SUMMARY
The aim of this study was to determine whether a temporary rise in sexual risk behaviour during war in Guinea–Bissau could explain the observed trends in HIV-1 and HIV-2 prevalence, and to explore the possible contribution of competitive elimination of HIV-2 by HIV-1. A simulation model of the heterosexual transmission of sexually transmitted infections was parameterized using demographic, behavioural and epidemiological data from rural Guinea–Bissau, and fitted to the observed HIV-1 and HIV-2 trends with and without a historic rise in risk behaviour. The observed trends could only be simulated by assuming a temporary rise in risk behaviour. Around 30% of the projected decline in HIV-2 prevalence from a peak of 8·7% to 4·3% in 2010 was due to competitive elimination by HIV-1. Importantly for public health, HIV-1 prevalence was predicted to continue increasing and to become the dominant HIV type by 2010. Data collection is required to validate this prediction.
INTRODUCTION
In contrast to HIV-1, the spread of HIV-2 has been largely restricted to West Africa and countries with close historical links to Guinea–Bissau (e.g. Angola, Mozambique, Brazil) [1]. Guinea–Bissau has the highest HIV-2 prevalence worldwide (8%–10% in the general adult population) [2–4]. In recent years a decline in the prevalence of HIV-2 has been observed in most populations in West Africa including some communities in Guinea–Bissau [5–7]. HIV-2 prevalence decreased in men but not in women in a community study from urban Guinea–Bissau between 1987 and 1996 [8]. HIV-2 prevalence has also remained stable in a rural area in Guinea–Bissau (8·3% in 1990 vs. 7·9% in 1997; M. F. Schim van der Loeff, unpublished data).
At the same time, HIV-1 prevalence in Guinea–Bissau has risen from <0·5% in the late 1980s to around 2–3% 10 years later, suggesting an ongoing HIV-1 epidemic [5, 8, 9]. Differences in biology and viral load may explain the conflicting trends of HIV-1 and HIV-2 prevalence [10–12]. Heterosexual transmission of HIV-2 seems to be less efficient compared to HIV-1 [13, 14]. Further, progression to AIDS is slower in HIV-2- than in HIV-1-infected individuals [15–19].
It has been suggested that the exceptionally high prevalence of HIV-2 in Guinea–Bissau, especially in older age groups, may be due to increased promiscuity and commercial sex work during the war of independence between 1963 and 1974 [1, 20]. We used the microsimulation model STDSIM fitted to data from a rural area in Guinea–Bissau to (1) determine whether such a temporary increase in sexual risk behaviour can help explain the observed trends in HIV-1 and HIV-2 prevalence, and (2) explore the potential role of HIV-1 in reducing the prevalence of HIV-2 (competitive elimination).
METHODS
The microsimulation model STDSIM
We used the stochastic microsimulation model STDSIM, that simulates the natural history and the dynamics of the heterosexual transmission of HIV and other sexually transmitted infections (STI) in a dynamic population of interacting individuals [21]. Transmission of STI and HIV are simulated at the level of the sexual contact which can occur within steady and short-term relationships and as one-off contacts between males and commercial sex workers (CSWs) [22].
The natural course of infection of the modelled STI and of HIV-1 was divided, where appropriate, into different stages allowing variation in transmission probability and cofactor effects. These were previously validated by simultaneously fitting to data from three rural sites in sub-Saharan Africa [23]. HIV-2 was newly parameterized in this study. Chancroid and primary HSV-2 ulcers were assumed to enhance HIV-1 and HIV-2 transmission 25-fold, recurrent HSV-2 ulcers 10-fold, primary syphilis including periods without ulcers 7·5-fold, gonorrhoea and chlamydial infection 3-fold and trichomoniasis 2-fold [23]. A priori model input and output constraints were determined using data from a rural population in Guinea–Bissau and literature review. The model was fitted iteratively to these constraints. Results of 150 runs were averaged to account for the stochastic nature of the simulations. The time-frame of the simulation was from 1910 to 2010.
Model parameters
For the representation of HIV-1 we used fixed parameter values validated by previous modelling work on data from four populations in sub-Saharan Africa (Table 1) [24]. Parameters regarding HIV-2 infectivity and natural course of infection were estimated based on published data (Table 1). Based on estimates from a cohort study on CSWs in Dakar [13, 25], we assumed the ratio of HIV-2/HIV-1 infectivity was 1/4 (range 1/5 to 1/3). The HIV-2 transmission probability by stage was modelled to be proportional to HIV-1 transmissibility (Table 1). For both HIV-1 and HIV-2 the transmission probability from women to men was assumed to be half of the probability from men to women. Recent data showed no cross-immunity between HIV-1 and HIV-2. Therefore no interaction between HIV-1 and HIV-2 was modelled [5, 26–28].
Table 1.
HIV-1 and HIV-2 model input parameters with upper and lower limits
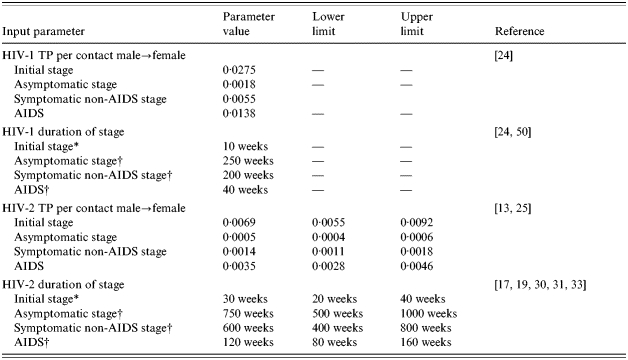
TP, Transmission probability.
Average duration, drawn from an exponential.
Average duration, drawn from a Weibull distribution (shape parameter=2).
Data on the duration of the different stages of HIV-2 infection (primary infection, asymptomatic/symptomatic non-AIDS stage, AIDS) are scarce, but progression to AIDS in HIV-2 seems very slow. Based on a CSW study from Dakar [29, 30], Anderson & May estimated an average incubation period of 30 years [31]. The risk of death attributable to HIV-2 found in cohort studies on seroprevalent cases with up to 9 years of follow-up was compatible with this estimate [17, 32]. We assumed that the average time from infection to death for HIV-2 was three times longer compared to HIV-1. Data also suggested that the HIV-2 AIDS stage may be up to three times longer than that of HIV-1 [19, 33]. For simplicity, we assumed each HIV-2 stage to be three times longer than the respective HIV-1 stage (Table 1). Therefore the ratio of the basic reproduction numbers in our model (R0,HIV-2/R0,HIV-1=0·75) was compatible with previous estimates (0·71) [31].
HIV-2 has been identified in a blood sample from Guinea–Bissau dating back to 1966 and may have been introduced as early as 1945 [34, 35]. We introduced HIV-2 into the model in 1950. In contrast, no HIV-1 infections were found in blood samples from several rural sites in Guinea–Bissau taken in 1980 and from Bissau in 1987 [17, 36]. In the study area, HIV-1 prevalence was 0·5% in 1990 [4]. Based on these data, the year of introduction of HIV-1 was assumed to be 1987.
Simulated population
The area for which HIV transmission was modelled consists of a set of 10 farming villages in the north-west of Guinea–Bissau. The characteristics of this population have been described [32]. The majority of the population belong to the Manjako ethnic group and is highly mobile. Many men outmigrate for work elsewhere in the region causing an adult male to female ratio of around 0·82 [37]. Women from the area form a significant proportion of prostitutes working in urban centres in Guinea–Bissau and neighbouring countries [32].
The demographic characteristics of the population were fitted to data from a survey carried out in 1997. The growth rate was 2·4% and the average life expectancy was 46 years as reported in census data from Guinea–Bissau (2000) [38].
The behavioural characteristics and HIV-1/HIV-2 prevalence were based on two cross-sectional studies carried out in the area in 1989–1991 and in 1997–1998 [27, 32]. To allow the comparison between the observed and simulated overall HIV-1 and HIV-2 prevalence, the simulated and the observed values were standardized using the age and sex distribution reported in the 1997 demographic survey.
Based on the field data, the average age of first sex was assumed to be 17·5 years for men and women. Studies across sub-Saharan Africa have shown that men and women may substantially misreport their sexual behaviour, with women potentially under-reporting and men over-reporting the number of recent partners [39, 40]. Thus, the proportion of men and women reporting more than one partner in the last 12 months was allowed to deviate downwards and upwards, respectively, relative to the observed data. In the area, men in polygamous unions may not have a sexual relationship with all of their spouses. Therefore we assumed the proportion of polygamous men was lower than the data suggest.
Data on which to base the quantification of commercial sex work in the area were limited. According to the 1997 study, up to 3% of women may have worked as a CSW at some point in their life, but there was no information on current CSW status. Based on the limited data we assumed that the majority of males did not visit CSWs (65%), or did so only once a year (31%). A smaller proportion of males (4%) visited CSWs nine times per year. CSWs were recruited from single and divorced females in the population according to male demand and serviced one partner per week to simulate low-level sex work assumed to be more prevalent in rural areas.
Modelling strategy
In the first scenario, the model was fitted to the increasing prevalence of HIV-1 between 1990 and 1997 using the a priori constraints on sexual behaviour. The simulated age and sex distribution of HIV-1 prevalence was fitted to the prevalence data from the cross-sectional study in 1997 by varying the age-specific rate of partner change within the predefined limits. Since HIV-1 was introduced in the late 1980s, this approach allowed us to simulate the conditions under which the HIV-1 epidemic occurred. We then used the model to estimate HIV-2 prevalence if these conditions had remained constant throughout the time-frame of the simulation.
To explore the hypothesis that a temporary rise in risk behaviour must have taken place to explain the observed high HIV-2 prevalence, a second scenario was modelled assuming an increase in risk behaviour from 1963 to 1974 contemporary with the war of independence. The sexual risk behaviour prior to 1963 and after 1974 was assumed to be similar. Since it has been suggested that HIV-1 may competitively replace HIV-2 [31], we repeated the second scenario without introducing HIV-1 to estimate the prevalence of HIV-2 if the HIV-1 epidemic had not occurred and therefore estimate the impact of the competitive elimination of HIV-2 by HIV-1.
Sensitivity analysis
To assess the robustness of the results to uncertainties in the HIV-2 transmission probability and the duration of infection, the scenario assuming no behaviour change and the scenario simulating behaviour change were repeated assuming the high and low values for each parameter shown in Table 1. Since there was also uncertainty regarding the simulated risk behaviour, we tested the sensitivity of the findings to changes in the number of male CSW visits per year in the high frequency group (6 or 12 visits per year resulting in a core group size of frequent CSW visitors of 8% or 2%, respectively). We explored whether a change in any of these parameters allowed fitting the model to the observed HIV-1 and HIV-2 prevalence without assuming a change in behaviour. The scenarios were refitted to the data by varying the overall risk behaviour within the predefined limits.
RESULTS
Simulated population characteristics
The simulated population provided a good fit to the age and sex distribution of the population in 1997 (not shown). In accordance with the data, the simulated adult male to female ratio was 0·85 resulting from substantial simulated outmigration of males older than 25 years. The simulated population consisted of around 22000 individuals of all ages in 1997.
As expected, to fit the observed HIV-1 prevalence by age and sex, we had to assume that the proportion of adults with more than one partner in the previous 12 months was higher than observed for females, but lower than observed for males (women: model 18%, data 3%; men: model 27%, data 41%). The proportion of women in steady relationships was slightly lower compared to the data (women: model 53%, data 66%), while in men it was somewhat higher (model 52%, data 42%). Also, we assumed a lower proportion of polygamous men compared to the data (model 8%, data 17%). In line with the data males were older than their female partners (4 years). The proportion of females recruited as CSW was 1·1%.
Simulated HIV-1 and HIV-2 prevalence
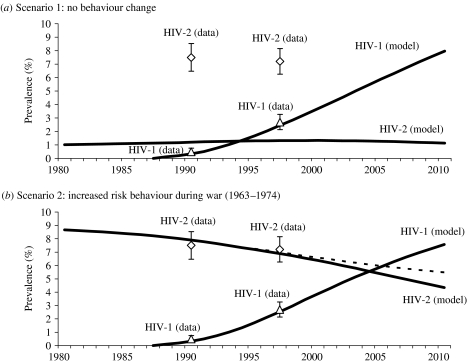
Figure 1(a) shows the simulated epidemic curve for HIV-1 fitted to the overall prevalence among ⩾15-year-olds in 1990 and 1997 assuming no change in sexual behaviour over time. In this scenario, HIV-2 prevalence would have reached 1·4% in 1997, much lower than the 7·2% observed.
Fig. 1.
Observed (with 95% CI) and simulated HIV-1 and HIV-2 prevalence among ⩾15-year-olds in (a) Scenario 1 (constant risk behaviour) and (b) Scenario 2 (behaviour change). All values standardized using the age and sex composition in 1997. Observed HIV-1 prevalence shown as triangles, observed HIV-2 prevalence shown as diamonds. The dashed line in Scenario 2 shows the HIV-2 prevalence trend in the absence of HIV-1.
Figure 1(b) shows the second scenario assuming higher risk behaviour between 1963 and 1974 (proportion with more than one partner in preceding 12 months: men 31%, women 21%; proportion of frequent visitors to CSW 8%, 2·2% of females recruited as CSW). In this scenario the prevalence of HIV-1 and HIV-2 was fitted well. The peak of the HIV-2 epidemic (8·7%) occurred in 1979, 5 years after the end of the simulated period of high-risk behaviour. HIV-2 declines from its peak of 8·7% to 4·3% in 2010 (a 51% relative decline), while HIV-1 prevalence rises to 7·6%. Repeating Scenario 2 without introducing HIV-1 (the dashed line) showed that in the absence of HIV-1 the prevalence of HIV-2 would decline from 8·7% in 1979 to 5·5% in 2010 (a relative decline of 37%). Therefore, the model predicts that between 1979 and 2010, around 70% of the expected decline in HIV-2 prevalence could be due to the historic change of risk behaviour, and around 30% due to competitive elimination by HIV-1.
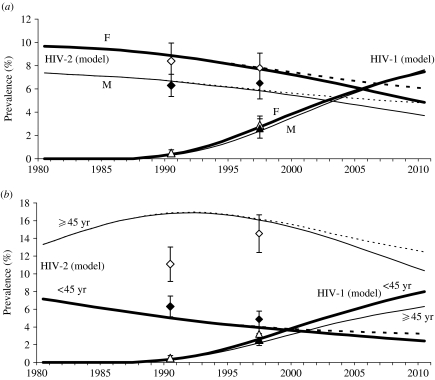
Figure 2 shows the observed and simulated HIV prevalence trends in Scenario 2 stratified by gender and by age (15–44 years and ⩾45 years). The model fitted the gender-specific HIV-1 and HIV-2 prevalences well and predicted similar prevalence trends for males and females after 1997 (Fig. 2a). The increasing HIV-1 prevalence in younger and older adults and the declining HIV-2 prevalence in younger adults were also fitted well by the model, but the HIV-2 prevalence among older adults in 1990 was not fitted by the model (Fig. 2b).
Fig. 2.
Observed (with 95% CI) and simulated HIV-1 and HIV-2 prevalence in Scenario 2 (behaviour change) stratified by gender (a) and age (b). All values standardized using the age and sex composition in 1997. Observed HIV-1 prevalence shown as triangles. Observed HIV-2 prevalence shown as diamonds. White markers show data on (a) females and (b) on adults aged ⩾45 years. Black markers show data on (a) males and (b) on adults aged 15–44 years. The dashed lines show the HIV-2 prevalence trends in the absence of HIV-1.
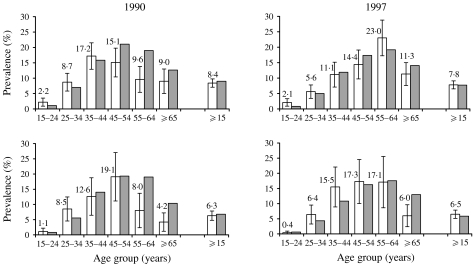
Further stratifications by age and gender for the years 1990 and 1997 are shown in Figures 3 and 4 confirming a good fit of the overall HIV-1 and HIV-2 prevalence in women and men in Scenario 2. The model overestimates the HIV-1 prevalence in women in the 25–34 years age group and underestimates HIV-1 in the 55–64 years age group (Fig. 3). The observed age distribution of HIV-1 prevalence in men is represented well by the simulation.
Fig. 3.
Observed (with 95% CI) and simulated prevalence of HIV-1 by age in 1997 in (a) women and (b) men. Data from 1990 survey not shown due to small numbers. □, Data; , model.
, model.
Fig. 4.
Observed (with 95% CI) and simulated prevalence of HIV-2 by age in 1990 and 1997 in women (top panels) and men (bottom panels). □, Data;
 , model.
, model.
In the model, the peak age of HIV-2 prevalence shifts from the 45–54 years age group in 1990 to the 55–64 years age group in 1997, suggesting a cohort effect of past HIV-2 infection (Fig. 4). A similar effect can be seen in the data, but appears less obvious for men than for women. The model overestimates HIV-2 prevalence in older men and women in 1990, and men aged ⩾65 years in 1997.
Sensitivity analysis
Assuming no change in behaviour (Scenario 1), the projected HIV-2 prevalence in 1997 was 1·6% if the ratio of HIV-2/HIV-1 infectivity was raised to 1/3. In all other simulations assuming no behaviour change, HIV-2 prevalence in 1997 was even lower (not shown).
The sensitivity analysis of Scenario 2 (increased risk behaviour 1963–1974) is shown in Table 2. Assuming a shorter duration of HIV-2 infection or a lower transmission probability resulted in an earlier peak and a steeper decline of HIV-2. Similarly, concentrating visits to CSWs in fewer men (12 visits per year in the highest visiting frequency group) resulted in an earlier peak of HIV-2 (1976), but the rapid decline of HIV-2 between 1990 and 1997 was not consistent with the observed prevalence trend. In this scenario, HIV-1 prevalence reaches a plateau at 4·9% in 2010. Assuming a larger group of males who visited CSWs less often, resulted in a good fit to the HIV-2 prevalence data, but this resulted in a very steep rise of HIV-1 to 13% in 2010. In all counterfactual scenarios without introducing HIV-1, the absence of HIV-1 resulted in a higher HIV-2 prevalence in 2010 (by +0·8% to +1·4%).
Table 2.
Sensitivity analysis of selected model parameters for Scenario 2 (behaviour change 1963–1974)
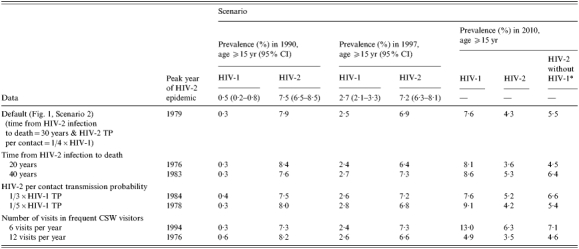
TP, Transmission probability; CSW, commercial sex workers.
Projected HIV-2 prevalence in 2010 without introduction of HIV-1.
DISCUSSION
The model supports the hypothesis that the high prevalence of HIV-2 found in Guinea–Bissau can be explained by a period of higher risk sexual behaviour during the war of independence between 1963 and 1974. It suggests that HIV-2 prevalence in rural Guinea–Bissau is about to decline as observed in some urban settings in this country [5, 8], and that this decline may have been hastened by the ongoing HIV-1 epidemic.
Apart from Guinea–Bissau high levels of HIV-2 outside risk groups have only been observed in war-affected regions in northern Angola (11·3% in pregnant women [41]), suggesting that a substantial penetration of HIV-2 into the general population occurs only if an existing HIV-2 endemicity combines with prolonged periods of social disturbance.
Our model prediction for the HIV-1 prevalence trend in rural Guinea–Bissau was consistent with the available data on pregnant women in the capital city Bissau which shows prevalence rising from <1% prior to 1993 to 2·5% in 1997 and 4·8% in 2000 [42]. Our study predicts that HIV-1 prevalence has continued to rise since 2000 and will continue to do so over the next few years. This contrasts with the most recent model predictions by UNAIDS, in which HIV-1 prevalence in adults was modelled to have stabilized at 3·8% between 2003 and 2005 [43]. However, data on pregnant women in Bissau have been unavailable after 2000 and therefore we cannot determine which of these contrasting model forecasts is more likely to be correct.
The model findings are limited by uncertainty regarding the duration of HIV-2 stages, HIV-2 transmission probability and sexual behaviour in the area. However, the sensitivity analysis revealed that even large changes in any of these parameters still required a period of higher risk behaviour in the past to explain the observed HIV-2 prevalence. Moreover, in all scenarios HIV-2 is projected to decline in the future, while HIV-1 shows a further increase. However, the peak year of the HIV-2 epidemic, the slope of its subsequent decline and the magnitude of the HIV-1 epidemic strongly depended on the size of the simulated core group of male CSW visitors, as well as on the assumed parameters for the transmission probability of HIV-2 and the duration of infection until death. Therefore, predictions of the future prevalence of HIV-1 and HIV-2 remain somewhat uncertain.
Further, the modelled and observed HIV prevalences were not always consistent. The model overestimated the HIV-2 prevalence in older individuals in 1990 which could be due to an overestimation of sexual risk behaviour in these age groups relative to younger age groups, or because the two samples in 1990 and 1997 were drawn from slightly different populations. The latter possibility is compatible with the large age-specific changes in HIV-2 prevalence in women between 1990 and 1997 and the known high mobility of the people living in the area [37].
We also predicted a slightly faster decline of HIV-2 prevalence between 1990 and 1997 than was observed, probably due to our simplified assumption of an abrupt reduction of risk behaviour in 1974. Assuming a more gradual decline in risk behaviour after 1974 would have resulted in a slower HIV-2 decline. The high prevalence of HIV-1 in the 55–64 years age group in women was also not well represented by the model. This observation from the data may be due to the high average age of active CSWs in the area [44] or to an increased susceptibility of post-menopausal women to HIV infection [8, 45, 46]. However, the current STDSIM model does not allow age-specific variations in susceptibility.
Finally, the model does not take into account non-sexual transmission routes that may explain the high HIV-2 prevalence in Guinea–Bissau. A recent study on elderly people in Bissau, the capital of Guinea–Bissau, found a moderate association between female circumcision, medical injections and HIV-2 infection [47], although an earlier study in Bissau failed to find an association between medical injections and HIV-2 infection [20]. Lifetime blood transfusions were a risk factor for HIV-2 infection in the 1990 survey conducted in the rural area on which our model was based (odds ratio 2·1) [4]. Therefore, the screening of blood supplies since 1987 may contribute to the decline of HIV-2 [8]. However, since blood transfusions were reported by only 2% of the study population [4], the population attributable fraction of HIV-2 infections preventable by blood screening is likely to be <4%. Our study cannot exclude the possibility that other routes of transmission may have contributed to the high HIV-2 prevalence in Guinea–Bissau, but it does show that a moderate rise in risk behaviour compatible with existing data is sufficient to explain the observed trends in HIV-1 and HIV-2 prevalence.
To our knowledge there is only one previous modelling study of HIV-1 and HIV-2 transmission. In 1996, Anderson & May used a deterministic model of HIV-1 and HIV-2 transmission in a randomly mixing population [31]. Assuming homogenous risk behaviour they predicted that HIV-1 may competitively replace HIV-2 within 200 years of the introduction of HIV-1, and that no significant impact on HIV-2 prevalence would be observed for at least 50 years. Our model that takes into account heterogeneity in risk behaviour, and therefore concentrates HIV-1 and HIV-2 among higher risk individuals, predicted that the effects of competitive elimination of HIV-2 by HIV-1 may happen more quickly.
The competitive elimination of HIV-2 by HIV-1 is due to the higher mortality in HIV-2-infected individuals who are also HIV-1 infected. The decrease of HIV-2 prevalence caused by HIV-1 also results in a lower HIV-2 incidence, especially since HIV-1/HIV-2 co-infection disproportionally affects sexually more active persons [27], who in the absence of HIV-1 may have continued to transmit HIV-2. In addition, HIV-1 indirectly lowers HIV-2 incidence by removing core group individuals from the population who drive the spread of classical STIs acting as cofactors for HIV-2 infection.
Our model suggests that around 70% of any decrease in HIV-2 prevalence in this part of rural Guinea–Bissau may be due to behaviour change and around 30% due to HIV-1. However, we assumed no intra-host competition between HIV-1 and HIV-2. There is some evidence that at low CD4 counts HIV-2 viral load may be lower in dually infected individuals than in those only infected with HIV-2 [48, 49]. Thus, dual infection could lead to a lower HIV-2 infectivity and a more rapid competitive exclusion of HIV-2. However, our model shows that ‘demographic’ elimination alone strongly impacts on HIV-2 prevalence.
In conclusion, our model confirms that the diverging trends of HIV-1 and HIV-2 prevalence in Guinea–Bissau can be explained by the combination of behaviour change after the war of independence and competitive elimination by HIV-1. While the exact future HIV prevalences remain uncertain, the public health burden of HIV-1 is likely to continue to increase relative to HIV-2 and it may become the dominant HIV type in Guinea–Bissau by 2010. Indeed, this may have already happened in younger age groups. Our analysis raises the possibility that HIV-1 prevalence in Guinea–Bissau may exceed that in neighbouring West African countries, where, with some exceptions, HIV-1 prevalence has remained <5%. Further data collection is required to validate this model prediction.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Schim van der Loeff MF, Aaby P. Towards a better understanding of the epidemiology of HIV-2. AIDS. 1999;13:S69–S84. (Suppl. A): [PubMed] [Google Scholar]
- 2.Norrgren H et al. HIV-1, HIV-2, HTLV-I/II and Treponema pallidum infections: incidence, prevalence, and HIV-2-associated mortality in an occupational cohort in Guinea-Bissau. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1995;9:422–428. doi: 10.1097/00042560-199508000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Poulsen AG et al. HIV-2 infection in Bissau, West Africa, 1987–1989: incidence, prevalences, and routes of transmission. Journal of Acquired Immune Deficiency Syndromes. 1993;6:941–948. [PubMed] [Google Scholar]
- 4.Wilkins A et al. The epidemiology of HIV infection in a rural area of Guinea-Bissau. AIDS. 1993;7:1119–1122. doi: 10.1097/00002030-199308000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Norrgren H et al. Trends and interaction of HIV-1 and HIV-2 in Guinea-Bissau, west Africa: no protection of HIV-2 against HIV-1 infection. AIDS. 1999;13:701–707. doi: 10.1097/00002030-199904160-00011. [DOI] [PubMed] [Google Scholar]
- 6.Peeters M et al. Genetic subtypes of HIV type 1 and HIV type 2 strains in commercial sex workers from Bamako, Mali. AIDS Research and Human Retroviruses. 1998;14:51–58. doi: 10.1089/aid.1998.14.51. [DOI] [PubMed] [Google Scholar]
- 7.Schim van der Loeff MF et al. Sixteen years of HIV surveillance in a West African research clinic reveals divergent epidemic trends of HIV-1 and HIV-2. International Journal of Epidemiology. 2006;35:1322–1328. doi: 10.1093/ije/dyl037. [DOI] [PubMed] [Google Scholar]
- 8.Larsen O et al. Declining HIV-2 prevalence and incidence among men in a community study from Guinea-Bissau. AIDS. 1998;12:1707–1714. doi: 10.1097/00002030-199813000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Poulsen AG et al. Prevalence of and mortality from human immunodeficiency virus type 2 in Bissau, West Africa. Lancet. 1989;1:827–831. doi: 10.1016/s0140-6736(89)92281-2. [DOI] [PubMed] [Google Scholar]
- 10.Andersson S et al. Plasma viral load in HIV-1 and HIV-2 singly and dually infected individuals in Guinea-Bissau, West Africa: significantly lower plasma virus set point in HIV-2 infection than in HIV-1 infection. Archives of Internal Medicine. 2000;160:3286–3293. doi: 10.1001/archinte.160.21.3286. [DOI] [PubMed] [Google Scholar]
- 11.Berry N et al. Low level viremia and high CD4% predict normal survival in a cohort of HIV type-2-infected villagers. AIDS Research and Human Retroviruses. 2002;18:1167–1173. doi: 10.1089/08892220260387904. [DOI] [PubMed] [Google Scholar]
- 12.Popper SJ et al. Lower human immunodeficiency virus (HIV) type 2 viral load reflects the difference in pathogenicity of HIV-1 and HIV-2. Journal of Infectious Diseases. 1999;180:1116–1121. doi: 10.1086/315010. [DOI] [PubMed] [Google Scholar]
- 13.Gilbert PB et al. Comparison of HIV-1 and HIV-2 infectivity from a prospective cohort study in Senegal. Statistics in Medicine. 2003;22:573–593. doi: 10.1002/sim.1342. [DOI] [PubMed] [Google Scholar]
- 14.Kanki PJ et al. Slower heterosexual spread of HIV-2 than HIV-1. Lancet. 1994;343:943–946. doi: 10.1016/s0140-6736(94)90065-5. [DOI] [PubMed] [Google Scholar]
- 15.Norrgren H et al. Clinical progression in early and late stages of disease in a cohort of individuals infected with human immunodeficiency virus-2 in Guinea-Bissau. Scandinavian Journal of Infectious Diseases. 2003;35:265–272. doi: 10.1080/00365540310000210. [DOI] [PubMed] [Google Scholar]
- 16.Pepin J et al. HIV-2 infection among prostitutes working in The Gambia: association with serological evidence of genital ulcer diseases and with generalized lymphadenopathy. AIDS. 1991;5:69–75. [PubMed] [Google Scholar]
- 17.Poulsen AG et al. 9-year HIV-2-associated mortality in an urban community in Bissau, west Africa. Lancet. 1997;349:911–914. doi: 10.1016/S0140-6736(96)04402-9. [DOI] [PubMed] [Google Scholar]
- 18.Romieu I et al. HIV-2 link to AIDS in West Africa. Journal of Acquired Immune Deficiency Syndromes. 1990;3:220–230. [PubMed] [Google Scholar]
- 19.Whittle H et al. HIV-2-infected patients survive longer than HIV-1-infected patients. AIDS. 1994;8:1617–1620. doi: 10.1097/00002030-199411000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Poulsen AG et al. Risk factors for HIV-2 seropositivity among older people in Guinea-Bissau. A search for the early history of HIV-2 infection. Scandinavian Journal of Infectious Diseases. 2000;32:169–175. doi: 10.1080/003655400750045286. [DOI] [PubMed] [Google Scholar]
- 21.Korenromp EL et al. Model-based evaluation of single-round mass treatment of sexually transmitted diseases for HIV control in a rural African population. AIDS. 2000;14:573–593. doi: 10.1097/00002030-200003310-00013. [DOI] [PubMed] [Google Scholar]
- 22.Korenromp EL et al. HIV spread and partnership reduction for different patterns of sexual behaviour – a study with the microsimulation model STDSIM. Mathematical Population Studies. 2000;8:135–173. [Google Scholar]
- 23.White RG et al. Can population differences explain the contrasting results of the Mwanza, Rakai, and Masaka HIV/sexually transmitted disease intervention trials?: a modeling study. Journal of Acquired Immune Deficiency Syndromes. 2004;37:1500–1513. doi: 10.1097/01.qai.0000127062.94627.31. [DOI] [PubMed] [Google Scholar]
- 24.Orroth KKet al. Understanding differences across the contrasting epidemics in East and West Africa: results from a simulation model of the Four Cities Study. Sexually Transmitted Infections Published online: 3 April 2007. doi: 10.1136/sti.2006.023531
- 25.Donnelly C et al. Comparison of transmission rates of HIV-1 and HIV-2 in a cohort of prostitutes in Senegal. Bulletin of Mathematical Biology. 1993;55:731–743. doi: 10.1007/BF02460671. [DOI] [PubMed] [Google Scholar]
- 26.Greenberg AE. Possible protective effect of HIV-2 against incident HIV-1 infection: review of available epidemiological and in vitro data. AIDS. 2001;15:2319–2321. doi: 10.1097/00002030-200111230-00015. [DOI] [PubMed] [Google Scholar]
- 27.Schim van der Loeff M et al. HIV-2 does not protect against HIV-1 infection in a rural community in Guinea-Bissau. AIDS. 2001;15:2303–2310. doi: 10.1097/00002030-200111230-00012. [DOI] [PubMed] [Google Scholar]
- 28.Wiktor SZ et al. Lack of protection against HIV-1 infection among women with HIV-2 infection. AIDS. 1999;13:695–699. doi: 10.1097/00002030-199904160-00010. [DOI] [PubMed] [Google Scholar]
- 29.Kanki PJ. Clinical significance of HIV-2 infection in West Africa. AIDS Clinical Review. 1989:95–108. , pp. [PubMed] [Google Scholar]
- 30.Marlink R et al. Reduced rate of disease development after HIV-2 infection as compared to HIV-1. Science. 1994;265:1587–1590. doi: 10.1126/science.7915856. [DOI] [PubMed] [Google Scholar]
- 31.Anderson RM, May RM. The population biology of the interaction between HIV-1 and HIV-2: coexistence or competitive exclusion? AIDS. 1996;10:1663–1673. doi: 10.1097/00002030-199612000-00011. [DOI] [PubMed] [Google Scholar]
- 32.Ricard D et al. The effects of HIV-2 infection in a rural area of Guinea-Bissau. AIDS. 1994;8:977–982. doi: 10.1097/00002030-199407000-00016. [DOI] [PubMed] [Google Scholar]
- 33.Matheron S et al. HIV-1 and HIV-2 AIDS in African patients living in Paris. AIDS. 1997;11:934–936. [PubMed] [Google Scholar]
- 34.Kawamura M et al. HIV-2 in West Africa in 1966. Lancet. 1989;1:385. doi: 10.1016/s0140-6736(89)91760-1. [DOI] [PubMed] [Google Scholar]
- 35.Lemey P et al. Tracing the origin and history of the HIV-2 epidemic. Proceedings of the National Academy of Sciences USA. 2003;100:6588–6592. doi: 10.1073/pnas.0936469100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fultz PN et al. Seroprevalence of HIV-1 and HIV-2 in Guinea Bissau in 1980. AIDS. 1988;2:129–132. doi: 10.1097/00002030-198804000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Lagarde E et al. Mobility and the spread of human immunodeficiency virus into rural areas of West Africa. International Journal of Epidemiology. 2003;32:744–752. doi: 10.1093/ije/dyg111. [DOI] [PubMed] [Google Scholar]
- 38.WHO Guinea-Bissau: 2003. . Core Health Indicators by Country: [Google Scholar]
- 39.Buve A et al. Interpreting sexual behaviour data: validity issues in the multicentre study on factors determining the differential spread of HIV in four African cities. AIDS. 2001;15:S117–S126. doi: 10.1097/00002030-200108004-00013. (Suppl. 4): [DOI] [PubMed] [Google Scholar]
- 40.Nnko S et al. Secretive females or swaggering males? An assessment of the quality of sexual partnership reporting in rural Tanzania. Social Science & Medicine. 2004;59:299–310. doi: 10.1016/j.socscimed.2003.10.031. [DOI] [PubMed] [Google Scholar]
- 41.Matos Almeida MJ 1989. HIV-1 and HIV-2 serological survey in Lunda Norte, northeastern province of Republica Popular de Angola, . The scientific and social challenge. V International Conference on AIDS, Montreal.
- 42.UNAIDS/WHO. Guinea-Bissau: 2006. ). UNAIDS/WHO Epidemiological Fact Sheet, 2006 Update, [Google Scholar]
- 43.UNAIDS/WHO. Geneva: UNAIDS/WHO; 2006. ). Report on the global AIDS epidemic. . Annex 2. [Google Scholar]
- 44.Buckner M, Becker C, Dozon JP, Toure M.Village women as town prostitutes: cultural factors relevant to prostitution and HIV epidemiology in Guinea-Bissau Experiencing and Understanding AIDS in AfricaParis: Editions Karthala; 1999, pp. 391–404. [Google Scholar]
- 45.Aaby P et al. Age of wife as a major determinant of male-to-female transmission of HIV-2 infection: a community study from rural West Africa. AIDS. 1996;10:1585–1590. doi: 10.1097/00002030-199611000-00019. [DOI] [PubMed] [Google Scholar]
- 46.Holmgren B et al. Increased prevalence of retrovirus infections among older women in Africa. Scandinavian Journal of Infectious Diseases. 1999;31:459–466. doi: 10.1080/00365549950163978. [DOI] [PubMed] [Google Scholar]
- 47.Pepin J et al. Parenteral transmission during excision and treatment of tuberculosis and trypanosomiasis may be responsible for the HIV-2 epidemic in Guinea-Bissau. AIDS. 2006;20:1303–1311. doi: 10.1097/01.aids.0000232239.05545.33. [DOI] [PubMed] [Google Scholar]
- 48.Koblavi-Deme S et al. Differences in HIV-2 plasma viral load and immune activation in HIV-1 and HIV-2 dually infected persons and those infected with HIV-2 only in Abidjan, Cote D'Ivoire. AIDS. 2004;18:413–419. doi: 10.1097/00002030-200402200-00006. [DOI] [PubMed] [Google Scholar]
- 49.Sarr AD et al. Relation between HIV-2 proviral load and CD4+ lymphocyte count differs in monotypic and dual HIV infections. Journal of Human Virology. 1999;2:45–51. [PubMed] [Google Scholar]
- 50.Morgan D et al. HIV-1 infection in rural Africa: is there a difference in median time to AIDS and survival compared with that in industrialized countries? AIDS. 2002;16:597–603. doi: 10.1097/00002030-200203080-00011. [DOI] [PubMed] [Google Scholar]