Abstract
Background
We prospectively evaluated the incidence and possible factors causing intramuscular injection during lumbar sympathetic ganglion block and compared the multiple needle technique to the single technique to obtain a profound and complete block effect.
Methods
Among 83 patients, 58 patients (group A, n = 27, multiple needle technique and group B, n = 31, single needle technique) were reevaluated for the changes of skin temperature (Ts) and mean segment of longitudinal contrast spread. After injecting the contrast agent, the incidence of psoas muscle injection and the change of Ts was compared between two groups.
Results
The incidence of psoas muscle injection was 21.3% (46/216) and it was associated with the level of injection (L2) significantly (χ2 = 14.773, P = 0.001). DTpost (postblock temperature difference between ipsilateral and contralateral great toe, 4.6 ± 2.8℃, 1.8 ± 1.6℃, P < 0.001 for group A and B) and DTnet (DTpost - DTpre, 3.9 ± 2.7℃, 1.5 ± 1.5℃, P < 0.001 for group A and B) was significantly higher in group A. The mean segment of longitudinal contrast spread was 8.1 ± 0.9 for group A and 3.2 ± 1.6 for group B (P < 0.001).
Conclusions
The LSGB at the L2 level showed the lowest incidence of psoas muscle injection of contrast. Multiple needle approach showed more significant increase of DTnet and DTpost.
Keywords: needle technique, psoas muscle, skin temperature
INTRODUCTION
Lumbar sympathetic ganglion block (LSGB) is a commonly performed procedure in the diagnosis and treatment of various pain states including complex regional pain syndrome, frost bite, peripheral vascular disease, acute herpes zoster and cancer pain which are thought to have sympathetic component in pain generation [1,2].
In clinical practice, psoas muscle injection of contrast occurs frequently, although the needle position is considered as appropriate for LSGB in anteroposterior and lateral projection view of fluoroscope. If we perform chemical or radiofrequency neurolysis in such cases, genitofemoral neuralgia can be caused and the effect of sympathetic block can be incomplete [3]. Moreover, in cases of diagnostic LSGB, the interpretation of treatment result can be obscure because of the unwanted somatic block. However, the actual incidence of injection into the psoas muscle during LSGB is not known.
In order to obtain a profound and complete sympatholytic effect, performing multi-level LSGB than single level LSGB seems more beneficial because of the variations of lumbar sympathetic ganglia. The lumbar sympathetic ganglia are variable in numbers, sizes and location. In most cases, three or four ganglia are found and there tends to be fusion of L1 and L2 ganglia in most patients [4-6]. In spite of the expected benefits of multilevel approach, the approach method is different from center to center, and there are few studies comparing these two methods.
When we determine the effect of sympathetic block, observing the successful contrast spread pattern of LSGB is not enough, essentially subjective and objective method should be followed to assess the degree of sympathetic block. Subjective measures include pain relief, warmth, changes in skin color, and anhidrosis. Objective tests include measurements of skin temperature (Ts) and blood flow, provocative sweat tests, and sympathetic skin response tests [7,8]. In this study, we compared the effect of sympathetic block between these two methods by the changes of Ts.
We performed this prospective study to identify the incidence of psoas injection of contrast during LSGB at L2, L3, and L4 and to compare the single needle technique versus multiple needle technique.
MATERIALS AND METHODS
This study was approved by the institutional review board and hospital ethics committee. Written informed consent was obtained from each patient prior to the LSGB procedure. For the evaluation of the psoas muscle injection, 216 injections of 83 consecutive patients who were scheduled to undergo fluoroscopically guided LSGB were enrolled. Among 83 patients, 58 patients were reevaluated for the changes of Ts. The other 25 patients were excluded because they showed psoas muscle injection in spite of repeated needle repositioning. They were divided into group A (n = 27, multiple needle technique) and group B (n = 31, single needle technique) and they were monitored the Ts for 30 minutes. In this study, the inclusion criteria of this study was patients who had radicular pain caused by spinal stenosis, herniated nucleus pulposus, internal disc disruption and failed back surgery syndrome. Patients who had known allergies to contrast media or local anesthetics, or who had coagulopathy were excluded. All procedures were performed by one of the authors under the fluoroscopic guidance.
All lumbar sympathetic blocks were performed under fluoroscopic guidance using a unilateral three needle technique in group A and single needle technique in group B. Patients were placed in the left or right lateral position on the fluoroscopic table depending on which leg was painful, and their backs were draped using a sterile technique. In group A, the second, third and fourth lumbar vertebras were identified by the biplanar fluoroscopy and their spinous process was marked. Three skin wheals were made with 1% lidocaine at 6 to 7 cm lateral from the lower margin of the L2, L3 and L4 spinous process. In group B, all LSGBs were performed at L2 level with the same method of group A. Five inches and 22-gauge block needles were used to perform this sympathetic block. We targeted the anterolateral margin of the vertebral body by the anteroposterior and lateral fluoroscopic view. Before we insert the needle, 1 µg of fentanyl was injected by the intravenous route to decrease the procedure pain. The needles were advanced slowly in order, guided by a lateral fluoroscopic view. After bony contact was made at about a depth of 2 inches, the block needle was withdrawn into the subcutaneous tissue and redirected at a slightly steeper angle and was then walked off the anterolateal margin of the vertebral body. Confirmation of the final needle position was accomplished using the anteroposterior and lateral views.
To evaluate the incidence of psoas muscle injection (Fig. 1), 2 ml of contrast (Iopamidol®, 300 mgI/ml; Bracco s.p.a., Milan, Italy) was injected after negative aspiration for blood and cerebrospinal fluid. Two ml of contrast was injected at each three vertebral level, totally 6 ml in group A, and 2 ml of contrast at one vertebral level in group B. The number of psoas injection of contrast was counted as L2, L3, and L4 in all patients. We recorded that the psoas muscle appearance was observed at the L2, L3 or L4.
Fig. 1.
Anteroposterior fluoroscopic view. Psoas muscle injections of contrast are shown (black arrows) during lumbar sympathetic ganglion block.
To determine the longitudinal constrast spread level, we injected the mixture of ropivacaine 0.75% 5 ml and contrast agent 5 ml. In group A, the mixture of 3.3 ml was injected at each three level and in group B, the mixture 10 ml was injected at single level. The height of lumbar vertebral body was subdivided into 4 parts, as follows, upper, medium, lower lumbar body and lumbar intervertebral disc segment (Fig. 2). If the contrast was appeared from lumbar upper level to intervertebral disc, this was recorded as 4 segments of longitudinal spread.
Fig. 2.
Longitudinal contrast spread level between group A and B and demonstration of lumbar vertebral body as upper (U), middle (M), lower (L) and intervertebral disc (D) to assess the degree of longitudinal contrast spread.
Ambient temperature in the two groups was controlled to minimize the difference of Ts between groups. Changes in Ts (℃) were measured as an indicator of the efficacy of the sympathetic block. To measure the Ts, adhesive thermocouple probes (Hewlett Packard, M1205A, Germany) were tightly attatched to the plantar surface of the ipsilateral (painful side) great toe. We defined the preblock temperature value (Tpre) at least 10 minutes after attaching the thermocouples probes. Just after injecting the mixture of ropivacaine, Ts at the designated sites was measured for 30 minutes. The preblock temperature difference between the ipsilateral and contralateral great toes (DTpre, ℃), and the postblock temperature difference between ipsilateral and contralateral great toe (DTpost, ℃) were measured and calculated. DTnet was calculated as follows: DTnet = DTpost - DTpre.
Statistical analysis was performed using SPSS 14.0 and all results were presented as a mean ± the standard deviation (SD) or number of patients. P < 0.05 defined statistical significance. Normality tests were performed using Kolmogorov-Smirnov tests. Chi square test was used for comparing categorical variables and a logistic regression was performed to identify factors associated with the psoas injection.
Chi-square and independent T-test were used to compare the mean values of the two groups of demographic data. An independent T-test was used to compare the mean values of the Tpre, DTpre, DTpost, DTnet and mean segment.
RESULTS
LSGB was performed in 65 patients by a unilateral three-needle technique (L2, L3, and L4), and each patient received three consecutive successful LSGBs, therefore it was counted as 195 injections. In 18 patients, although they received the same unilateral three-needle technique, we could only get a successful sympathetic contrast shadow in one or two LSGBs in spite of needle repositioning; therefore, it was counted as 21 injections.
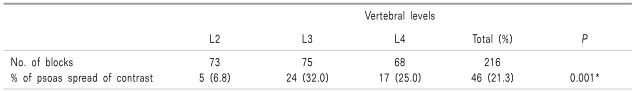
The overall incidence of psoas injection of contrast was 21.3% (46/216) and level of injection (categorized in L2, L3, and L4) showed significant correlation with the incidence of psoas injection of contrast, and L2 showed the lowest incidence (χ2 = 14.773, P = 0.001; Table 1).
Table 1.
The Incidence of Contrast Injection to Psoas Muscle During Lumbar Sympathetic Ganglion Block (LSGB)
Data are number (%) of injections. *χ2 test.
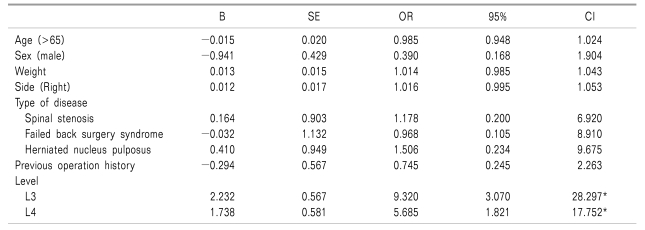
Age, sex, weight, side of injection, level and type of disease were analyzed as factors contributing to the psoas injection of contrast, and no factors except the level showed statistical significant correlation with the incidence of psoas injection of contrast (Table 2).
Table 2.
Factors Contributing to the Psoas Injection of Contrast During Lumbar Sympathetic Ganglion Block
*P < 0.001.
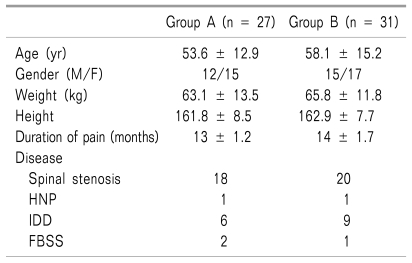
Among 83 patients, 58 patients were reevaluated for the changes of Ts and they were divided as group A and B. There were no significant differences in the patients' characteristics, duration of the disease and distribution of disease between two groups (Table 3).
Table 3.
Demographic Data
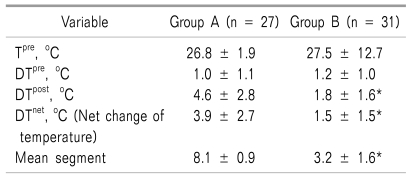
Tpre at the great toe was not significantly different between two groups (26.8 ± 1.9℃, 27.5 ± 2.7℃ for group A and B, Table 4). DTpost (4.6 ± 2.8℃, 1.8 ± 1.6℃, P < 0.001 for group A and B) and DTnet (3.9 ± 2.7℃, 1.5 ± 1.5℃, P < 0.001 for group A and B, Table 4) was significantly high in group A.
Table 4.
Cutaneous Temperature Changes and Segment of Longitudinal Contrast Spread
Tpre: preblock ipsilateral great toe temperature, DTpre: temperature difference between ipsilateral and contralateral great toe at preblock period, DTpre: temperature difference between ipsilateral and contralateral great toe at postblock period, DTnet: DTpost - DTpre.
*P < 0.001.
The mean segment of longitudinal contrast spread was 8.1 ± 0.9 for group A and 3.2 ± 1.6 for group B (P < 0.001, Table 4).
DISCUSSION
Multiple needle approach showed more significant increase of Ts (DTnet, DTpost) and LSGB at the L2 level showed the lowest incidence of psoas muscle injection of contrast. In this study, the overall incidence of psoas injection of contrast was 21.3%, and the level of injection showed statistical significant correlation. The L2 level showed the lowest incidence of psoas injection of contrast. Sayson et al. [9] evaluated the incidence of genitofemoral nerve block during LSGB and they reported that L2 level (0%) is less likely to be blocked than L4 (40%) level. Ranson et al. [10] investigated the cross sectional area of the paraspinal muscle on MRI, and reported that the cross sectional area of psoas muscle was smallest at L2 (9.75, left side) compared to L3 (16.26) or L4 (24.11) levels. We supposed that the smallest cross sectional area of psoas muscle at L2 level compared to the lower lumbar levels might be related to the lowest incidence of psoas injection of contrast in this study. If LSGB fails due to the psoas muscle injection in spite of repeated needle repositioning, L2 level should be considered to increase the success rate.
We could achieve significant vertical spread of contrast with the more significant increase of DTnet and DTpost in group A compared to group B. Lumbar sympathetic ganglion has the variations of the size, number and location [4-6]. This is true not only among cadavers but also on opposite sides of the same cadaver [5]. We supposed that multi-level LSGB would have more profound sympatholytic effect than single level because of greater vertical spread of contrast to the lumbar spine and more chances to meet sympathetic ganglion.
There is a tendency to perform a single level LSGB for the diagnostic purpose before radiofrequency ablation or chemical neurolysis. As our result shows that the sympatholytic effect of a single level LSGB is incomplete, therefore the interpretation of the treatment response can be limited. However, if we perform a multi-level LSGB irrespective of diagnostic or therapeutic purpose, several flaws are expected such as more prolonged procedure time and increased patient discomfort. In our pain clinic, we use small doses of fentanly (1 µg/kg) to reduce the procedure related pain. We think that these flaws do not outweigh the incomplete sympatholytic effect of a single level approach.
We could observe the most significant increases of Ts after LSGB at the great toe, and this result is in accordance with the study by Werdehausen et al. [11]. They concluded that the earliest and greatest rise of Ts occurred at the great toe (10.6 ± 0.4℃), became smaller proximally, and was negligible above the ankles, irrespective of the type and extent of block. Kim et al. [12] recommended the plantar surface of the feet as a site of temperature measurement because they showed the most significant change in temperature following a LSGB.
If we achieve the maximum change of Ts, it can promise the complete sympathectomy, and Stevens et al. [13] suggested that the maximum increase in Ts after the stellate ganglion block was predictive of a complete sympathectomy of the hand. Park et al. [14] concluded that the presence of the point of temperature change of 0.4℃ per minute would be used as an indicator of the onset of the successful LSGB without additional cost and time.
There are several limitations of our study. First, we observed the change of Ts only for 30 minutes, because of the circumstances of busy clinical practice. Second, to assess the efficacy of sympathetic block, we did not use other additional tools such as sweat test, laser dopler flowmetry, or thermography except monitoring of the Ts. To confirm the success of sympathetic block, monitoring of the multiple parameters would be more beneficial than a single paramenter.
In conclusion, LSGB performed at L2 level showed the lowest incidence of psoas muscle injection, and LSGB by multiple needle approach had a more significant increase of DTnet and DTpost.
References
- 1.de Oliveira R, dos Reis MP, Prado WA. The effects of early or late neurolytic sympathetic plexus block on the management of abdominal or pelvic cancer pain. Pain. 2004;110:400–408. doi: 10.1016/j.pain.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 2.Day M. Sympathetic blocks: the evidence. Pain Pract. 2008;8:98–109. doi: 10.1111/j.1533-2500.2008.00177.x. [DOI] [PubMed] [Google Scholar]
- 3.Kline MT, Yin W. Radiofrequency techniques in clinical practice. In: Waldman SD, editor. Interventional pain management. 2nd ed. Philadelphia: W.B. Saunders; 2001. pp. 243–293. [Google Scholar]
- 4.Datta S, Pai U. Paradiscal extraforaminal technique for lumbar sympathetic block: report of a proposed new technique utilizing a cadavar study. Pain Physician. 2004;7:53–57. [PubMed] [Google Scholar]
- 5.Rocco AG, Palombi D, Raeke D. Anatomy of the lumbar sympathetic chain. Reg Anesth. 1995;20:13–19. [PubMed] [Google Scholar]
- 6.Murata Y, Takahashi K, Yamagata M, Takahashi Y, Shimada Y, Moriya H. Variations in the number and position of human lumbar sympathetic ganglia and rami communicantes. Clin Anat. 2003;16:108–113. doi: 10.1002/ca.10069. [DOI] [PubMed] [Google Scholar]
- 7.Stevens RA, Stotz A, Kao TC, Powar M, Burgess S, Kleinman B. The relative increase in skin temperature after stellate ganglion block is predictive of a complete sympathectomy of the hand. Reg Anesth Pain Med. 1998;23:266–270. doi: 10.1016/s1098-7339(98)90053-0. [DOI] [PubMed] [Google Scholar]
- 8.Schmid MR, Kissling RO, Curt A, Jaschko G, Hodler J. Sympathetic skin response: Monitoring of CT-guided lumbar sympathetic blocks. Radiology. 2006;241:595–602. doi: 10.1148/radiol.2412051229. [DOI] [PubMed] [Google Scholar]
- 9.Sayson SC, Ramamurthy S, Hoffman J. Incidence of genitofemoral nerve block during lumbar sympathetic block: comparison of two lumbar injection sites. Reg Anesth. 1997;22:569–574. [PubMed] [Google Scholar]
- 10.Ranson CA, Burnett AF, Kerslake R, Batt ME, O'Sullivan PB. An investigation into the use of MR imaging to determine the functional cross sectional area of lumbar paraspinal muscles. Eur Spine J. 2006;15:764–773. doi: 10.1007/s00586-005-0909-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Werdehausen R, Braun S, Hermanns H, Freynhagen R, Lipfert P, Stevens MF. Uniform distribution of skin-temperature increase after different regional anesthesia techniques of the lower extremity. Reg Anesth Pain Med. 2007;32:73–78. doi: 10.1016/j.rapm.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Kim YC, Bahk JH, Lee SC, Lee YW. Infrared thermographic imaging in the assessment of successful block on lumbar sympathetic ganglion. Yonsei Med J. 2003;44:119–124. doi: 10.3349/ymj.2003.44.1.119. [DOI] [PubMed] [Google Scholar]
- 13.Stevens RA, Stotz A, Kao TC, Powar M, Burgess S, Kleinman B. The relative increase in skin temperature after stellate ganglion block is predictive of a complete sympathectomy of the hand. Reg Anesth Pain Med. 1998;23:266–270. doi: 10.1016/s1098-7339(98)90053-0. [DOI] [PubMed] [Google Scholar]
- 14.Park SY, Nahm SG, Kim YC, Lee SC. The cutoff rate of temperature to interpret the successful lumbar sympathetic block; The Korean Pain Society The forty nine Scientific Meeting; 2009. 11; Seoul. [Google Scholar]