Figure 12. Cellular Basis for Pulmonary Vascular Remodeling-lessons from hypoxia.
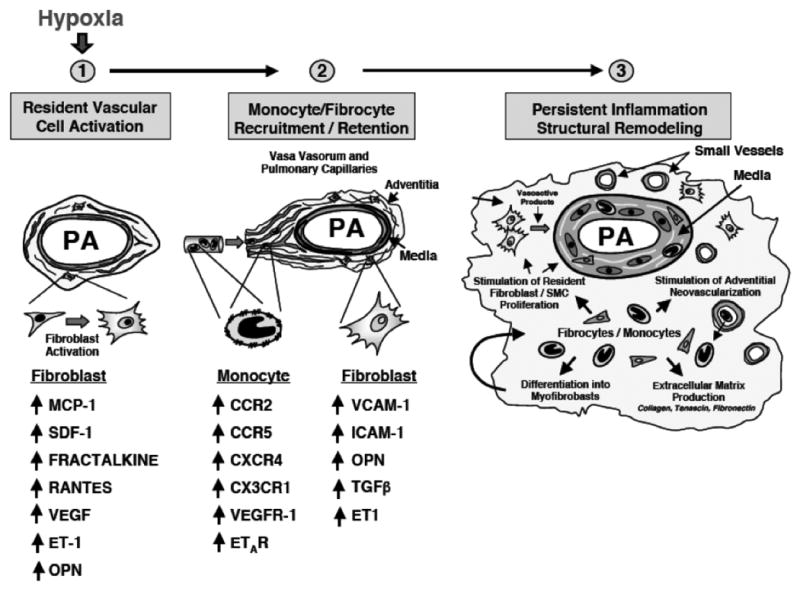
Fibroblasts, monocytes and fibrocytes play critical roles in orchestrating hypoxia-induced pulmonary vascular remodeling. Hypoxia or hypoxia-associated stimuli increase production by resident fibroblasts (and probably PASMC) of chemokines/cytokines including: monocyte chemoattractant protein (MCP)-1, stromal cell-derived factor (SDF)-1, fractalkine (CX3CL1), RANTES, VEGF, osteopontin (OPN) and endothelin. These and other factors stimulate recruitment of monocytes and monocyte-derived mesenchymal precursors (fibrocytes) to the vessel wall. Upregulation of monocyte receptors for these ligands (CCR2, CXCR4, CX3CR1, VEGFR-1 and ETR-A) occurs. Monocytes are retained in the vessel wall by the upregulation of adhesion molecules on fibroblasts, including vascular cell adhesion molecule (VCAM), intracellular adhesion molecule (ICAM) and OPN. As monocytes and fibrocytes accumulate in the vessel wall, they exert potent effects on the proliferative, migratory, matrix-producing and contractile capabilities of resident fibroblasts and PASMC through the secretion of TGF-β, PDGF-A and B, EGF, IL-6, IGF-1, MMP-9 and others. In addition, these cells produce potent proangiogenic molecules such as VEGF, S100A4, βFGF that likely play roles in stimulating further angiogenesis in the vessel wall.
Figure and legend contributed by Kurt Stenmark, University of Colorado at Denver.
