen Q. In situ visualization of tears on contact lens using ultra high resolution optical coherence tomography. Eye Contact Lens 2009;35(2):44–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prydal JI, Campbell FW. Study of precorneal tear film thickness and structure by interferometry and confocal microscopy. Invest Ophthalmol Vis Sci 1992;33(6):1996–2005 [PubMed] [Google Scholar]
- 5.Prydal JI, Artal P, Woon H, Campbell FW. Study of human precorneal tear film thickness and structure using laser interferometry. Invest Ophthalmol Vis Sci 1992;33(6):2006–2011 [PubMed] [Google Scholar]
- 6.King-Smith PE, Fink BA, Fogt N, Nichols KK, Hill RM, Wilson GS. The thickness of the human precorneal tear film: evidence from reflection spectra. Invest Ophthalmol Vis Sci 2000;41(11):3348–3359 [PubMed] [Google Scholar]
- 7.Wang J, Fonn D, Simpson TL, Jones L. Precorneal and pre- and postlens tear film thickness measured indirectly with optical coherence tomography. Invest Ophthalmol Vis Sci 2003;44(6):2524–2528 [DOI] [PubMed] [Google Scholar]
- 8.Wang J, Aquavella J, Palakuru J, Chung S, Feng C. Relationships between central tear film thickness and tear menisci of the upper and lower eyelids. Invest Ophthalmol Vis Sci 2006;47(10):4349–4355 [DOI] [PubMed] [Google Scholar]
- 9.Doane MG. An instrument for in vivo tear film interferometry. Optom Vis Sci 1989;66(6):383–388 [DOI] [PubMed] [Google Scholar]
- 10.Fogt N, King-Smith PE, Tuell G. Interferometric measurement of tear film thickness by use of spectral oscillations. J Opt Soc Am A Opt Image Sci Vis 1998;15(1):268–275 [DOI] [PubMed] [Google Scholar]
- 11.Bruce AS, Brennan NA. Clinical observations of the post-lens tear film during the first hour of hydrogel lens wear. Int Contact Lens Clin 1988;15(10):304–310 [Google Scholar]
- 12.Nichols JJ, Mitchell GL, King-Smith PE. Thinning rate of the precorneal and prelens tear films. Invest Ophthalmol Vis Sci 2005;46(7):2353–2361 [DOI] [PubMed] [Google Scholar]
- 13.Nichols JJ, King-Smith PE. The effect of eye closure on the post-lens tear film thickness during silicone hydrogel contact lens wear. Cornea 2003;22(6):539–544 [DOI] [PubMed] [Google Scholar]
- 14.Nichols JJ, King-Smith PE. The impact of hydrogel lens settling on the thickness of the tears and contact lens. Invest Ophthalmol Vis Sci 2004;45(8):2549–2554 [DOI] [PubMed] [Google Scholar]
- 15.Nichols JJ, Mitchell GL, King-Smith PE. The impact of contact lens care solutions on the thickness of the tear film and contact lens. Cornea 2005;24(7):825–832 [DOI] [PubMed] [Google Scholar]
- 16.Shen M, Wang J, Qu J, et al. Diurnal variation of ocular hysteresis, corneal thickness, and intraocular pressure. Optom Vis Sci 2008;85(12):1185–1192 [DOI] [PubMed] [Google Scholar]
- 17.Patel S, Bevan R, Farrell JC. Diurnal variation in precorneal tear film stability. Am J Optom Physiol Opt 1988;65(3):151–154 [DOI] [PubMed] [Google Scholar]
- 18.Lin RC, Shure MA, Rollins AM, Izatt JA, Huang D. Group index of the human cornea at 1.3-microm wavelength obtained in vitro by optical coherence domain reflectometry. Opt Lett 2004;29(1):83–85 [DOI] [PubMed] [Google Scholar]
- 19.Bruce AS, Mainstone JC. Lens adherence and postlens tear film changes in closed-eye wear of hydrogel lenses. Optom Vis Sci 1996;73(1):28–34 [DOI] [PubMed] [Google Scholar]
- 20.Wong H, Fatt I, Radke CJ. Deposition and thinning of the human tear film. J Colloid Interface Sci 1996;184(1):44–51 [DOI] [PubMed] [Google Scholar]
- 21.Creech JL, Do LT, Fatt I, Radke CJ. In vivo tear-film thickness determination and implications for tear-film stability. Curr Eye Res 1998;17(11):1058–1066 [DOI] [PubMed] [Google Scholar]
- 22.Nichols JJ, King-Smith PE. Thickness of the pre- and post-contact lens tear film measured in vivo by interferometry. Invest Ophthalmol Vis Sci 2003;44(1):68–77 [DOI] [PubMed] [Google Scholar]
- 23.Lin MC, Graham AD, Polse KA, Mandell RB, McNamara NA. Measurement of post-lens tear thickness. Invest Ophthalmol Vis Sci 1999;40(12):2833–2839 [PubMed] [Google Scholar]
- 24.Izatt JA, Hee MR, Swanson EA, et al. Micrometer-scale resolution imaging of the anterior eye in vivo with optical coherence tomography. Arch Ophthalmol 1994;112(12):1584–1589 [DOI] [PubMed] [Google Scholar]
- 25.Wang J, Fonn D, Simpson TL, Jones L. The measurement of corneal epithelial thickness in response to hypoxia using optical coherence tomography. Am J Ophthalmol 2002;133(3):315–319 [DOI] [PubMed] [Google Scholar]
- 26.Wang J, Thomas J, Cox I, Rollins A. Noncontact measurements of central corneal epithelial and flap thickness after laser in situ keratomileusis. Invest Ophthalmol Vis Sci 2004;45(6):1812–1816 [DOI] [PubMed] [Google Scholar]
- 27.Li Y, Shekhar R, Huang D. Corneal pachymetry mapping with high-speed optical coherence tomography. Ophthalmology 2006;113(5):792–799-e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldsmith JA, Li Y, Chalita MR, et al. Anterior chamber width measurement by high-speed optical coherence tomography. Ophthalmology 2005;112(2):238–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang J, Aquavella J, Palakuru J, Chung S. Repeated measurements of dynamic tear distribution on the ocular surface after instillation of artificial tears. Invest Ophthalmol Vis Sci 2006;47(8):3325–3329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaluzny BJ, Kaluzny JJ, Szkulmowska A, et al. Spectral optical coherence tomography: a new imaging technique in contact lens practice. Ophthalmic Physiol Opt 2006;26(2):127–132 [DOI] [PubMed] [Google Scholar]
- 31.Christopoulos V, Kagemann L, Wollstein G, et al. In vivo corneal high-speed, ultra high-resolution optical coherence tomography. Arch Ophthalmol 2007;125(8):1027–1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang J, Cox I, Reindel WT. Upper and lower tear menisci on contact lenses. Invest Ophthalmol Vis Sci 2009;50(3):1106–1111 [DOI] [PubMed] [Google Scholar]