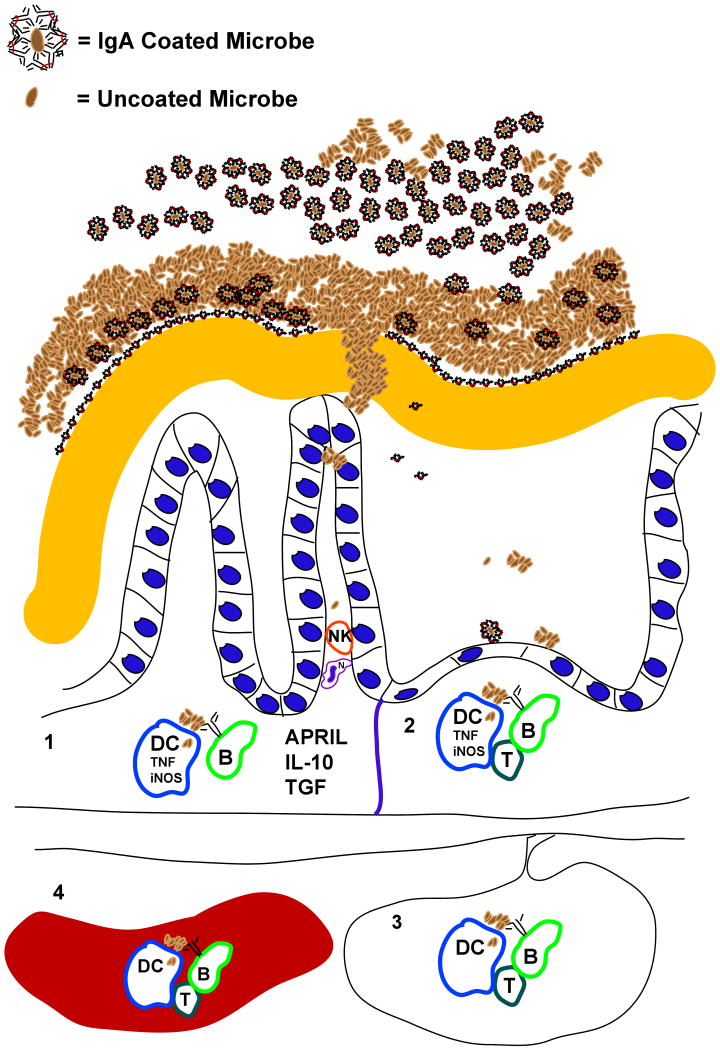
Figure 3. Host-microbial interactions affected by IgA are modulated as result of stimulation of the immune system at different sites.
Secretory IgA, antimicrobial peptides, and mucus are among the factors that comprise the mucosal barrier. The ability of different microorganisms to develop resistance to these factors, or to degrade mucus, will contribute to greater microbial pattern recognition receptor-mediated signaling in epithelial cells, dendritic cells (DCs), macrophages, and B cells. Where these organisms prime the adaptive immune system will depend on how far they can penetrate the barrier, and where the host traffics microbial cells and their antigens. Numbers in the figure refer to the following processes. (1) The simplest response loop may be the innate immune system's induction of IgA production in the lamina propria: NK, DC, epithelial cell-derived cytokines (APRIL, IL-10, TGF, TNF among others) and membrane-bound receptors (e.g. CD40-CD40 ligand) induce IgA production from recruited B cells. (2) Bacteria, bound or unbound by IgA in the lumen, are actively transported to Peyer's patches and associated lymphoid organs where T cell priming and help are more likely. (3) DCs transport whole bacteria and microbial antigens to mesenteric lymph nodes where priming of T cells and B cells programs them to home to the lamina propria, and where IgA induction is favored. (4) Commensal microbes (and invasive pathogens) are transported and trapped by the innate immune system in the spleen, where a systemic immune response is induced (lymphocytes primed in the spleen are less likely to home to the gut, and more likely to switch to non-IgA subclasses).