SUMMARY
We report an outbreak of hepatitis A that occurred in the city of Bari (Apulian region) in June 2002. Overall, 26 cases were observed over a 4-week period. These were traced back to the index case, a food handler who prepared various food products for sale over the counter at a store in the district (OR 5·36, CI 95% 1·58–19·25). Laboratory investigations confirmed that the outbreak was due to a point source and identified a new genotype IB variant. There is a possible indication for administration of hepatitis A vaccine to food handlers, although further evidence of an acceptable cost–benefit ratio needs to be ascertained.
INTRODUCTION
There has been a notable decline in the incidence of hepatitis A in Italy in recent years. Nevertheless, in some areas the endemic circulation of the virus has persisted at medium to high levels. In particular, in Apulia (a region in South-eastern Italy with 4 000 000 inhabitants), various epidemics have been recorded in the last few years, yielding a mean annual incidence of more than 20 cases/100 000 inhabitants. A widespread vaccination campaign was set up in 1997 targeting all infants, who should be vaccinated at 15–18 months, and adolescents, vaccinated at 12 years. Since that time, no new epidemics have occurred, although the disease is still endemic with a declining trend. Analyses conducted during the last epidemic demonstrated that the consumption of raw sea food played a predominant role in sustaining the spread of the disease, but it was difficult to document inter-human transmission. Nevertheless, person-to-person transmission, mediated by food vectors other than sea food, plays an important role in maintaining the high endemic level [1–3]. Moreover, it is essential to be able to determine all the main routes of transmission in order to plan the best means of disease prevention [4–7].
In this stable endemic scenario, on 19 June 2002 the Food Hygiene Service of the local health service unit notified the Regional Reference Centre of a suspected cluster of hepatitis A cases. The epidemic was observed in a district in Bari (quarter X) and mainly involved a group of workers in a services company.
MATERIALS AND METHODS
Epidemiological issues
Epidemiological surveillance was carried out by monitoring all hepatitis A notifications recorded in the infectious diseases on-line register (SIMI), as well as all hospital admissions for hepatitis A, in order to identify the cases and perform a descriptive analysis. In addition, active searches were set up to identify cases among residents in the area, through direct contact with the local general practitioners (GPs) in quarter X.
Cases were defined as those subjects with a clinical diagnosis of hepatitis A, together with laboratory confirmation of hepatitis A virus (HAV) IgM in acute phase sera.
The epidemiological investigation was conducted by direct interview of the cases using a standard questionnaire collecting detailed information on the patient’s personal data, date of symptom onset, and details of the symptoms, frequency of consumption and place of purchase of foods consumed in the 2–6 weeks before disease onset.
A case-control study was conducted to assess the risk factors for the disease and molecular tests were carried out on samples from the cases to identify the HAV strain responsible for the outbreak. All subjects responding to the definition of cases and resident or present for work purposes in quarter X were included in the investigation. The controls were healthy subjects working at the services company in question, and in another services company located in the same district, as well as all those cohabiting with cases but without contact with these two companies. All controls were HAV IgM negative and had normal hepatic enzymes.
Data collected from the SIMI database and hospital discharge records were integrated into a single archive using Epi-Info 6.04 software (CDC, Atlanta, GA, USA). Name and date of birth were used to exclude duplicated records.
The data collected in the study were stored and analysed with the statistical software packages Epi-Info 6.04 and Statview 5.0 for Macintosh (SAS Institute, Cary, NC, USA).
Statistical associations among the category variables under study were assessed with the χ2 test (values of P<0·05 were taken to be statistically significant); analysis of the risk factors was conducted by calculating the odds ratio (OR) and the respective 95% confidence intervals (CIs).
Laboratory issues
HAV IgM was detected by Axsym Microparticle MEIA (Abbott Diagnostics, Abbott Park, IL, USA). Viral nucleic acid extraction from stool samples and reverse transcriptase–polymerase chain reaction (RT–PCR) in the VP3–VP1 and VP1–P2A junctions was performed as described previously [8]. PCR products were purified using the QIAquick Purification kit (Qiagen S.p.A, Milan, Italy) and sequenced (ABI Prism 310; Applied Biosystems, Foster City, CA, USA). The relatedness of HAV RNA sequences isolated from the 14 specimens was assessed through multiple sequence alignment using the Clustal X program.
RESULTS
It was suspected that there might be a link between the outbreak and a probable index case, a food handler who had contracted hepatitis A and worked behind the counter at a grocery frequented by the employees of the company involved (store X).
However, it was not possible to draw up a detailed list of the products most frequently purchased at the store because all the subjects were not able to give precise details. The variable ‘has consumed food bought at store X’ was, therefore, used.
The epidemiological survey resulted in identification of the first 10 cases, aged between 25 and 35 years, among the services company workers. In all cases onset of symptoms had been observed between 4 and 22 June 2002. Two cases had been hospitalized. The most common symptoms were fever, asthenia and jaundice.
All cases volunteered that they had often consumed food supplied by store X in the 6 weeks before onset of the disease. The suspected index case was a 22-year-old who worked at the counter. He had presented with jaundice on 23 May 2002 and had been admitted to the Infectious Diseases ward. He had continued to work behind the counter up to this point.
The first cluster was followed by another 16 cases, identified by means of the hospital records. They had no relationship with the previous group but had developed hepatitis A in the same time interval (onset of symptoms between 10 and 26 June), lived or worked in the same district, and 12 (75%) had bought various food products at store X. Active surveillance through the GPs did not reveal any further cases.
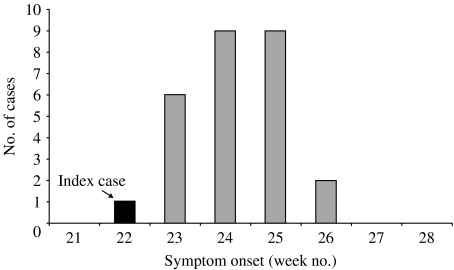
The cases had a mean age of 25 years (median 26 years) and 81% were male. The plot of the epidemic curve related to these 26 cases suggested a single source of exposure (Fig. 1).
Fig. 1.
Outbreak of hepatitis A detected in Bari during the period May–June 2002. ■, Index case (food handler).
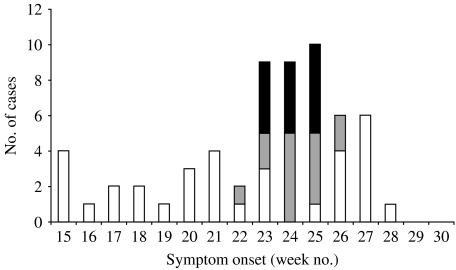
Data merging with the SIMI register demonstrated that the passive surveillance system had recorded an increase in the number of new cases in the four weeks of June and the first week of July, but had not indicated any particular outbreak peak. Instead, a peak was evident in the first three weeks of June when the other 13 cases, discovered during the active surveillance but never notified to SIMI, were included (Fig. 2). The controls were 51 selected healthy subjects.
Fig. 2.
Cases of hepatitis A notified in Bari during the period April–July 2002. □, Cases notified by routine passive surveillance system, not belonging to the outbreak;  , cases belonging to the outbreak (14) and notified by routine passive surveillance; ■, additional cases (13) detected by active surveillance.
, cases belonging to the outbreak (14) and notified by routine passive surveillance; ■, additional cases (13) detected by active surveillance.
The rate of infection in exposed subjects was found to be quite high, equal to nearly half of all the subjects who had consumed food from store X (22/45, 49%).
A significant association was found with the consumption of rolls prepared at the counter where the index case worked (OR 5·36, CI 95% 1·58–19·25, P=0·001). There was no association with exposure to other possible risk factors including consumption of sea food, meals at restaurants or a history of recent travel. No association between the water supply and cases was found. Moreover, the water supply was excluded as a source after checking with water company technicians, who declared that all routine quality controls on the distribution network were negative over that time period.
Stool or blood samples were collected from 20 patients (six employees of the service agency and another 14 cases) from 2 to 15 days after the onset of clinical symptoms (mean time 5 days). A stool specimen was also obtained from the presumptive index case (food handler) 3 weeks after hospitalization.
HAV RNA was detected in 65% (13/20, 12 faecal samples and one serum specimen) of available clinical samples and in the faecal sample taken from the food handler. The sequences of HAV cDNA from 11 out of 12 hepatitis A cases and from the food handler were identical over about 800 bases encompassing both VP3–VP1 and the VP1–P2A junctions. The nucleic acid sequences of HAV isolated from a case revealed a difference in 1 of 320 nucleotides in the VP3–VP1 junction and in 3 of 512 nucleotides in the VP1–P2A junction region and an overall similarity rate of 99·5% with the other strains of the outbreak.
All outbreak strains were assigned to subgenotype IB, which is not the most widespread in Southern Italy [8].
HAV sequence analysis of the samples from the cases including the food handler confirmed that the outbreak originated from a point source.
DISCUSSION
The outbreak we describe occurred in the context of a relatively stable endemic situation, which had shown a tendency to decline in the last few years [9].
First, the episode shows the need to improve the current surveillance system as 16 of the 26 cases would not have been linked with the index case. Only active surveillance and computer integration with the hospital discharge sheets brought the cluster to light and hence enabled suitable control measures to be adopted. It should be noted that non-immune subjects in contact with the cases were immunized post-exposure, which should have prevented more cases [10, 11].
The present study highlights the importance of investigating epidemic foci by sequence-based molecular methods, which can reliably supplement epidemiological information. Well standardized surveillance networks together with virological studies could help to better document outbreaks of hepatitis A and could provide useful information on the molecular epidemiology of HAV.
The demonstration of this route of transmission can also help explain the mechanisms that sustain the spread of the virus in this region [2, 9]. Therefore, some consideration of strategies for disease prevention seems justifiable in view of the food handler’s role [4–7, 12, 13].
Although the priority is to intensify the general control and prevention measures, the opportunities offered by vaccination in such cases should not be ignored. Having been relatively little studied as yet, the evidence for hepatitis A vaccination of all food handlers in terms of cost effectiveness is still not sufficiently strong [14].
Indeed, the problem of selective vaccination of high-risk groups has to be raised in the absence of a widespread vaccination strategy. Such a solution needs to be supported by careful local assessment of the costs and of the possibility of setting up alternative measures. Among these, it is important to include timely vaccination of the family contacts of cases [15]. Administration of hepatitis A vaccination to food handlers in areas with high circulation of the virus should, therefore, be considered.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Prikazchikov SA, Balayan MS. Shifts in the rates and levels of antibody to hepatitis A virus associated with hepatitis A infection in children’s communities. Eur J Epidemiol. 1987;3:370–376. doi: 10.1007/BF00145647. [DOI] [PubMed] [Google Scholar]
- 2.Jones AE, Smith JL, Hindman SH et al. Foodborne hepatitis A infection: a report of two urban restaurant-associated outbreaks. Am J Epidemiol. 1977;105:156–162. doi: 10.1093/oxfordjournals.aje.a112368. [DOI] [PubMed] [Google Scholar]
- 3.Hooper RR, Juels CW, Routenberg JA et al. An outbreak of type A viral hepatitis at the Naval Training Center, San Diego: epidemiologic evaluation. Am J Epidemiol. 1977;105:148–155. doi: 10.1093/oxfordjournals.aje.a112367. [DOI] [PubMed] [Google Scholar]
- 4.Perrett K. HNIG prophylaxis management of hepatitis A in a food handler at a London secondary school. Commun Dis Public Health. 2003;6:259. [PubMed] [Google Scholar]
- 5.CDC. Foodborne transmission of hepatitis A– Massachusetts, 2001. Morb Mortal Wkly Rep. 2003;52:565–567. [PubMed] [Google Scholar]
- 6.Nicholls M, Bruce M, Thomas J. Management of hepatitis A in a food handler at a London secondary school. Commun Dis Public Health. 2003;6:26–29. [PubMed] [Google Scholar]
- 7.Honish L, Bergstrom K. Hepatitis A infected food handler at an Edmonton, Alberta retail food facility: public health protection strategies. Can Commun Dis Rep. 2001;27:177–180. [PubMed] [Google Scholar]
- 8.Chironna M, Grottola A, Lanave C, Villa E, Barbuti S, Quarto M. Genetic analysis of HAV strains recovered from patients with acute hepatitis from Southern Italy. J Med Virol. 2003;70:343–349. doi: 10.1002/jmv.10402. [DOI] [PubMed] [Google Scholar]
- 9.Lopalco PL, Malfait P, Menniti-Ippolito F et al. Determinants of acquiring hepatitis A virus disease in a large Italian region in endemic and epidemic periods. J Viral Hepat. 2005;12:315–321. doi: 10.1111/j.1365-2893.2005.00593.x. [DOI] [PubMed] [Google Scholar]
- 10.Gustafson TL, Hutcheson RH, Jr, Fricker RS, Schaffner W. An outbreak of foodborne hepatitis A: the value of serologic testing and matched case-control analysis. Am J Public Health. 1983;73:1199–1201. doi: 10.2105/ajph.73.10.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Snydman DR, Dienstag JL, Stedt B, Brink EW, Ryan DM, Fawaz KA. Use of IgM-hepatitis A antibody testing. Investigating a common-source, food borne outbreak. J Am Med Assoc. 1981;245:827–830. [PubMed] [Google Scholar]
- 12.Hanrahan JP, Zimmerman KL, Toly MH, Prowda RL, Grabau JC, Morse DL. An outbreak of hepatitis A linked to a food handler in a cafeteria. NY State J Med. 1984;84:10–13. [PubMed] [Google Scholar]
- 13.CDC. Suspected hepatitis A in a food handler– California. Morb Mortal Wkly Rep. 1981;30:596–597. [PubMed] [Google Scholar]
- 14.Meltzer MI, Shapiro CN, Mast EE, Arcari C. The economics of vaccinating restaurant workers against hepatitis A. Vaccine. 2001;19:2138–2145. doi: 10.1016/s0264-410x(00)00396-0. [DOI] [PubMed] [Google Scholar]
- 15.Sagliocca L, Amoroso P, Stroffolini T et al. Efficacy of hepatitis A vaccine in prevention of secondary hepatitis A infection: a randomised trial. Lancet. 1999;353:1136–1139. doi: 10.1016/S0140-6736(98)08139-2. [DOI] [PubMed] [Google Scholar]