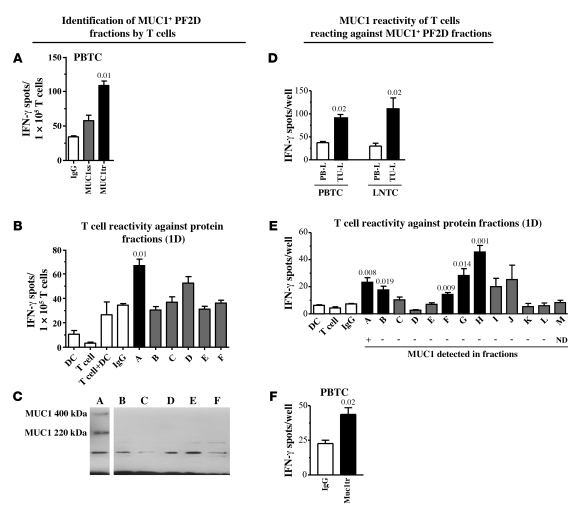
Figure 2. Identification of MUC1+ protein fractions by MUC1-reactive T cells from patients with head and neck cancer.
(A) T cell reactivity of patient HN-1 against DCs pulsed with synthetic, MUC1-derived long peptides from the signaling sequence (MUC1ss) or the tandem repeat region (MUC1tr) as revealed by IFN-γ ELISPOT assay. (B) T cell reactivity of HN-1 against DCs pulsed with 1D fraction A but not B–F of the patient’s autologous tumor. (C) Detection of MUC1 protein in PF2D fraction A by IP. Lanes were run on the same gel but were noncontiguous, as indicated by the black line. (D) T cell reactivity of patient HN-2 against TU-L–pulsed DCs as revealed by IFN-γ ELISPOT assay. (E) T cell reactivity of HN-2 against DCs pulsed with 1D fractions (A–M) of the patient’s autologous tumor. Corresponding results of MUC1 protein detection by MUC1-specific IP are indicated for each PF2D fraction below (+, MUC1-positive; –, no detection of MUC1; ND, not determined). MUC1 could only be detected in fraction A. (F) T cell reactivity of patient HN-2 against DCs pulsed with synthetic, MUC1-derived long peptide (tandem repeat region, MUC1tr) as revealed by IFN-γ ELISPOT assay. Negative controls are denoted by white bars; statistically significant differences versus IgG or PBMC lysate (PB-L) control, as appropriate, are indicated by black bars; gray bars indicate nonsignificant responses. PBTC, peripheral blood–derived T cells; LNTC, tumor-draining lymph node–derived T cells.