Abstract
Objectives
To determine whether bodily pain is increased in patients with chronic rhinosinusitis (CRS) and if bodily pain improves following endoscopic sinus surgery (ESS).
Methods
All studies reporting results of more than 10 adult patients analyzing the response of bodily pain to ESS were retrieved by searching MEDLINE, EMBASE, Web of Science, Cochrane databases, and additional Web-based sources (from January 1, 1980, to May 1, 2008); by examining bibliographies of retrieved articles; and by contacting investigators in the field.
Results
Of 279 ESS symptom outcome studies, only studies measuring results using the 36-Item Short Form Health Survey (SF-36) quality-of-life survey instrument measured bodily pain. Eleven observational ESS studies (1019 patients) reported mean preoperative SF-36 bodily pain scores at 0.89 SD below general population norms (24% more severe bodily pain than general population norms) and significantly below norms for a population 25 years older. Using a repeated-measures design, 9 of 11 studies noted significant improvement in SF-36 bodily pain domain scores following ESS, with a moderate-sized combined effect of 0.55 (95% confidence interval, 0.45–0.64; I2 = 44%) using the fixed-effects model. This pooled effect corresponded to a mean improvement of 11.8 U on the SF-36 bodily pain domain scale.
Conclusions
Bodily pain is increased in patients with CRS awaiting ESS, exceeding the normative bodily pain scores of a general normative population 25 years older. Using within-subject comparisons, a clinically and statistically significant improvement in bodily pain is noted after ESS, an improvement similar to that previously described for fatigue.
Keywords: Bodily pain, chronic rhinosinusitis, surgery, endoscopic, fibromyalgia, SF-36, fatigue, quality of life, meta-analysis
Introduction
More than 15 years ago, Cleveland et al1 reported a preponderance of generalized bodily pain in patients with rhinitis. Conversely, a disproportionately high prevalence of chronic rhinosinusitis (CRS) symptoms among patients with otherwise unexplained bodily pain was noted in a study2 of patients seeking general medical care. Confirmation of both observations has been evidenced by studies3,4 of patients with CRS using the 36-Item Short Form Health Survey (SF-36), a general health-related quality-of-life (QOL) instrument that includes a separate assessment of bodily pain.
Within one of the more commonly used global QOL survey instruments to measure changes following endoscopic sinus surgery (ESS), the bodily pain domain score of the SF-36 measures the frequency of and discomfort due to bodily pain on a scale of 0 (most bodily pain) to 100 (least bodily pain), permitting comparisons with general population norms. Geographically, culturally, and racially/ethnically diverse populations of patients with CRS show increased SF-36 bodily pain scores compared with norms.3–6
Fibromyalgia and other illnesses (eg, chronic fatigue syndrome, multiple chemical sensitivity syndrome, and sick building syndrome) commonly characterized by fatigue, bodily pain, and the absence of objective findings are commonly associated with an increased prevalence of CRS.7,8 One study demonstrated that 25% of patients with fibromyalgia had visited a physician within the previous 6 months for CRS-related problems.9
Among many diverse medical specialties, clinicians have not generally accepted CRS as an independent and sufficient cause of bodily pain. This may prompt clinicians to look for and ascribe bodily pain symptoms to another condition aside from CRS, such as fibromyalgia. The possibility that some patients diagnosed with both fibromyalgia (or other functional somatic syndromes) and CRS are actually experiencing only CRS may not be considered.
Systematic assessments of the severity of bodily pain from CRS prior to ESS and the response of bodily pain to ESS have not been performed, to our knowledge. The objectives of this study were to determine if elevated levels of bodily pain are associated with CRS and to examine whether bodily pain improves following ESS.
Materials and Methods
Identification of Studies
We searched PubMed, MEDLINE, EMBASE, Cochrane databases, Web of Science, and Google Scholar for all English-language peer-reviewed ESS studies of more than 10 adults from January 1, 1980, or database inception, to May 1, 2008. We used the following “exploded” Medical Subject Headings and text words: endoscopic, sinus, and surgery. Relevant reviews and cited references from retrieved articles were examined for additional studies. Issues of the American Journal of Rhinology not listed in Index Medicus (1987–1997) were searched by hand. After reviewing all titles and relevant abstracts for the reporting of ESS symptom outcomes, full-text articles were obtained for appropriate studies. We excluded studies involving surgery limited to the turbinates or septum, radical surgery (e.g., frontal sinus drillout or sinus ablation), surgery involving massive polyposis, and reports of results on patients with substantial comorbidities (e.g., cystic fibrosis, human immunodeficiency virus, and malignancy).
Relevant unpublished data were also sought. We examined ISI Proceedings (accessed through Web of Science), contacted authors for additional data when necessary, and consulted investigators in the field.
Studies of all designs reporting symptom response following ESS were examined for any measurements of bodily pain. In addition, all survey instruments measuring generic or disease-specific QOL following ESS were examined for any questions related to bodily pain.
Studies reporting results on bodily pain were limited to those utilizing the SF-36, the 12-Item Short Form Health Survey (SF-12), or the 8-Item Short Form Health Survey (SF-8). The SF-36 reports QOL scores in 8 domains from 0 (worst QOL) to 100 (best QOL) and measures bodily pain by scoring the response to 2 multiple-choice questions that, when combined, produce 11 possible levels of bodily pain severity. The SF-12 and the SF-8 are abbreviated versions of the SF-36. Using the already described methods, we searched for non–English-language studies with results measured by the SF-36, SF-12, or SF-8. After an independent search and assessment by 2 of us (A.C.C. and R.S.) and a group consultation, articles were cataloged.
Study Selection and Data Extraction
Using the guidelines provided by MOOSE (Meta-analysis of Observational Studies in Epidemiology),10 2 of the authors (A.C.C. and R.S.) independently reviewed all included studies measuring bodily pain before and after ESS. Using the PICOS (participant, intervention and exposure, comparator, outcomes, and study design) approach, the following characteristics of the studies and the participants were recorded: author, year, design, participants, surgical procedure, duration, purpose, survey methods, and specific symptoms analyzed. The time from surgery to the last evaluation of bodily pain was defined as the study duration. Study characteristics were entered into a spreadsheet (Excel 2003; Microsoft Corporation, Redmond, Washington). Meta-analysis was performed using commercially available software (Comprehensive Meta-Analysis software version 2.2; Biostat, Inc, Englewood, New Jersey).
Statistical Analysis
The standardized mean difference (Cohen d) of the SF-36 bodily pain domain scores before and after surgery using the exact sample size before and after surgery was defined as the effect size for outcome measures. Effect size in this study refers to the amount of improvement in bodily pain after ESS. Effect size is a standardized form of measuring the effect of an intervention adjusting for the pooled standard deviations of the outcomes measures.
Because the correlation coefficient (r) between the paired measures before and after surgery (a statistic not generally published) is required for an optimal estimated effect size, we calculated the repeated standardized mean difference using appropriate formulas11 provided by Comprehensive Meta-Analysis software version 2.2. The latter results are similar to Cohen d, especially for studies with the same sample size before and after surgery.
Bodily pain results were limited to studies reporting results using the SF-36 and SF-8. Therefore, this meta-analysis is limited to studies using these validated instruments. The combined effects for summarizing odds ratios and standardized mean differences were calculated using both the fixed method and the random-effects method. The SF-36 mean bodily pain domain scores were compared with normative values using 1-sample t test. For all results, P < .05 was considered statistically significant.
The SF-36 bodily pain scores were reported in 9 studies6,12–19 and were provided by the authors in 2 additional studies20,21 (G. E. Davis, MD, MPH, e-mail communication, May 2008; and V. J. Lund, MS, FRCS, FRCS (Edin), written correspondence, December 2004). The SF-8 bodily pain domain scores were reported in a study13 that was considered an SF-36 study. Three studies12,17,21 among the 11 reported means but not standard deviations; when standard deviations were not specified and were unobtainable from the authors, they were estimated based on the other 8 SF-36 bodily pain domain standard deviation scores (23.7 U before surgery and 21.9 U after surgery). When studies reported only the results of separate groups (e.g., men and women), scores were weighted according to sample size and aggregated.
To evaluate whether the effects of ESS on bodily pain were the same across studies, heterogeneity was assessed. Heterogeneity was assessed using I2, a statistic that describes the percentage of total variation across trials due to heterogeneity rather than chance, where I2 lies between 0% (no heterogeneity) and 100% (maximal heterogeneity), with 25%, 50%, and 75% representing low, moderate, and high heterogeneity, respectively.22 I2 is calculated as I2 = 100% × (Q − df)/Q, where Q indicates the Cochran heterogeneity statistic.
Results
Literature Search
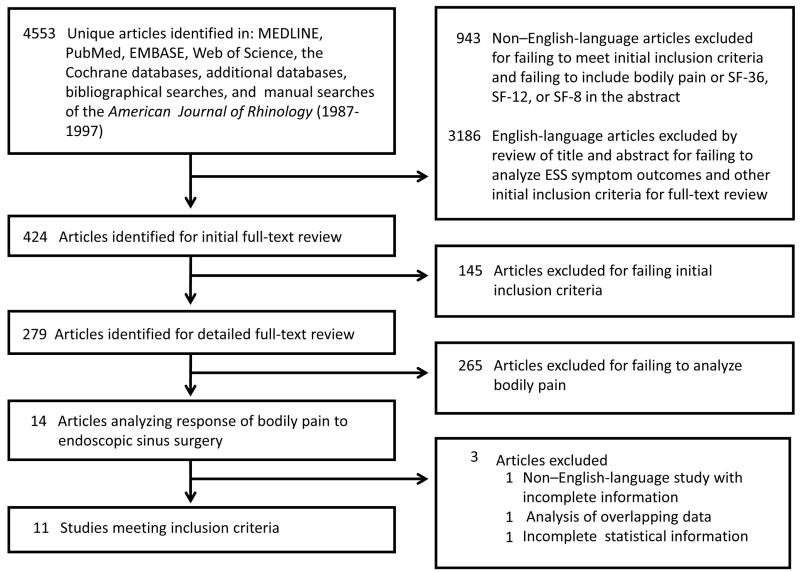
After a review of 4553 articles identified by the prescribed searches and a full-text review of 424 articles we found 279 studies that met initial selection criteria (Fig 1). All survey instruments and other symptom scoring methods were examined for questions concerning bodily pain. Of 18 different survey instruments used in 279 articles bodily pain was measured in 4 surveys: Glasgow Benefit Inventory (2 studies); European Quality of Life (1 study), SF-36 (13 studies), and SF-8 (1 study). Independent scores for questions concerning bodily pain were not available for studies measuring results using the Glasgow Benefit Inventory or the European Quality of Life. No additional studies measured bodily pain by any other method.
Figure 1.
Study selection. SF-8 = 8-Item Short Form Health Survey; SF-12 = 12-Item Short Form Health Survey SF-36 = 36-Item Short Form Health Survey
Measures of bodily pain before and after ESS applicable to this meta-analysis were limited to 11 studies using the SF-36 (10 studies) or SF-8 surveys (1 study) (Table). One non–English-language study6 was translated by Dr. Rusan Chen, Senior Statistician, Georgetown University. The other non–English-language study17 was translated by Steven Vitek, Technical Translator, PatentTranslators.com. (Copies of both translations are available from the corresponding author.)
Table.
Characteristics of Included Studies
| Sourcea | Study Design | Length of Follow- up, mo | Sample Sizeb | Age, mean, y | Outcome Measure |
|---|---|---|---|---|---|
| Baumann and Blumenstock,12 2005 (Germany) | CS (prospective), consecutive patients | 3 | 121 | 47.9 | BP (SF-36) |
| Brandsted and Sindwani,13 2007 (USA) | Record review (retrospective), consecutive patients | 12 | 40 | 45 | BP (SF-8)c |
| Davis et al,20 2005 (USA) | CS (prospective), consecutive patients | 12 | 51 | 45.9 | BP (SF-36) |
| Durr and Desrosiers,14 2003 (Canada) | CS (prospective), consecutive patients | 3 | 47 | 43.7 | BP (SF-36) |
| Gliklich and Hilinski,15 1995 (USA) | CS (prospective), consecutive patients | 3 | 40 | 42.6 | BP (SF-36) |
| Gliklich and Metson,16 1997 (USA) | CT (prospective), consecutive patients | 6 | 108 | 42.7 | BP (SF-36) |
| Hosemann et al,17 2003 (Germany) | CS (prospective), consecutive patients | 6 | 103 | 44 | BP (SF-36) |
| Khalid et al,18 2004 (USA) | Retrospective, randomly selected patients | 36 | 150 | 46.9 | BP (SF-36) |
| Ragab et al,21 2004 (United Kingdom) | RCT (prospective), consecutive patients | 12 | 40 | 43 | BP (SF-36) |
| Winstead and Barnett,19 1998 (USA) | CS (prospective), consecutive patients | 12 | 43 | 34 | BP (SF-36) |
| Zuo et al,6 2007 (China) | CS (prospective), randomly selected patients | 6 | 115 | 33.5 | BP (SF-36) |
Abbreviations: BP, bodily pain; CS, cohort study; CT, clinical trial; RCT, randomized controlled trial; SF-8, 8-Item Short Form Health Survey; SF-36, 36-Item Short Form Health Survey.
Additional information was obtained about the following studies: Baumann and Blumenstock12 (from I. Baumann, MD, e-mail communication, May 2007); Davis et al20 (from G. E. Davis, MD, MPH, e-mail communication, May, 2008); Hosemann et al17 (from W. Hosemann, MD, e-mail communication, June 2007); and Ragab et al21 (from V. J. Lund, MS, FRCS, FRCS(Edin), written correspondence, December 2004).
Number of patients with final outcome data.
For the purposes of this study, results from the SF-8 are considered with those from the SF-36.
Two studies23,24 reported SF-12 results using a version that did not include bodily pain domain scores (M. Akarcay, MD, e-mail communication, January 2005; and S. J. Atlas, MD, e-mail communication, March 2007). Two studies reported results from an identical or overlapping database and were excluded.25,26 A study27 reporting SF-36 results as medians rather than means were also excluded.
Study and Baseline Patient Characteristics
Although the purpose and design of the included studies varied, all measured bodily pain before and after ESS using within-subject comparisons. Study design, length of follow-up, sample size, and the mean age of the patients for each of the 11 studies are given in the table.
The total sample size for the meta-analysis was 1019 patients (range, 39–150 patients per study), with a mean (SD) age of 42.6 (4.7) years during a mean (SD) follow-up of 10.1 (9.4) months (median, 6 months). Nine of 11 were prospective cohort studies. The mean and median percentage of women in each study was 50% (range, 28%17–67%14).
The percentage of patients with nasal polyposis presenting for surgery was noted in 7 studies and ranged from 7%19 to 55%6 (median, 40%). A history of nasal surgery was stated as an exclusionary condition in 3 studies.14–16 The percentages of patients presenting for surgery with a history of prior nasal surgery was noted in 3 studies (17%,19 24%,12 and 81%18). Patients with serious comorbid diseases were specifically excluded from 3 studies,14,19,21 and none of the other studies described patients with significant comorbid diseases. The surgical procedure in all studies was described as ESS but varied in extent depending on CT and endoscopic findings.
Quantitative Data Synthesis
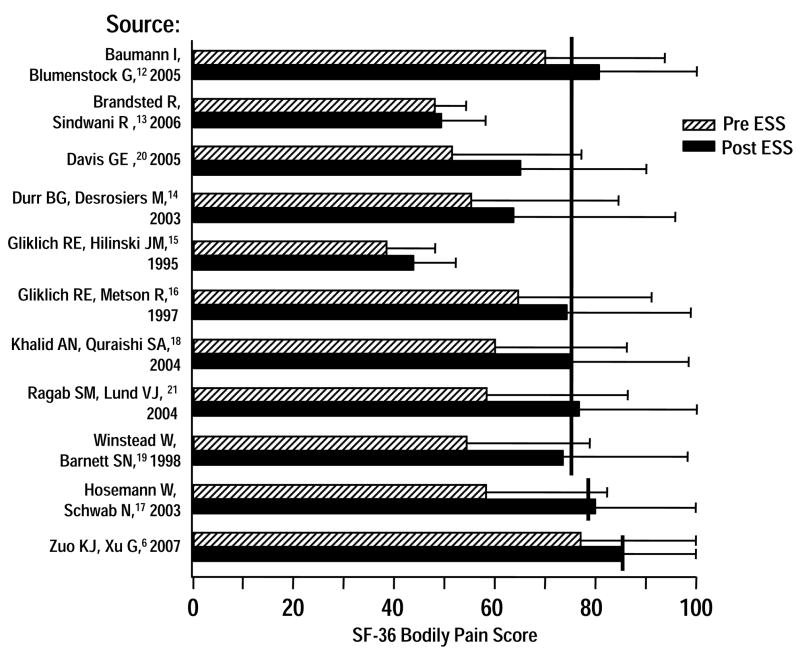
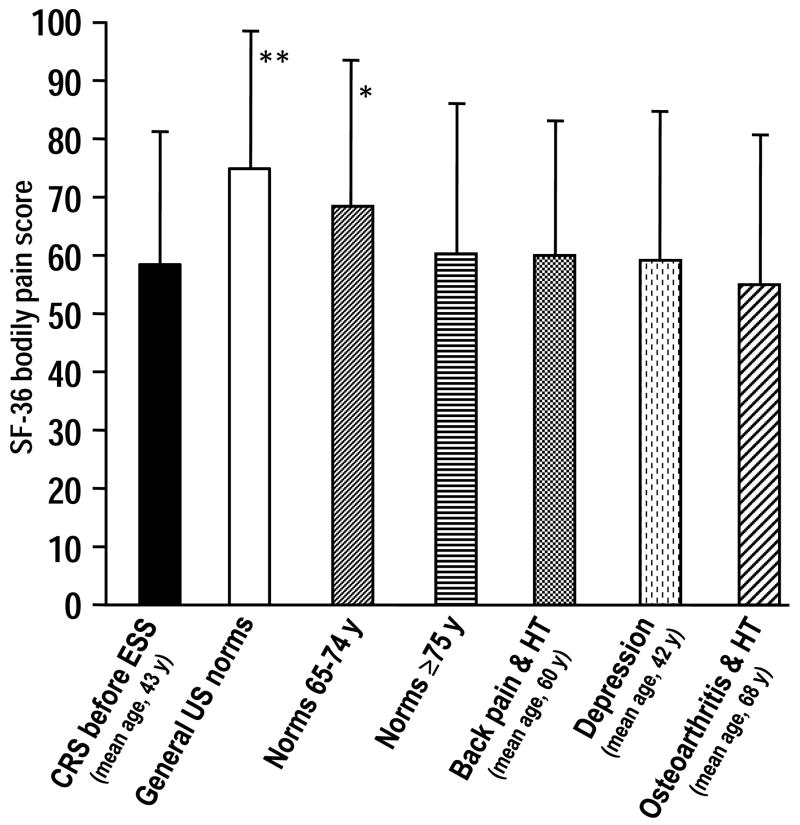
The pooled mean preoperative SF-36 bodily pain domain score of the 11 included studies, weighted by sample size, was 0.89 SD below US national or local population norms (P<.001) indicating a 24% greater burden of bodily pain when compared to these norms (Fig 2). Bodily pain scores were also significantly less (indicating more bodily pain) than those of a general normative population 25 years older and were similar to those of a general normative population 75 years or older (Fig 3).
Figure 2.
Preoperative and postoperative SF-36 bodily pain symptom scores. Vertical bars indicate national or local general population SF-36 bodily pain normative values. Brackets indicate SDs.
Figure 3.
Comparisons between preoperative SF-36 bodily pain scores in studies12–16, 18–21 using US SF-36 bodily pain score norms and normative values for different age groups and different diseases. Brackets indicate SDs. Abreviation: HT indicates hypertension; CRS pre-ESS indicates values for patients with chronic rhinosinusitis before endoscopic sinus surgery.
*Chronic rhinosinusitis patients before endoscopic sinus surgery vs. general US normative values (P<.001).
** Chronic rhinosinusitis patients before endoscopic sinus surgery vs. US normative values for people 65 to 74 years of age (P<.001).
Among 11 studies, 2 studies13,14 did not demonstrate a significant improvement in bodily pain domain scores following ESS. The remaining 9 studies showed a statistically significant improvement in the postoperative bodily pain domain scores compared with preoperative levels.
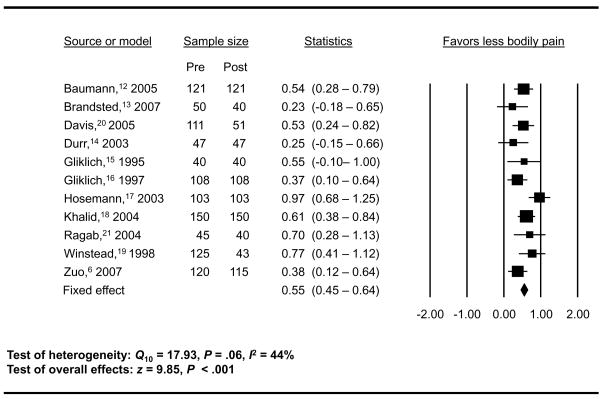
Figure 4 shows the results of the meta-analysis using a forest plot of effect size and 95% confidence interval for each study. The effect size ranged from 0.23 to 0.97. The combined effect sizes, defined as Cohen d, are 0.55 and 0.54 as estimated using the fixed model and the random-effects model, respectively, showing a moderate effect size as defined by Cohen.28 A fixed-effects model assumes that ESS had similar effects across studies, while a random-effects model assumes that ESS may have different treatment effects across studies. The test of heterogeneity resulted in Q10 = 17.93 (P = .06) with I2 = 44%, demonstrating moderate heterogeneity.
Figure 4.
Changes in SF-36 bodily pain scores following endoscopic sinus surgery.
Abbreviation: SF-36, 36-Item Short Form Health Survey. Data are given as standardized mean difference (95% confidence interval) unless otherwise indicated. Positive estimates favor decreased bodily pain following endoscopic sinus surgery. Effect size was defined as the standardized mean difference (Cohen d). See “Methods” section for further details. Cochran Q test was used to measure heterogeneity.
Following surgery, postoperative bodily pain scores improved to values similar to US national or local population norms in 7 studies.6,12,16–19,21 The mean postoperative SF-36 bodily pain domain score for all studies was approximately 0.30 SD below US or local population norms indicating 9% more bodily pain in the post surgical study group than in the normative populations.
Discussion
Although often unrecognized, the burden of CRS-associated bodily pain is substantial, exceeding the burden of bodily pain in a patient population norm 25 years older and similar to that of older patients, patients with depression, and patients having arthritis. The resulting QOL impairment due to bodily pain is well described by the SF-36, however, the prevalence of bodily pain is not. Cleveland et al1 noted bodily pain among 49% in a series of 47 consecutive patients with rhinitis. Fibromyalgia diagnostic criteria were met in 38% of the study population. In a study7 of patients with chronic fatigue syndrome, a syndrome defined, in part, by bodily pain and symptoms typical of CRS, 71% had symptoms of rhinitis.
Fatigue and bodily pain largely define a number of functional somatic syndromes that are poorly differentiated from each other, lack objective findings, and are characterized by a disproportionate prevalence of CRS (chronic fatigue syndrome, fibromyalgia, multiple chemical sensitivity syndrome, etc.) Because undetected or undiagnosed CRS has not been a generally accepted explanation for otherwise unexplained bodily pain it is likely that some patients are inappropriately classified as experiencing these functional somatic syndromes. These syndromes are associated with significant morbidity and respond poorly to treatment. The need to appropriately diagnose and treat CRS in patients with functional somatic syndromes is supported by our findings and by a recent report29 demonstrating improvement in fatigue and QOL following ESS in patients with fibromyalgia.
The improvement in bodily pain noted in 9 of 11 studies produced a moderate-sized combined effect of 0.55 (95% confidence interval, 0.45–0.64), corresponding to a mean (SD) improvement of 11.8 (6.1) U on the SF-36 bodily pain domain scale. This improvement reflects a change in the responses to 2 multiple-choice bodily pain domain questions of approximately 1 level (1 net state change) among 11 possible levels of response. A combined effect of 0.5 SD such as that noted herein usually corresponds to a minimal clinically important difference in diseases for which a minimal clinically important difference has been established.30 The effect size of ESS in relieving bodily pain is similar to the effect size of some established therapies in relieving the bodily pain of fibromyalgia (aerobic exercise effect size, 0.377; pool-based exercise effect size, 0.437; and tramadol hydrochloride effect size, 0.657).31
In addition, the combined effect improvement noted for bodily pain is similar to the SF-36 vitality domain score combined effect of 0.47 (95% confidence interval, 0.38–0.56) as noted in a previous publication.32 In that study, fatigue (vitality) improved after ESS to a similar degree as other pooled nasal symptoms, suggesting that bodily pain might also improve as much as other pooled nasal symptoms after surgery.
While bodily pain has been only minimally explored as a specific CRS symptom complex, 1 study33 noted more bodily pain in patients with greater than 9 mm of sinus soft tissue swelling on computed tomography than in patients with 9 mm or less of swelling. While the conclusions of this meta-analysis are partially limited by the number, size, and design of the studies examined they do, nevertheless, offer the most consistent evidence to date that bodily pain likely improves following ESS. Patients awaiting ESS for CRS who have significant bodily pain symptoms can expect with a reasonable likelihood that their symptoms will show fairly substantial improvement after surgery.
Conclusions
Chronic rhinosinusitis is characterized by elevated levels of bodily pain in addition to more well-known symptoms. Following ESS, bodily pain improves by a pooled effect size of approximately 0.5 SD, a statistically significant improvement similar to that noted in a previous meta-analysis32 for fatigue.
Acknowledgments
We thank Rusan Chen, PhD, Senior Statistician, Georgetown University, Washington, DC, for his invaluable help with statistical analysis and Catherine A. Alden for editorial assistance. We thank the following authors for providing additional information about their studies: M. Akarcay, MD; S. J. Atlas, MD; I. Baumann, MD; G. E. Davis, MD, MPH; D. G. Durr, MD; W. Hosemann, MD, and V. J. Lund, MS, FRCS, FRCS (Edin).
Footnotes
Presented at the Annual Meeting of the American Academy of Otolaryngology–Head and Neck Surgery, Chicago, Illinois, September 22, 2008.
Financial Disclosure: None reported.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Alexander C. Chester, Department of Medicine, Georgetown University Hospital, Washington, DC.
Raj Sindwani, Department of Otolaryngology–Head and Neck Surgery, St Louis University School of Medicine, St Louis, Missouri.
Timothy L. Smith, Department of Otolaryngology–Head and Neck Surgery, Oregon Health & Science University, Portland.
Neil Bhattacharyya, Division of Otolaryngology, Brigham and Women’s Hospital, and Department of Otology & Laryngology, Harvard Medical School, Boston, Massachusetts.
References
- 1.Cleveland CH, Jr, Fisher RH, Brestel EP, et al. Chronic rhinitis: an underrecognized association with fibromyalgia. Allergy Proc. 1992;13:263–267. doi: 10.2500/108854192778817077. [DOI] [PubMed] [Google Scholar]
- 2.Chester AC. Symptoms of rhinosinusitis in patients with unexplained chronic fatigue or bodily pain: a pilot study. Arch Intern Med. 2003;163:1832–1867. doi: 10.1001/archinte.163.15.1832. [DOI] [PubMed] [Google Scholar]
- 3.Gliklich RE, Metson R. Effect of sinus surgery on quality of life. Otolaryngol Head Neck Surg. 1997;117:12–17. doi: 10.1016/S0194-59989770199-2. [DOI] [PubMed] [Google Scholar]
- 4.Durr DG, Desrosiers MY, Dassa C. Impact of rhinosinusitis in health care delivery: the Quebec experience. J Otolaryngol. 2001;30:93–97. doi: 10.2310/7070.2001.20813. [DOI] [PubMed] [Google Scholar]
- 5.Wang PC, Tai CJ, Lin MS, et al. Quality of life in Taiwanese adults with chronic rhino-sinusitis. Qual Life Res. 2003;12:443–448. doi: 10.1023/a:1023494025748. [DOI] [PubMed] [Google Scholar]
- 6.Zuo KJ, Xu G, Wang DY, et al. Postoperative symptoms and life quality assessment of chronic rhinosinusitis patients receiving endoscopic sinus surgery [in Chinese] Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2007;42:245–249. [PubMed] [Google Scholar]
- 7.Baraniuk JN, Clauw DJ, Gaumond E. Rhinitis symptoms in chronic fatigue syndrome. Ann Allergy Asthma Immunol. 1998;81:359–365. doi: 10.1016/S1081-1206(10)63129-8. [DOI] [PubMed] [Google Scholar]
- 8.Waylonis GW, Heck W. Fibromyalgia syndrome. New associations. Am J Phys Med Rehabil. 1992;71:343–8. doi: 10.1097/00002060-199212000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Michaud K, Wolfe F. The association of rheumatoid arthritis and its treatment with sinus disease. J Rheumatol. 2006;33:2412–241. [PubMed] [Google Scholar]
- 10.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 11.Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychol Meth. 1996;1(2):170–177. [Google Scholar]
- 12.Baumann I, Blumenstock G. Impact of gender on general health-related quality of life in patients with chronic sinusitis. Am J Rhinol. 2005;19:282–287. [PubMed] [Google Scholar]
- 13.Brandsted R, Sindwani R. Impact of depression on disease-specific symptoms and quality of life in patients with chronic rhinosinusitis. Am J Rhinol. 2007;21:50–54. doi: 10.2500/ajr.2007.21.2987. [DOI] [PubMed] [Google Scholar]
- 14.Durr DG, Desrosiers M. Evidence-based endoscopic sinus surgery. J Otolaryngol. 2003;32:101–106. doi: 10.2310/7070.2003.37123. [DOI] [PubMed] [Google Scholar]
- 15.Gliklich RE, Hilinski JM. Longitudinal sensitivity of generic and specific health measures in chronic sinusitis. Qual Life Res. 1995;4:27–32. doi: 10.1007/BF00434380. [DOI] [PubMed] [Google Scholar]
- 16.Gliklich RE, Metson R. Effect of sinus surgery on quality of life. Otolaryngol Head Neck Surg. 1997;117:12–17. doi: 10.1016/S0194-59989770199-2. [DOI] [PubMed] [Google Scholar]
- 17.Hosemann W, Schwab N, Praetner L, et al. Extended outcome assessment in endonasal sinus surgery [in German] Laryngorhinootologie. 2003;82:341–346. doi: 10.1055/s-2003-39729. [DOI] [PubMed] [Google Scholar]
- 18.Khalid AN, Quraishi SA, Kennedy DW. Long-term quality of life measures after functional endoscopic sinus surgery. Am J Rhinol. 2004;18:131–136. [PubMed] [Google Scholar]
- 19.Winstead W, Barnett SN. Impact of endoscopic sinus surgery on global health perception: an outcomes study. Otolaryngol Head Neck Surg. 1998;119:486–491. doi: 10.1016/S0194-5998(98)70106-8. [DOI] [PubMed] [Google Scholar]
- 20.Davis GE, Yueh B, Walker E, et al. Psychiatric distress amplifies symptoms after surgery for chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2005;132:189–196. doi: 10.1016/j.otohns.2004.09.135. [DOI] [PubMed] [Google Scholar]
- 21.Ragab SM, Lund VJ, Scadding G. Evaluation of the medical and surgical treatment of chronic rhinosinusitis: a prospective, randomised, controlled trial. Laryngoscope. 2004;114:923–930. doi: 10.1097/00005537-200405000-00027. [DOI] [PubMed] [Google Scholar]
- 22.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 23.Akarcay M, Kizilay A, Miman MC, et al. The effect of endoscopic sinus surgery on quality of life [in Turkish] Kulak Burun Bogaz Ihtis Derg. 2003;11:65–71. [PubMed] [Google Scholar]
- 24.Atlas SJ, Metson RB, Singer DE, et al. Validity of a new health-related quality of life instrument for patients with chronic sinusitis. Laryngoscope. 2005;115:846–854. doi: 10.1097/01.MLG.0000157693.92975.02. [DOI] [PubMed] [Google Scholar]
- 25.Baumann I, Blumenstock G, Praetorius M, et al. Patients with chronic rhinosinusitis: disease-specific and general health-related quality of life [in German] HNO. 2006;54:544–549. doi: 10.1007/s00106-006-1402-y. [DOI] [PubMed] [Google Scholar]
- 26.Zuo KJ, Xu G, Shi JB, et al. Subjective and objective clinical outcome assessment on chronic rhinosinusitis following endoscopic sinus surgery. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2008;43:7–12. [PubMed] [Google Scholar]
- 27.Hoffman SF, Mahoney MC, Chmiel JF, et al. Conducting outcomes research in a community-based practice setting. Am J Rhinol. 1994;8:193–200. [Google Scholar]
- 28.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 29.Soler Z, Mace J, Smith TL. Fibromyalgia and chronic rhinosinusitis: Outcomes after endoscopic sinus surgery. Am J Rhinol. 2008;22:427–432. doi: 10.2500/ajr.2008.22.3198. 2008; in press. [DOI] [PubMed] [Google Scholar]
- 30.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 31.Carville SF, Arendt-Nielsen S, Bliddal H, et al. EULAR evidence-based recommendations for the management of fibromyalgia syndrome. Ann Rheum Dis. 2008;67:536–541. doi: 10.1136/ard.2007.071522. [DOI] [PubMed] [Google Scholar]
- 32.Chester AC, Sindwani R, Smith TL, et al. Fatigue improvement following endoscopic sinus surgery: a systematic review and meta-analysis. Laryngoscope. 2008;118:730–739. doi: 10.1097/MLG.0b013e318161e57b. [DOI] [PubMed] [Google Scholar]
- 33.Stavem K, Rossberg E, Larsson PG. Reliability, validity and responsiveness of a Norwegian version of the Chronic Sinusitis Survey. BMC Ear Nose Throat Disord. 2006;6:e9. doi: 10.1186/1472-6815-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]