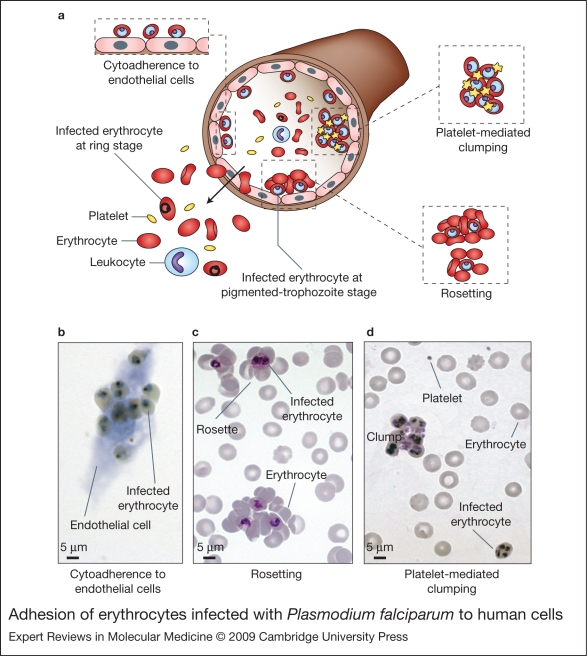
Figure 2.
Adhesion of Plasmodium falciparum-infected erythrocytes to human cells. (Legend; See previous page for figure) (a) Schematic representation of the adhesion properties of P. falciparum-infected erythrocytes to different host cells. Erythrocytes infected with mature forms of P. falciparum parasites (pigmented trophozoites and schizonts) have the ability to bind to a range of host cells, such as endothelium, uninfected erythrocytes (rosetting) and platelets (platelet-mediated clumping). The adhesion of infected erythrocytes to endothelial cells leads to their sequestration in the microvasculature of various organs and tissues such as heart, lung, brain, muscle and adipose tissue. As a result, only erythrocytes carrying young ring forms of the parasite are detected in human peripheral blood samples. Although cytoadherence and sequestration of mature infected erythrocytes in the microvasculature occur in all infections, several specific adhesive phenotypes have been associated with severe pathological outcomes of malaria, such as the formation of rosettes and the adhesion of infected erythrocytes to brain endothelium. Rosetting and platelet-mediated clumping are phenotypes that are displayed by some but not all P. falciparum isolates in vitro. In vivo, it is thought that the formation of rosettes and clumps will be accompanied by adhesion to endothelial cells and sequestration in the microcapillaries (Ref. 115). (b) Cytoadherence of infected erythrocytes to in-vitro-cultured brain endothelial cells, visualised by light microscopy after Giemsa staining. (c) Rosettes detected in in vitro P. falciparum cultures, observed after preparation of Giemsa-stained thin smears and light microscopy. (d) Platelet-mediated clumps of infected erythrocytes formed after in vitro co-incubation of parasite cultures with platelets, observed by Giemsa-stained thin smears and light microscopy.