Classically orthostatic tremor and the associated symptom of intense unsteadiness disappear with ambulation1. Here we describe a patient with cerebellar atrophy who presented with slow orthostatic tremor, which disappeared when walking forwards, but persisted when walking backwards.
A 70 year old female initially presented with unsteadiness and symptomatic axial tremor on standing. These problems had progressed over a period of 18 months and had caused her to fall on numerous occasions. The intense feeling of unsteadiness was always apparent when standing, walking backwards or turning and was relieved by the use of a support, walking forwards or sitting. She therefore required a walking stick outside the house. Although the axial tremor, which produced a sensation as though her whole body was shaking, was only occasionally symptomatic, it always occurred when standing. In the three months before neurological assessment her family had noticed that her speech was becoming slurred.
She had a past medical history of polymyalgia rheumatica (previously treated with steroids for 15 months), psoriasis, diverticulosis and ischaemic heart disease. Her regular medications were aspirin, atenolol and simvastatin. She smoked eight cigarettes a day but did not drink alcohol.
Bedside examination revealed mild cognitive impairment (Addenbrooke’s cognitive examination 90/100), mild cerebellar dysarthria, bilateral phasic nystagmus, mild synkinetic rigidity, hyperreflexia, postural upper limb tremor, mild dysmetria in the left UL, bilateral dysdiadochokinesis and bilateral heel-shin ataxia. However, there was no muscle wasting or weakness, plantar responses were flexor, joint position sensation was intact in the toes and there was no hypokinesia.
During forward ambulation she took small steps, but the gait was not broad based or ataxic, and tandem walking, though unstable, was achieved without support. Turns were slow and unstable. When she walked backwards she became markedly unstable, stumbling or falling occasionally, and therefore could only do so very slowly and deliberately, taking one step at a time. As a consequence her backward gait had an adhesive quality (i.e. reminiscent of the ‘moonwalk’ popularised by the late Michael Jackson). Antepulsion was negative but retropulsion was positive.
There was evidence of cerebellar atrophy on MRI and motor evoked potentials showed prolonged lower limb central motor conduction times (28.7ms; normal range 13.1±3.8ms). Autonomic function tests were normal and an Ioflupane (123I) - SPECT scan showed no evidence of a nigrostriatal dopaminergic deficiency.
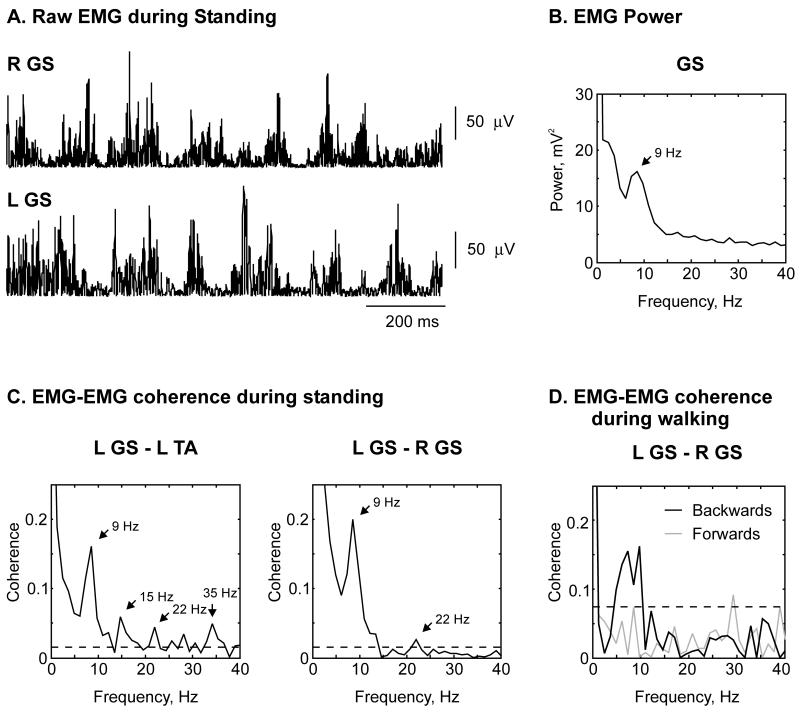
Electromyography (EMG) showed no evidence of leg tremor while seated, either at rest or with legs extended and feet plantar flexed, but as the patient stood tremor appeared in the legs. Raw rectified EMG recorded using adhesive electrodes from right and left gastrocnemius-soleus (GS) muscles (gain 5000; band pass filtered 30Hz-2kHz; 5kHz digitization) whilst standing is shown in Figure 1A. Each 1s long segment of data contained eight or nine 50-100ms bursts of EMG, which appeared synchronous. Frequency domain analysis (see power spectrum in Figure 1B) confirmed that the dominant frequency was ~9Hz. Coherence analysis and measurement of significance was performed as previously published2. This confirmed that there was significant unilateral and bilateral EMG-EMG coherence not only at ~9Hz, but also significant unilateral EMG-EMG coherence peaks at 15Hz and 22Hz and 35Hz, and a significant bilateral EMG-EMG coherence peak at 22Hz suggesting that other common frequencies might also be driving lower limb tremor (Figure 1C). During forward walking there was no significant bilateral EMG-EMG coherence at any frequency (grey line; figure 1D). However, during backward locomotion (at approximately the same speed as forward locomotion, 2 paces per second), when the patient was most unsteady, there was significant bilateral EMG-EMG coherence at tremor frequency (black line; figure 1D).
Figure 1.
A. Raw rectified EMG traces recorded from right and left gastrocnemius-soleus (GS) muscles during standing. B. Left GS EMG power during standing. C. Unilateral EMG-EMG coherence between left tibialis anterior (TA) and left GS and bilateral EMG-EMG coherence between left and right GS during standing. D. Bilateral coherence during forward (grey) and backward (black) walking. Dashed lines show significance limits.
Orthostatic tremor (OT) is a rare form of task specific tremor affecting the legs and trunk. It only appears on standing, is associated with a profound and disabling sense of unsteadiness and is relieved by sitting, walking or the use of a support. Two types of OT are recognized: fast/primary OT, characterised by bursts of muscle activity at 13-18 Hz1; and slow OT, with 70-120ms EMG bursts at frequencies <12Hz3,4. Slow OT has been described in patients with Parkinson’s disease and parkinsonism4, cerebellar lesions5 and cerebellar atrophy6, but can occur in the absence of primary or associated neurological disease3. In slow OT EMG coherence analysis reveals significant bilateral coupling at tremor frequency between EMG recorded from lower limb, upper limb and axial muscles (coherence 0.2-0.8), which is absent in controls under normal conditions7 and patients with orthostatic myoclonus4, and is not as strong as that seen in fast/primary OT (coherence 0.8-1).
The observation that OT does not disappear, but persists, or worsens when walking backwards is novel and not only emphasizes the pathophysiological differences between slow and fast orthostatic tremor, but may provide further clues as to the origins of slow OT.
Acknowledgements
Financial disclosure (related to research covered in this article): This research was funded by The Wellcome Trust and UK Medical Research Council.
MRB is employed by the National Health Service (NHS) and National Institute for Health Research (NIHR).
REJ is employed by the NHS. ERW and SNB are employees of Newcastle University.
Financial disclosure (previous 12 months): Research activities of MRB, ERW and SNB are supported by grants from The Wellcome Trust, MRC, BBSRC, EPSRC and UCB Pharma held by SNB.
SNB is engaged as a consultant to Cambridge Laboratories on an unrelated project. SNB and MRB have received travel grants from UCB Pharma.
Footnotes
The authors have no conflict of interest.
References
- 1.Heilman KM. Orthostatic tremor. Archives of neurology. 1984;41(8):880–881. doi: 10.1001/archneur.1984.04050190086020. [DOI] [PubMed] [Google Scholar]
- 2.Evans CM, Baker SN. Task-dependent intermanual coupling of 8-Hz discontinuities during slow finger movements. Eur J Neurosci. 2003;18(2):453–456. doi: 10.1046/j.1460-9568.2003.02751.x. [DOI] [PubMed] [Google Scholar]
- 3.Uncini A, Onofrj M, Basciani M, Cutarella R, Gambi D. Orthostatic tremor: report of two cases and an electrophysiological study. Acta neurologica Scandinavica. 1989;79(2):119–122. doi: 10.1111/j.1600-0404.1989.tb03722.x. [DOI] [PubMed] [Google Scholar]
- 4.Leu-Semenescu S, Roze E, Vidailhet M, et al. Myoclonus or tremor in orthostatism: an under-recognized cause of unsteadiness in Parkinson’s disease. Mov Disord. 2007;22(14):2063–2069. doi: 10.1002/mds.21651. [DOI] [PubMed] [Google Scholar]
- 5.Baker M, Fisher K, Lai M, Duddy M, Baker S. Slow orthostatic tremor in multiple sclerosis. Mov Disord. 2009;24(10):1550–1553. doi: 10.1002/mds.22630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Setta F, Jacquy J, Hildebrand J, Manto MU. Orthostatic tremor associated with cerebellar ataxia. Journal of neurology. 1998;245(5):299–302. doi: 10.1007/s004150050222. [DOI] [PubMed] [Google Scholar]
- 7.Sharott A, Marsden J, Brown P. Primary orthostatic tremor is an exaggeration of a physiological response to instability. Mov Disord. 2003;18(2):195–199. doi: 10.1002/mds.10324. [DOI] [PubMed] [Google Scholar]