Abstract
Rationale
End of test criteria can influence spirometry results. Epidemiology studies initiated before adoption of the 1987 American Thoracic Society (ATS) guidelines typically used a 1 or 2 second plateau on the volume-time curve, not a minimum test duration of 6 seconds, to terminate a test.
Objectives
To determine the effect of changing guidelines on FEV1, FVC and FEV1/FVC during a longitudinal study of young adults.
Methods
Spirometry was performed on participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study. Values obtained at entry and 2, 5 and 10 years later using accepted procedures were re-evaluated using the 2005 ATS-ERS guidelines, which were in effect for the year 20 exam. Generalized estimating equations were used to adjust tests with short exhalations that were acceptable by then current end of test criteria.
Results
The percentage of participants at years 0, 2, 5, and 10 with exhalations less than six seconds but with an acceptable plateau was 33%, 29%, 9%, and 2%, respectively. Exhalations less than 6 seconds occurred more frequently in younger and female participants, and were associated with lower FVC and higher FEV1/FVC. For short exhalations the adjusted FVC was 47 ml and 110 ml higher than the measured FVC when 6 and 8 second exhalation times were used.
Conclusions
In longitudinal studies of young adults, changing end of test criteria may affect lung function, especially among younger and female participants. Determining adjusted values for tests with short exhalations may better represent the lung health of participants.
Keywords: CARDIA, forced expiratory volume in one second (FEV1), forced vital capacity (FVC), forced expiratory time, pulmonary function testing, spirometry
Introduction
Observational studies in which participants are followed over time provide important information about the natural history of disease including risk factors that contribute to disease development and progression (1–3). During such studies, measurement tools, assays, and guidelines for how best to make the measurement of interest may change. When measurement tools and assays change, comparability studies are performed. However, changes in guidelines may be problematic, especially if earlier measurements were made using guidelines no longer considered acceptable.
In 1985–6, 5,115 individuals age 18–30 years were enrolled in the longitudinal Coronary Artery Risk Development in Young Adults (CARDIA) study to assess cardiovascular risk factors in young adults (4, 5). Spirometry was done at the initial visit and at four subsequent visits. During the first 20 years of the study, guidelines for performing spirometry changed. American Thoracic Society (ATS) guidelines published in 1979 did not specify the duration of the forced expiratory maneuver used to determine forced vital capacity (FVC) (6). These guidelines were used for the first 5 years of the CARDIA study. ATS guidelines published in 1987 specified a two second plateau and exhalation time of at least 6 seconds (7), but were not immediately incorporated into standard practice. The most recent spirometry guidelines, jointly developed by the ATS and European Respiratory Society (ERS) and published in 2005 (8), state that an acceptable test in adults must have an exhalation time of at least 6 seconds, while recognizing that this is not always possible.
Based on accepted practices at the time of each visit, the CARDIA study’s manual of operations at years 0, 2 and 5 stated that expiration should be recorded to the plateau (visual) and the plateau should be maintained for one second. The year 10 manual of operations stated that the plateau should be maintained for two seconds. At year 20 an acceptable test required an exhalation time of at least 6 seconds and an acceptable plateau. A possible effect of a short exhalation time and incomplete plateau would be a lower FVC and an elevated FEV1/FVC not truly representative of the individual’s lung health.
Because of previous concerns that end of test criteria may influence spirometry results (9) and a statistical procedure performed on CARDIA data identified a secular trend or methodological artifact that resulted in increasing mean FVC, especially over the first 10 years (10), we re-examined data from the first 10 years of CARDIA applying 2005 ATS-ERS standards. We found that among participants at years 0 and 2 who had acceptable tests based on the manual of operations then in use, approximately 30% had exhalation times less than 6 seconds. Eliminating test results from earlier years that did not meet current performance guidelines would result in the loss of a large amount of valuable data and possibly introduce bias. We therefore sought to determine the prevalence of tests with short exhalations that were otherwise acceptable at each examination, identify participant characteristics associated with short exhalation times, quantify the effect of the short exhalation times on FEV1, FVC and FEV1/FVC, and provide guidance to other investigators analyzing spirometry data from tests performed before adopting the current end of test criteria.
Methods
Participants and Measurements
The data are from CARDIA, a multi-center cohort study in the United States (4, 5). Participants were recruited from the general population, randomly sampled from a prepaid health plan in Oakland CA and from populations in Birmingham, AL, Chicago, IL, and Minneapolis, MN. At year 0, the CARDIA study included 5,115 participants in approximately equal number by ethnic group (black and white), gender, ages (18–24 and 25–30), and education more than or less than or equal to high school. The detailed methods, instruments and quality control procedures are described in previous reports (4, 5).
The analyses included all participants at each of the examinations who had lung function testing and were not pregnant. Demographic characteristics, lifestyle habits (e.g., smoking history), and medical history were collected by self-report using a questionnaire. An asthma diagnosis was made at any examination if the participant had a physician diagnosis of asthma or was taking asthma medication (11).
Lung function was measured at years 0, 2, 5, and 10 using a Collins Survey 8-liter water sealed spirometer and an Eagle II Microprocessor (Warren E. Collins, Inc., Braintree, MA). Year 20 lung function was measured using a dry rolling-seal volume OMI spirometer (Viasys Corp, Loma Linda, CA). The accuracy of each spirometer was validated using a Pulmonary Waveform Generator (MH Custom Design and Manufacturing, Midvale, UT), a computer driven spirometry simulator accurate to within 0.5%. The results obtained on the OMI spirometers exceeded American Thoracic Society (ATS) criteria for accuracy and precision (12). The four functional Collins Survey spirometers used at the earlier visits were also tested with the waveform generator. They too exceeded ATS criteria for accuracy and precision. A study comparing the Collins and OMI spirometers was performed on 25 volunteers at the LDS Hospital (Salt Lake City, UT) and demonstrated excellent consistency between the old and new spirometers. The average difference between the spirometers was 6 ± 146 ml (mean ± SD) for FVC and 21 ± 135 ml for FEV1. The standard deviations were smaller than the intra-session repeatability (150 ml) recommended by the ATS/ERS (8)
Standard quality control and testing procedures were followed at all examinations (6–8). We analyzed the largest FVC and FEV1 from at least five maneuvers. Data are represented as a percent of the predicted value (13). We only used results from test sessions in which at least one spirometry measurement met acceptability criteria at the time of the test. Analyses were performed on data from CARDIA participants who attended the initial (year 0) exam and any of the subsequent exams.
Statistical Methods
Body mass index was computed as weight (kg) divided by height squared (m2). Smoking status was categorized into three groups: never smoker, former smoker, current smoker.
Factors associated with test sessions having short exhalation times, defined as no trial lasting 6 or more seconds but that were acceptable based on the then current manual of procedures, were assessed by univariate analysis using Chi-square tests for categorical variables and t-tests or ANOVA for continuous variables. Logistic regression was used to assess multivariable associations.
To develop equations for adjusting the FVC value when the exhalation time was less than six seconds but the test was otherwise acceptable (e.g., there was an adequate plateau), the year 0 pulmonary function dataset was analyzed using each acceptable test. The 4,549 participants who underwent spirometry testing at baseline produced 30,690 records. Records were excluded if there was evidence of airway obstruction (FEV1/FVC ratio <0.7), one or more covariates (FEV1, height, age, exhalation time) were missing, there was only one acceptable test, exhalation times were less than 2 seconds or more than 8 seconds, or FVC values were in the top and bottom 1 percent of test results. This left 12,883 exhalations in 4,412 participants available for analysis. Most of the exclusions were because of missing data.
The data were clustered within participant and analyzed using Generalized Estimating Equations (GEE) (14) with observed FVC in repeated trials as the dependent variable. The GEE model correlated data from several expiratory maneuvers performed by the same participant, clustered within participant. We modeled the association between spirometry values and exhalation time by analyzing the same trial containing one or more exhalations, rather than using the maximum FVC, FEV1 and exhalation time coming from different trials. We stratified by race and sex and used exhalation time, age, FEV1 and height as independent variables based on their high statistical association with FVC. We calculated FVC for both 6 and 8 second exhalation times in those with exhalation times of 2 to 5 seconds. The calculated FVC values were compared with the measured values and with the predicted values from the NHANES III equations developed by Hankinson et al [11].
Results
Participant characteristics
Study participant characteristics are shown in table 1. At entry, the average age was 24.9 years and participants were evenly distributed by sex and race. The average body mass index (BMI) was 24.6, nearly 60% were current or former cigarette smokers, and the mean values for FVC, FEV1 and FEV1/FVC were normal. Over 20 years the percentage of female and white participants increased, the BMI increased, and the proportion of current smokers decreased while past and never smokers increased.
Table 1.
Participant Characteristics
| Study Year | 0 (1985–6) |
2 (1987–8) |
5 (1990–1) |
10 (1995–6) |
20 (2005–6) |
|---|---|---|---|---|---|
| Number | 4549 | 4455 | 4257 | 3674 | 3416 |
| Age – years (mean ± SD) |
24.9 ± 3.6 | 26.9 ± 3.6 | 30.0 ± 3.6 | 35.0 ± 3.6 | 45.1 ± 3.6 |
| Males (%) | 46.4 | 45.3 | 45.0 | 45.0 | 43.0 |
| Race – white (%) | 49.4 | 51.0 | 51.5 | 52.0 | 53.8 |
| Education - ≤ high school (%) |
37.8 | 33.7 | 31.7 | 28.8 | 23.7* |
| BMI (mean ± SD) |
24.6 ± 5.0 | 25.2 ± 5.3 | 26.2 ± 5.9 | 27.5 ± 6.6 | 29.4 ± 7.0** |
| Smoking - current/ previous/never (%) |
29.8/29.9/40.3 | 29.4/30.0/40.6 | 28.5/29.7/41.8 | 24.7/31.9/43.4 | 18.9*/36.2/44.9 |
| FEV1 - % predicted (mean ± SD) |
97.7 ± 11.8 | 97.5 ± 12.1 | 99.1 ± 13.2 | 98.3 ± 13.0 | 93.7 ± 14.6** |
| FVC - % predicted (mean ± SD) |
100.3 ± 11.5 | 100.3 ± 11.8 | 101.5 ± 12.4 | 101.5 ± 12.4 | 95.8 ± 13.9** |
| FEV1/FVC (mean ± SD) |
0.83 ± 0.06 | 0.82 ± 0.07 | 0.82 ± 0.07 | 0.82 ± 0.10 | 0.79 ± 0.07** |
Mean ± SD unless otherwise noted.
The data are from individuals who underwent pulmonary function testing and had measurements of exhalation time available for analysis.
p<0.05,
p<0.001 compared to the baseline examination
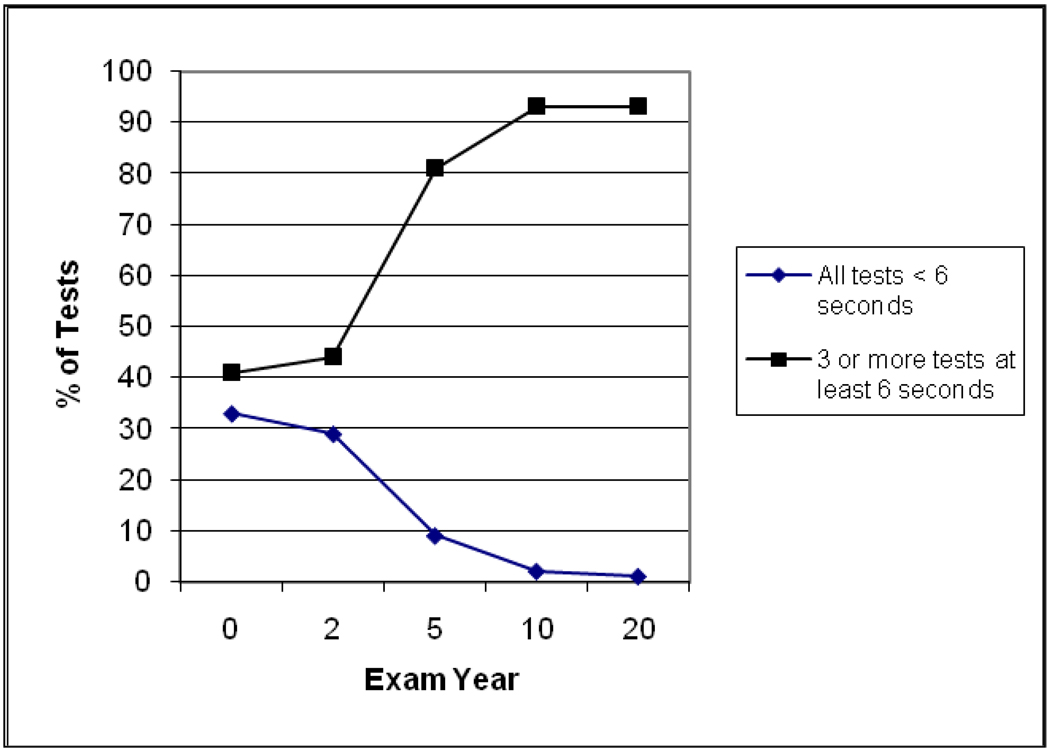
The percentage of participants with acceptable spirometry tests based on the then current manual of operations, but who did not have any exhalations lasting at least 6 seconds at years 0, 2, 5, 10 and 20 was 33%, 29%, 9%, 2% and 1%, respectively (fig. 1). The percentage of participants with three or more acceptable tests lasting ≥6 seconds was 41%, 44%, 81%, 93% and 93% at the same times. As the percentage of tests with exhalations lasting <6 seconds was very low at years 10 and 20, the subsequent analyses were limited to years 0, 2 and 5.
Figure 1.
Association between examination year and the percentage of participants with "unacceptably short" forced vital capacity tests (all tests with exhalation time <6 seconds) based on post-1987 ATS guidelines (diamonds) and with 3 or more tests ≥6 seconds (squares).
Participants with no exhalations lasting at least 6 seconds at years 0, 2 and 5 were more likely to be younger, female, and thinner than those with at least one exhalation ≥6 seconds (table 2). Those with no exhalations ≥6 seconds tests had lower FVC values, but higher FEV1 and FEV1/FVC values. The two groups did not differ by race, education level, smoking status, or presence of current asthma. Multivariate analysis confirmed the association of female sex, younger age, lower FVC and higher FEV1/FVC with short exhalations.
Table 2.
Association of Exhalation Time and Participant Characteristics at Years 0, 2 and 5
| Study Year | 0 | 2 | 5 | |||
|---|---|---|---|---|---|---|
| Trials with exhalation time ≥ 6 seconds |
0 | ≥ 1 | 0 | ≥1 | 0 | ≥ 1 |
| Number | 1287 | 3262 | 1269 | 3186 | 397 | 3860 |
| Age – years | 23.9 ± 3.7* | 25.3 ± 3.5 | 26.2 ± 3.7* | 27.2 ± 3.5 | 28.6 ± 3.8* | 30.1 ± 3.6 |
| Male (%) | 35.1* | 50.8 | 29.6* | 51.6 | 30.5* | 46.5 |
| White (%) | 48.0 | 49.9 | 45.2 | 53.4 | 48.1 | 51.9 |
| Education - ≤ high school (%) | 42.9 | 35.9 | 34.2 | 33.4 | 37.3 | 31.1 |
| BMI | 22.6 ± 3.7* | 25.4 ± 5.2 | 23.7 ± 4.8* | 25.7 ± 5.4 | 23.1 ± 5.1* | 26.5 ± 5.9 |
| Smoking - current/previous/never (%) |
27.0/27.8/45.2 | 30.9/30.8/38.3 | 26.3/27.9/45.8 | 30.6/30.9/38.5 | 27.7/26.2/46.1 | 28.6/30.1/41.3 |
| FEV1 - % predicted | 98.8 ± 11.4* | 97.3 ± 11.9 | 98.6 ± 11.4* | 97.1 ± 12.3 | 100.8 ± 15.3** | 99.0 ± 13.0 |
| FVC - % predicted | 98.0 ± 11.3* | 101.2 ± 11.5 | 98.2 ± 11.7* | 101.2 ± 11.7 | 97.7 ± 13.6* | 101.9 ± 12.2 |
| FEV1/FVC | 0.87 ± 0.05* | 0.82 ± 0.06 | 0.86 ± 0.06* | 0.81 ± 0.06 | 0.87 ± 0.08* | 0.81 ± 0.06 |
| Asthma (current) | 4.0 | 4.3 | 4.6 | 4.8 | NA# | NA |
Mean ± SD unless otherwise noted
Not available – participants not asked about asthma at this visit
p < 0.001,
p < 0.02 compared to those at the same study year with at least one exhalation of 6 or more seconds
The association between age and FVC at years 0 and 2 was examined in subjects who had one or more exhalations lasting ≥6 seconds versus those who had none. An age cut-point could not be identified below which individuals with no exhalation times ≥6 seconds had FVC values comparable to those with at least one exhalation ≥6 seconds (data not shown).
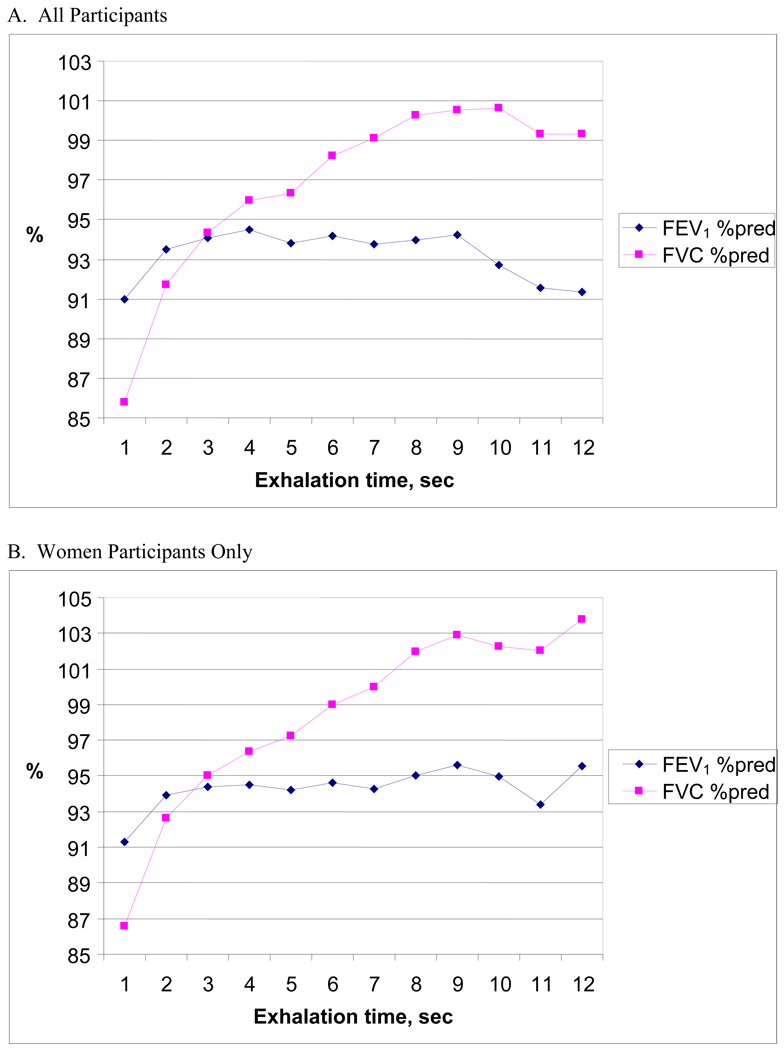
The association between exhalation time and FEV1 and FVC was examined within each participant using the generalized estimating equations model (14). We found that the FVC increased as exhalation time increased with a plateau value being reached at 8 seconds (fig. 2A; squares). The correlation between exhalation time and FVC was 0.75. For exhalation times between 3 and 8 seconds, each additional second of exhalation time was associated with approximately a 1% increase in FVC. These findings were similar when women were analyzed separately (figure 2B). FEV1 was not influenced by exhalation times between 2 and 8 seconds. However, those with exhalation times longer than 8 seconds had lower FEV1 values (fig. 2A; diamonds).
Figure 2.
Association between exhalation time and FVC (squares) and FEV1 (diamonds) for all participants (A) and for only the female participants (B) at year 0.
We used generalized estimating equations (GEE) that included measured FVC and FEV1, actual exhalation time, age and height to adjust FVC values obtained from tests with short exhalation times but were otherwise acceptable (e.g., had the required plateau). The equations for the 4 race-sex groups are shown in table 3. Using these equations we calculated the FVC if an exhalation <6 seconds had been prolonged to either 6 or 8 seconds. On average, the calculated FVC was 1.2% (47 ± 259 ml) and 2.7% (110 ± 263 ml) higher than the measured FVC when 6 and 8 second exhalation times were used.
Table 3.
Equations to Adjust FVC Values from Tests with Short Exhalation Times
| Group | Estimated FVC (liters) as a function of exhalation time |
|---|---|
| White males | −3.03480 + 0.04490*exhalation time − 0.00003*age + 0.02634*height (cm) + 0.78110*FEV1 |
| White females | −2.38537 + 0.03321*exhalation time + 0.00758*age + 0.02019*height (cm) + 0.78477*FEV1 |
| Black males | −2.24801 + 0.04734*exhalation time + 0.00373*age + 0.01788*height (cm) + 0.85956*FEV1 |
| Black females | −1.72559 + 0.03177*exhalation time + 0.00116*age + 0.01523*height (cm) + 0.83039*FEV1 |
The equations to calculate predicted FVC were developed using generalized estimating equations (GEE) that included measured FVC, FEV1, exhalation time, age and height. To calculate the adjusted FVC value for otherwise acceptable FVC tests with an exhalation time of at least 2 seconds but less than 6 seconds, an exhalation time of 6 seconds or more is inserted in the above equations.
To gain additional insight into the factor(s) contributing to the short exhalation times, we studied individuals with no exhalations lasting ≥6 seconds at both years 0 and 5 (N=446) and those with no exhalations ≥6 seconds at year 0 but at least one exhalation ≥6 seconds at year 5 (N=1,198) (table 4). The two groups did not differ by age or race, but those with short exhalations at both years were more likely to be female and thinner at year 5. The number of individuals with only short exhalations decreased substantially over 5 years in the absence of any change in test procedures.
Table 4.
Comparison of Participants with All Exhalation Times < 6 Seconds at Both Years 0 and 5 versus All < 6 Seconds only at Year 0
| Short Exhalations |
Year 0 and Year 5 | Year 0 Only |
|---|---|---|
| Number (% of total) |
446 (10.5%) | 1198 (28.0%) |
| Age – years (at Year 0) |
24.0 ± 3.7 | 24.4 ± 3.7 |
| White (%) | 227 (50.9%) | 585 (48.8%) |
| Female (%) | 309 (69.7%)* | 726 (60.6%)* |
| BMI | Y0: 22.5 ± 4.1 Y5: 23.6 ± 4.8# |
Y0: 23.3±4.1 Y5: 25.2±5.1 t |
| FEV1 - % predicted |
Y0: 99.3 ± 11.2 Y5: 101.4 ± 14.4** |
Y0: 98.6 ± 11.5 Y5: 99.4 ± 12.4 |
| FVC - % predicted |
Y0: 91.8 ± 12.8 Y5: 93.9 ± 14.1** |
Y0: 94.7 ± 12.8 Y5: 96.9 ± 13.7t |
Mean ± SD unless otherwise noted
p < 0.0001 compared to males
p < 0.05,
p < 0.0003,
p < 0.0001 compared to year 0
Discussion
Lung function measurements made before widespread acceptance of the recent guidelines for determining the acceptability of a forced vital capacity test had end of test criteria that are different from those used today. The earlier test results may not, therefore, be comparable to recent ones and changes seen over time may reflect differences in test procedures rather than participant-specific, time-dependent changes. Pistelli and colleagues previously reported that end of test criteria can influence the FVC (9). However, the literature provides little guidance about how to reconcile older and recent study results when test procedures change, nor what participant characteristics may influence the effects of different end of test criteria.
In our analysis of the CARDIA spirometry dataset, we confirmed that end of test criteria influence spirometry results. We also identified participants who were most likely to have results influenced by previous end of test criteria that did not require a minimum 6 second exhalation – young adults, especially females. We believe these findings have important implications for interpreting lung function data from longitudinal studies begun 20 or more years ago and which used end of test criteria that are not considered acceptable today.
We initially thought the high proportion of tests with exhalations less than 6 seconds during the first 5 years of the CARDIA study was due to using a one second visual plateau as the end of test criterion. Although this may have contributed, it does not appear to be the sole factor as the same test procedures were followed at years 0, 2 and 5, during which time the proportion of tests with short exhalations decreased from 33% to 9%. We also considered a training effect on either the staff or the participants, but we believe this is unlikely because the time between testing at years 0 and 2 was shorter than that between years 2 and 5, while the percentage of tests with short exhalations was unchanged between years 0 and 2 and decreased by more than 70% between years 2 and 5, Further, the manual of operations, equipment, and training were identical at all three times.
The spirometry guidelines published in 1979 by the American Thoracic Society state that “End of test will occur when the average flow over a 0.5 second interval is less than 50 ml/sec or when the volume change in a 0.5 second interval is less than 25 ml” (6). There is no mention of test duration. Subsequent guidelines published in 1987 recommend: “an obvious plateau in the volume-time curve resulting in no change in volume for AT LEAST 2 seconds or an exhalation time of at least 6 seconds ” (7). The 1994 ATS guidelines added: “There are circumstances (e.g., the testing of children, young adults, and some restricted patients) where shorter exhalation times are acceptable.” However, neither these documents nor the one published in 2005 (8), which allows the tester to use a plateau on the volume-time curve as an end of test criterion, provide guidance on interpreting the results obtained from tests with exhalation times less than 6 seconds. The documents also do not discuss the possibility of adjusting earlier FVC values in longitudinal epidemiology studies when a test has a short exhalation time but is otherwise acceptable.
To address this issue we analyzed all acceptable forced expiratory maneuvers performed by participants at year 0 and found that the FVC increased with exhalation time up to 8 seconds. We also found that those with exhalation times >8 seconds had lower FEV1 values. In some subjects this may reflect the presence of airflow obstruction not identified by a FEV1/FVC < 0.70. Using the year 0 data, we developed equations to estimate the FVC from acceptable tests (a plateau was achieved and all other quality control parameters were met) with exhalation times less than 6 seconds. The values obtained using these equations with a projected exhalation time of 8 seconds approximated the predicted values published by Hankinson et al (13). We previously reported a trend in FVC and FEV1 over spirometric examinations at years 0, 2, 5 and 10, based on a mathematical technique of looking at differences in these measures in people of the same age assessed at different examinations (15). We added 53 ml, 54 ml, and 16 ml to the predicted FVC at year 0, 2, and 5, respectively (10). These adjustments are similar to those obtained in the present study by examining the implications of protocol differences between examinations.
It is possible the association between longer exhalation times and larger FVC values was due to larger inhalation volumes, as reflected by the positive association between FEV1 and FVC (table 3). Alternatively, the association between a longer exhalation and larger FVC may be due to instrument factors such as the greater likelihood of inadvertent shaking of the tubing connecting the participant to the machine during the longer time. However, it is unclear why either of these factors would have played a greater role in the first 2 years of the study than in subsequent years, especially during the 10 years in which the same spirometers were used. It is also plausible that the FEV1 is correct and the FVC somewhat small based on failure to expel part of the residual air because of a shorter exhalation time.
We are unable to explain why the participants in the CARDIA study with short exhalations were younger and more likely to be female. However, anecdotal clinical experience supports this observation. One consideration is that early glottis closure occurs more frequently during forced expiration in younger adults, especially young women. Yet, as far as we know, there are no studies to substantiate this possibility.
The FVC adjustment we propose has important implications for longitudinal assessment of lung function change over time, especially in studies started more than 20 years ago that used end of test criteria like those in the early years of the CARDIA study. As these studies are an important source of information about early life factors that contribute to age- and time-dependent changes in lung function, having the most accurate assessment of lung function is vital to correctly interpreting the results. Although one can debate the biological and clinical significance of the modest differences in FVC between the measured values and the adjusted values obtained after using the proposed equations (about 110 ml), this difference equals about 4 years of lung function decline in healthy nonsmokers (13, 16) and should be of interest to researchers.
The strengths of this study include the large sample size, excellent retention of participants, careful documentation of the spirometry testing procedures, strict quality control procedures, and use of the same equipment and many of the same technicians during the first 10 years of the study. Limitations include loss of 15% of the participants between years 0 and 5, and the change in the characteristics of those who remained in the study for the full 20 years. In addition, the large standard deviations in the equations created to adjust for short exhalations indicate they are best suited for large epidemiology studies, not for clinical care.
In conclusion, analysis of the spirometry data from the CARDIA study of young adults clearly demonstrates that changing end of test criteria in a longitudinal study can influence FVC and FEV1/FVC; younger adult and female participants are most likely to be effected in studies that used only a plateau on the volume-time curve to terminate a test; equations using existing study data can be developed to adjust otherwise acceptable tests with short exhalations from older studies; and these adjusted values may better reflect the lung health of the participants.
Acknowledgments
Supported by National Heart, Lung, and Blood Institute contracts N01-HC-48047, N01-HC-48048, N01-HC-48049, N01-HC-48050 (CARDIA field centers), N01-HC-95095 (CARDIA Coordinating Center), and N01-HC045134 Reading Center (CARDIA Pulmonary Reading Center)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dawber TR, Meadors GF, Moore FE., Jr Epidemiological approaches to heart disease: the Framingham Study. American journal of public health and the nation's health. 1951 Mar;41(3):279–281. doi: 10.2105/ajph.41.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Appleyard M, Hansen AT, Schnohr P, Jensen G, Nyboe J. The Copenhagen Heart Study. A book of tables with data from the first examination (1976–78) and a five-year follow-up (1981–1985) Scand J Soc Med. 1989 Suppl 41:1–160. [PubMed] [Google Scholar]
- 3.Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, et al. The Cardiovascular Health Study: design and rationale. Annals of epidemiology. 1991 Feb;1(3):263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 4.Hughes GH, Cutter G, Donahue R, Friedman GD, Hulley S, Hunkeler E, et al. Recruitment in the Coronary Artery Disease Risk Development in Young Adults (Cardia) Study. Control Clin Trials. 1987 Dec;8(4 Suppl):68S–73S. doi: 10.1016/0197-2456(87)90008-0. [DOI] [PubMed] [Google Scholar]
- 5.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, Jr, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 6.ATS statement--Snowbird workshop on standardization of spirometry. Am Rev Respir Dis. 1979 May;119(5):831–838. doi: 10.1164/arrd.1979.119.5.831. [DOI] [PubMed] [Google Scholar]
- 7.Standardization of spirometry--1987 update. Statement of the American Thoracic Society. Am Rev Respir Dis. 1987 Nov;136(5):1285–1298. doi: 10.1164/ajrccm/136.5.1285. [DOI] [PubMed] [Google Scholar]
- 8.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005 Aug;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 9.Pistelli G, Carmignani G, Paoletti P, Di Pede F, Viegi G, Carrozzi L, et al. Comparison of algorithms for determining the end-point of the forced vital capacity maneuver. Chest. 1987;91(1):100–105. doi: 10.1378/chest.91.1.100. [DOI] [PubMed] [Google Scholar]
- 10.Thyagarajan B, Jacobs DR, Jr, Apostol GG, Smith LJ, Jensen RL, Crapo RO, et al. Longitudinal association of body mass index with lung function: the CARDIA study. Respiratory Research. 2008;9:31. doi: 10.1186/1465-9921-9-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beckett WS, Jacobs DR, Jr, Yu X, Iribarren C, Williams OD. Asthma is associated with weight gain in females but not males, independent of physical activity. Am J Respir Crit Care Med. 2001 Dec 1;164(11):2045–2050. doi: 10.1164/ajrccm.164.11.2004235. [DOI] [PubMed] [Google Scholar]
- 12.Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med. 1995 Sep;152(3):1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 13.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999 Jan;159(1):179–187. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 14.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 15.Jacobs DR, Jr, Hannan PJ, Wallace D, Liu K, Williams OD, Lewis CE. Interpreting age, period and cohort effects in plasma lipids and serum insulin using repeated measures regression analysis: the CARDIA Study. Statistics in Medicine. 1999;18(6):655–679. doi: 10.1002/(sici)1097-0258(19990330)18:6<655::aid-sim62>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 16.Lange P, Groth S, Nyboe J, Mortensen J, Appleyard M, Jensen G, et al. Decline of the lung function related to the type of tobacco smoked and inhalation. Thorax. 1990;45(1):22–26. doi: 10.1136/thx.45.1.22. [erratum appears in Thorax 1990 Mar;45(3):240] [DOI] [PMC free article] [PubMed] [Google Scholar]