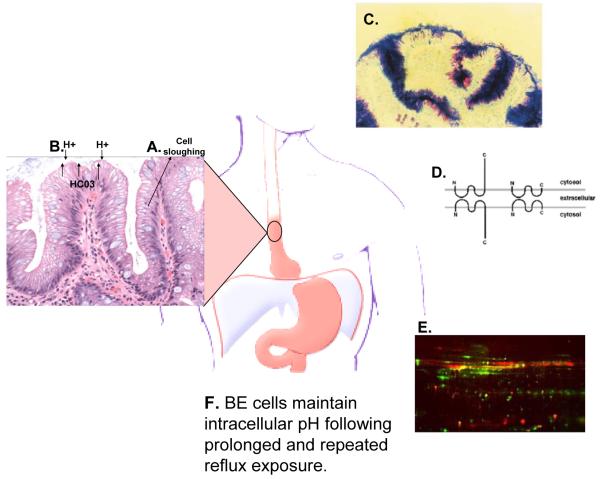
Figure 1. Barrett’s specialized intestinal metaplasia and mucosal defence.
(A) Specialized intestinal metaplasia is a well differentiated epithelium with crypt architecture in which putative stem cells residing at the base give rise to proliferating transient amplifying cells and differentiated cells that are sloughed into the lumen. This architecture has been proposed to be tumor suppressive because mutations occurring in transient amplifying or differentiated non-stem cells would be shed from the body before they could accumulate the serial mutations leading to cancer10. (B) The intestinal metaplasia also secretes anions, including bicarbonate, at levels more than fivefold greater than oesophageal squamous epithelium11. (C) Specialized intestinal metaplasia also secretes thick adherent mucus not present in normal squamous oesophageal cells12. Ultrastructural studies have shown that mucus secretion can be disrupted in Barrett’s oesophagus at increased risk of progression to oesophageal adenocarcinoma, including those with evidence of chromosomal instability and aneuploidy16. (D) Barrett’s oesophagus has claudin-18 tight junctions that provide greater protection against acid permeation than the claudin-18 deficient tight junctions of the oesophageal squamous epithelium13. (E) Barrett’s oesophagus also overexpresses genes involved in mucosal defence and repair14, and (F) Barrett’s oesophageal cells maintain physiologic intracellular pH following prolonged and repeated reflux exposure15. Abbreviation: Barrett’s oesophagus (BE).