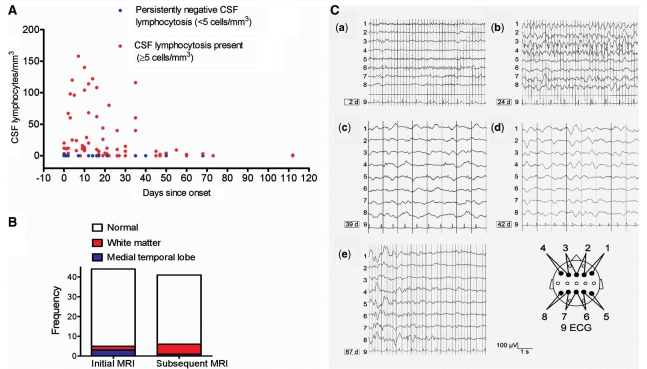
Figure 3.
Imaging, cerebrospinal fluid and EEG results. (A) The extent of CSF lymphocytosis (>5 cells/mm3, red dots) observed at different time points across all patients. Thirt-two percent of patients had persistently negative CSF lymphocytosis (<5 cells/mm3, blue dots). (B) MRI was commonly normal (white) and abnormalities were mainly restricted to white matter tracts (n = 6, red) and hippocampi (n = 4, blue) both at initial (median Day 1) and subsequent (median Day 25) imaging. (C) Serial electroencephalograms (EEGs) of a 17-year-old non-paraneoplastic female NMDAR-antibody-positive patient, not within our cohort of 44 cases. Bipolar transverse EEG recordings are shown in the scheme below. (a) EEG was normal after the patient had experienced a generalized convulsion. From Day 21–24, she suffered from frequent complex partial seizures; (b) EEG showed frequent, in part long-lasting frontal epileptiform spike-wave activity; (c–d) subsequently, there was continuous diffuse high-amplitude slowing without epileptiform potentials. From Day 39 on, no further seizures were observed. On Day 42, anti-epileptic therapy consisted of phenytoin (blood level: 25.4 µg/ml), phenobarbital (29.7 µg/ml) and lorazepam (2 mg daily dose). Glucocorticosteroids were instituted on Day 38. From Day 56, the patient recovered; and (e) normal EEG appearances recurred in sections in between abnormally high waves.