Abstract
Purpose
We presented our initial clinical experiences with transumbilical laparoendoscopic single-site (LESS) ureterolithotomy for large, impacted ureteral stones.
Materials and Methods
Between March 2009 and November 2009, seven LESS ureterolithotomies were performed at our institute. During the operation, we made a single 2 cm incision at the umbilicus and a homemade port by using a small wound retractor (Alexis®, Applied Medical, Rancho Santa Margarita, USA), a surgical glove, and conventional trocars. The operation was performed in the same manner as conventional laparoscopic surgery. The mean maximal stone diameter was 21.9 mm (range, 16.0-27.0 mm). There were six cases of upper ureteral stones and one case of a mid-ureteral stone. Perioperative and postoperative parameters were evaluated.
Results
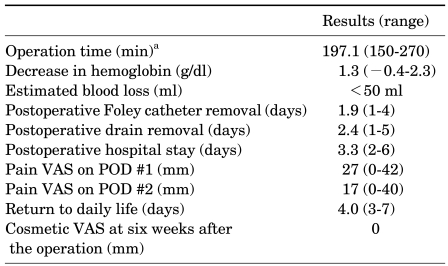
The mean operative time was 197.1 min (range, 150-270 min). No transfusions were required. The mean postoperative hospital stay was 3.3 days (range, 2-6 days). The mean pain intensity on a visual analogue scale (VAS) on postoperative day 2 was 26 mm (range, 0-80 mm), and the mean cosmetic VAS at 6 weeks after the operation was 0 mm. The mean time for patients to return to their baseline activities was 4.0 days (range, 3-7 days). In six cases, all stones were completely removed on the basis of postoperative radiologic evaluation. There were no cases of major complications, including internal organ injury, urinary leakage, or urinary tract infection.
Conclusions
Transumbilical LESS ureterolithotomy can be considered as an alternative treatment option with minimal invasiveness and good effectiveness for large, impacted ureteral stones.
Keywords: Instrumentation, Laparoscopy, Minimally invasive surgical procedures, Ureterolithiasis
INTRODUCTION
Although open ureterolithotomy for patients with proximal ureteral stones has a median stone-free rate of 97%, it has not been recommended as a first-line treatment because of longer hospitalization and greater postoperative morbidity [1]. However, the AUA/EAU Ureteral Stones Guideline Panel reported that laparoscopic or open ureterolithotomy as an alternative procedure might be desired as a primary or salvage therapy in very difficult situations such as cases with very large, impacted stones or multiple ureteral stones or in cases of concurrent conditions requiring surgery [2]. In these situations, laparoscopic ureterolithotomy is preferable to open surgical ureterolithotomy because of its decreased invasiveness [3,4].
Laparoscopic surgery has several advantages over open surgery, including decreased postoperative pain, improved cosmesis, and reduced hospital stay, and it is beginning to gain acceptance as a standard procedure for many intra-abdominal urology procedures [5-7]. Recently, efforts have been directed at further minimizing surgical morbidity and improving cosmetic outcomes with increasing experience in the laparoscopic environment. This has led to the development of techniques, multichannel single-port access, and novel articulating instruments that allow the laparoscopic procedure to be performed through a single skin incision within the umbilicus [8]. Laparoendoscopic single-site (LESS) surgery seeks to minimize patient discomfort, shorten convalescence, and improve cosmesis by placing all instruments through a readily concealed 2 cm incision [9].
In this study, we present our initial clinical experiences with seven patients who underwent transumbilical LESS ureterolithotomy for large, impacted ureteral stones.
MATERIALS AND METHODS
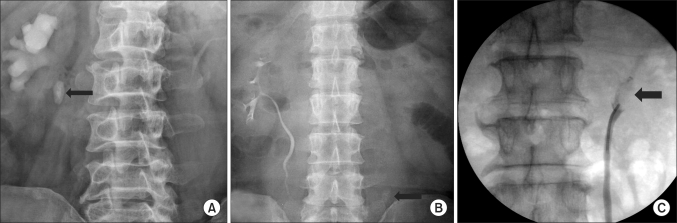
Between March 2009 and November 2009, we performed LESS ureterolithotomies in seven patients with upper (six cases) and middle (one case) ureteral stones. The indication was a large (>15 mm), impacted stone in the ureter. In our study, impaction was defined as hydroureteronephrosis above the calculus and a nonvisualized ureter below it on intravenous urogram (IVU) or the doctor's inability to pass a guidewire to the stone (Fig. 1) [10,11]. LESS ureterolithotomy was performed in patients who did not have critical ipsilateral renal impairment on the preoperative evaluation. Stones were on the right side in four cases and on the left side in three cases. The mean maximal stone diameter was 21.9 mm (range, 16.0-27.0 mm). Two patients had failed previous trials of extracorporeal shockwave lithotripsy (SWL), and another two patients had failed previous trials of retrograde ureteroscopic surgery. The baseline characteristics of all patients are summarized in Table 1.
FIG. 1.
Impacted ureteral stones (A, B). Hydroureteronephrosis above the calculus and a nonvisualized ureter below it are seen on IVU (C). A guidewire cannot be passed by the stone. Black arrow: impacted ureteral stone.
TABLE 1.
Demographic data of seven patients managed with LESS ureterolithotomy
LESS: laparoendoscopic single-site, M: male, URS: ureteroscopy, ESWL: extracorporeal shockwave lithotripsy
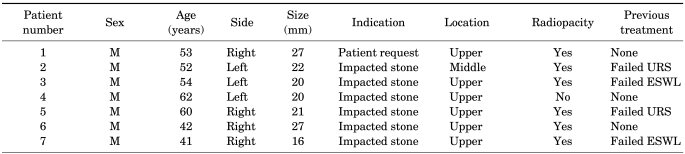
A homemade multi-channel port using a small wound retractor (Alexis®, Applied Medical, Rancho Santa Margarita, USA), a surgical glove, and conventional trocars [12] was used in all cases. We made a single 2 cm incision at the umbilicus, and a 2 to 3 cm rectus fasciotomy was made to enter the peritoneal cavity. The homemade multi-channel port was placed into the abdominal cavity, and the abdomen was insufflated to 15 mmHg (Fig. 2). We routinely used a rigid 30-degree, 10 mm laparoscope; articulating laparoscopic instruments, including a dissector, monopolar hook, scissors, and needle holder (Autonomy Laparo-angle™, Cambridge Endo, Framingham, USA); and standard straight working instruments. The right and left instruments were used cross-wise to each other to facilitate the intraperitoneal triangulation within the abdominal cavity. In four cases, an additional 2 mm needle trocar was used at the subcostal margin.
FIG. 2.
Homemade multichannel port using a small wound retractor (Alexis®, Applied Medical, Rancho Santa Margarita, USA), a surgical glove, and conventional trocars (12 mm, 12 mm, 5 mm).
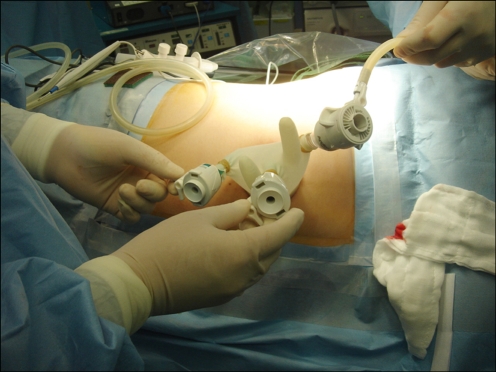
The operation was performed in the same manner as standard conventional laparoscopic surgery. With intraperitoneal access, the colon was mobilized medially, so that the ureter could be dissected and traced to the site of the stone. Because of the large size of the stone, it could be easily identified with proximal hydronephrosis and a hard tactile sensation at the level of the ureter. A longitudinal incision was made in the ureter over the calculus, which was removed by using straight or articulating forceps (Fig. 3). A double-pigtail ureteral stent was inserted in an anterograde fashion in two cases. In those cases, an additional set of 2 mm trocars was used. A 0.038 inch radiofocus guidewire (Termo®, Tokyo, Japan) was advanced through the 2 mm trocar and inserted into the bladder through the ureterotomy. And then, a double-pigtail ureteral stent was advanced in an anterograde fashion over the guidewire. In five cases, a double-pigtail ureteral stent was inserted in a retrograde fashion before the operation. The ureter was closed with 4-0 Vicryl by a full layer of four or six interrupted sutures in all cases. In six patients, surgical glue (Tisseel ®) or Surgicel® was applied over the ureterotomy suture site.
FIG. 3.
Ureteral stone removal using straight or articulating grasping forceps via an ureteral incision site.
One patient had one concomitant lower calyceal stone, and laparoscopic-guided flexible ureterorenoscopic extraction of the calyceal stone was simultaneously carried out. In this case, a flexible ureterorenoscope was inserted through the incision of the ureter to the calyces. Another patient had contralateral ureteral and renal stones that were removed together by flexible ureteroscopy before LESS ureterolithotomy. Postoperatively, all patients received patient-controlled analgesia. Follow-up was done with plain radiography (KUB) or noncontrast computed tomography at 1 day postoperatively and with KUB at 3 months postoperatively. Double-pigtail ureteral stents were routinely removed in the outpatient clinic approximately 6 weeks postoperatively. In one case of our series, the stent was removed 4 weeks after the surgery as the result of severe irritation symptoms. All patients were followed up by IVU 1 or 2 weeks after the ureteral stent removal.
Perioperative parameters including operative time, postoperative hemoglobin change, hospital stay, pain intensity on a visual analogue scale (VAS), cosmetic outcome on a VAS, time to return to full baseline activity, and complications were evaluated.
The VAS for cosmetic outcome consisted of a 100 mm horizontal line on a card with the words "completely satisfied" and "completely unsatisfied" placed at the left- and right-hand extremes of the line, respectively. The patients were instructed to mark the line at a point representing their cosmetic satisfaction 6 weeks after the operation.
To evaluate the 'Time to return to full baseline activities,' patients were asked to answer the question, "How long was it before you returned to daily activities for which you are normally independent?".
RESULTS
The procedure was successfully completed in all cases, with no conversions to standard multiport laparoscopic surgery or open surgery. All cases were performed in men, and their mean age was 56.2 years (range, 52-62 years). The mean operative time was 197.1 minutes (range, 150-270 minutes). Blood loss was estimated at less than 50 ml in all cases, and the decrease in serum hemoglobin was 1.3 g/dl (range, -0.4-2.3 g/dl). No transfusions were required. Oral feedings were started the next morning. All patients were ambulatory on the first postoperative day with minimal pain. The mean postoperative hospital stay was 3.3 days (range, 2-6 days). The mean pain intensities, as measured with a 100 mm VAS on postoperative days 1 and 2, were 27 mm (range, 0-42 mm) and 17 mm (range, 0-40 mm), respectively. The mean cosmetic 100 mm VAS at 6 weeks after the operation was 0 mm. The mean time to removal of the Foley catheter was 1.9 days (range, 1-4 days). Drains were inserted in five patients and were removed after a mean of 2.4 days (range, 1-5 days). The time to return to full baseline activities was 4.0 days (range, 3-7 days) (Table 2). There were no cases of operation-related complications such as internal organ injury, transfusion, urinary leakage, urinary tract infection, or ureteral stricture.
TABLE 2.
Perioperative data of LESS ureterolithotomy
LESS: laparoendoscopic single-site, VAS: visual analogue scale, POD: postoperative day, a: only LESS ureterolithotomy (five cases) 178 min, LESS ureterolithotomy with simultaneously ipsilateral lower calyceal stone removal (one case) 220 min, LESS ureterolithotomy with simultaneous contralateral ureteral and renal stone removal prior to LESS surgery (one case) 270 min
The stones were removed in all except one patient. In one patient, clinically insignificant fragments (<4 mm) migrated to the kidney and were spontaneously passed during the follow-up period.
All patients were asymptomatic and without obstructions or stricture formations upon postoperative follow-up, which included plain KUB films and IVU. There were no deteriorations in renal function.
DISCUSSION
The surgical management of urinary stone disease has dramatically changed since the introduction and development of percutaneous renal surgery and as a result of significant achievements in SWL, refinements in ureteroscopy, and technical advancements in the available modalities of intracorporeal lithotripsy [13].
At present, SWL and ureteroscopic lithotripsy are two highly effective common treatments for ureteral calculi [14]. Generally, SWL, either in situ or after pushback, is recommended as a first-line treatment for stones in the proximal ureter that are smaller than 1 cm. For stones larger than 1 cm in diameter, SWL, retrograde ureteroscopy, and percutaneous antegrade ureteroscopy are all acceptable choices. However, there are still difficult, large upper ureteral stones that are poorly treated by SWL or ureteroscopy alone. In this study, we assessed the feasibility, success rate, and safety of LESS ureterolithotomy to treat large, impacted upper ureteral stones, which are associated with lower success rates when treated by SWL or ureteroscopy alone.
The definition of an impacted ureteral calculus differs in several literature sources. Sinha et al used a definition of hydroureteronephrosis above the calculus and a nonvisualized ureter below it on IVU or no changes in the location of the calculus on serial plain abdominal radiographies [15]. Roberts et al defined impaction as ureteral calculi remaining unchanged in their location for at least two months, and Mugiya et al defined it as calculi causing a ureteral obstruction and not moving in response to manipulations such as ureteral catheterization [16,17]. In our study, impaction was defined as hydroureteronephrosis above the calculus and a nonvisualized ureter below it on IVU or the doctor's inability to pass a guidewire along the stone.
The 2007 AUA/EAU Ureteral Stones Guideline Panel reported that percutaneous antegrade ureteroscopy is an acceptable first-line treatment in select cases with large, impacted stones in the upper ureter; in combination with renal stone removal or in cases of ureteral stones after urinary diversion; or in select cases resulting from failure of retrograde ureteral access to large, impacted upper ureteral stones [2]. However, percutaneous antegrade ureteroscopy has a relatively high morbidity with a potentially large degree of bleeding despite its high stone-free rate because it requires access through the renal parenchyma [18].
The Guideline Panel also reported that laparoscopic or open surgical stone removal may be considered in rare cases in which SWL, ureteroscopy, or percutaneous ureteroscopy have failed or are unlikely to be successful [2]. Difficult ureteral calculi that are poorly treated by SWL, ureteroscopy, and percutaneous antegrade ureteroscopy, such as large stones, impacted stones, and hard stones, particularly those situated in the upper ureter or over the pelvic brim, can still be managed by open or laparoscopic surgeries [19].
Since the first transperitoneal and retroperitoneal laparoscopic ureterolithotomies were described in 1992 [20,21], laparoscopic procedures have been explored as options to replace open ureterolithotomy for ureteral stone disease due to the minimal invasiveness of the laparoscopic technique. Many series of laparoscopic ureterolithotomy have been reported with satisfactory outcomes [3,4,22,23]. Recently, efforts have been directed at further minimizing surgical morbidity and improving cosmetic outcomes with increasing experience in the laparoscopic environment. With the development of techniques, multichannel single port access, and novel articulating instruments, the laparoscopic procedure has been performed through a single skin incision. Several authors have reported their initial experiences with the single-port approach and the safety, effectiveness, and superior pain profile of this procedure in urology [24-26]. Rane and Rao reported on single-port-access laparoscopic ureterolithotomy in one patient in whom an R-port (Advanced Surgical Concepts, Wicklow, Ireland) was placed in the umbilicus to manage an impacted 2.5 cm stone in the upper ureter and suggested that single-port-access laparoscopic ureterolithotomy can be performed safely with fewer ports [27].
We also successfully performed LESS ureterolithotomies in seven patients with impacted ureteral stones. Each intraoperative procedure was accomplished with results similar to those of standard conventional multi-port laparoscopic ureterolithotomy. Compared with conventional laparoscopic surgery, LESS surgery has a unique learning curve, principally because of the difficulty in navigating the instruments within a limited range of motion and the need for significant coordination between the surgeon and the camera holder. Because all of the instruments are closely packed together, clashing of instruments and the laparoscope is common. We crossed the right and the left curved or straight instruments over each other to facilitate the intraperitoneal triangulation within the abdominal cavity, thus decreasing the range of motion. We had already experienced LESS surgery in more than 20 cases before beginning LESS ureterolithotomy, and we experienced no technical difficulties in performing LESS ureterolithotomies. The ureterotomy was usually closed with a straight needle holder by use of an intracorporeal suture. Otherwise, the articulating needle holder was used to make a proper suture line. Also, selective use of a 2 mm Verress needlescopic port and subsequently inserting a 1.9 mm needlescopic grasper facilitated the instruments' triangulation. This 2 mm port was inserted via a skin puncture without any formal skin incision at the subcostal margin, did not require formal closure, and was associated with negligible scarring or pain [28].
In two cases, simultaneous operations were performed. In comparison with several previous conventional laparoscopic ureterolithotomies [19,22,23], our LESS ureterolithotomy had a longer mean operation time that that of conventional laparoscopic surgeries from the published literature (60-160 min vs. 197.1 min). However, except for the two cases that included the simultaneous removal of stones from other sites, the mean operative time was 178 min.
Our data demonstrated that LESS ureterolithotomy can be considered as a good option for the treatment of large, impacted ureteral stones. In all cases, the stones were effectively managed with minimal morbidities, short convalescences, and excellent cosmetic outcomes. Umbilical scars were actually nonvisible in all patients (Fig. 4).
FIG. 4.
Six-week postoperative external image of an umbilical wound in a patient who underwent LESS ureterolithotomy.
There are several limitations of this study. First, the study described observational outcomes only, and therefore the results should not be considered to establish the superiority of LESS ureterolithotomy over open surgery or standard conventional laparoscopic surgery, although several published series have described recovery, pain, and cosmetic benefits with the single-port approach [29,30]. Additional comparisons between LESS ureterolithotomy and conventional laparoscopic or open ureterolithotomy for impacted stones are warranted. Second, the number of patients in this study was small and follow-up was short. Only seven cases and 3 months of follow-up were included in this study. Certainly, a larger study and longer follow-up are warranted to further characterize the role of this less-invasive operation. Third, although we used a 100 mm VAS to evaluate cosmetic satisfaction, this questionnaire has not yet been validated. However, all patients reported that they were 'completely satisfied (VAS 0 mm)' with the cosmetic results, and the cosmetic outcomes of LESS ureterolithotomy seem to be excellent.
CONCLUSIONS
Transumbilical LESS ureterolithotomy can be performed safely with good surgical outcomes in selected patients with large, impacted ureteral stones. Outcomes in limited cases in the short term appear comparable with those of conventional laparoscopic ureterolithotomy, as reported in published data.
Transumbilical LESS ureterolithotomy can be considered as an alternative treatment option with minimal invasiveness and good effectiveness in patients with large, impacted ureteral stones before open ureterolithotomy and for ureteral stones after failed SWL or ureteroscopy.
Prospective studies comparing the outcomes of LESS ureterolithotomy with those of standard laparoscopic ureterolithotomy are needed to further define the role and the potential advantages of this approach.
Footnotes
The authors have nothing to disclose.
References
- 1.Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. The American Urological Association. J Urol. 1997;158:1915–1921. doi: 10.1016/s0022-5347(01)64173-9. [DOI] [PubMed] [Google Scholar]
- 2.Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, et al. 2007 guideline for the management of ureteral calculi. J Urol. 2007;178:2418–2434. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 3.Skrepetis K, Doumas K, Siafakas I, Lykourinas M. Laparoscopic versus open ureterolithotomy. A comparative study. Eur Urol. 2001;40:32–36. doi: 10.1159/000049746. [DOI] [PubMed] [Google Scholar]
- 4.Goel A, Hemal AK. Upper and mid-ureteric stones: a prospective unrandomized comparison of retroperitoneoscopic and open ureterolithotomy. BJU Int. 2001;88:679–682. doi: 10.1046/j.1464-4096.2001.00150.x. [DOI] [PubMed] [Google Scholar]
- 5.Clayman RV, Kavoussi LR, Figenshau RS, Chandhoke PS, Albala DM. Laparoscopic nephroureterectomy: initial clinical case report. J Laparoendosc Surg. 1991;1:343–349. doi: 10.1089/lps.1991.1.343. [DOI] [PubMed] [Google Scholar]
- 6.Gill IS, Clayman RV, McDougall EM. Advances in urological laparoscopy. J Urol. 1995;154:1275–1294. [PubMed] [Google Scholar]
- 7.Kim HH. Laparoscopic surgery in urology (I) Korean J Urol. 2003;44:945–958. [Google Scholar]
- 8.Desai MM, Berger AK, Brandina R, Aron M, Irwin BH, Canes D, et al. Laparoendoscopic single-site surgery: initial hundred patients. Urology. 2009;74:805–812. doi: 10.1016/j.urology.2009.02.083. [DOI] [PubMed] [Google Scholar]
- 9.White WM, Haber GP, Goel RK, Crouzet S, Stein RJ, Kaouk JH. Single-port urological surgery: single-center experience with the first 100 cases. Urology. 2009;74:801–804. doi: 10.1016/j.urology.2009.04.030. [DOI] [PubMed] [Google Scholar]
- 10.Ziaee SA, Basiri A, Nadjafi-Semnani M, Zand S, Iranpour A. Extracorporeal shock wave lithotripsy and transureteral lithotripsy in the treatment of impacted lower ureteral calculi. Urol J. 2006;3:75–78. [PubMed] [Google Scholar]
- 11.Morgentaler A, Bridge SS, Dretler SP. Management of the impacted ureteral calculus. J Urol. 1990;143:263–266. doi: 10.1016/s0022-5347(17)39928-7. [DOI] [PubMed] [Google Scholar]
- 12.Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. Surg Endosc. 2009;23:1393–1397. doi: 10.1007/s00464-008-0252-y. [DOI] [PubMed] [Google Scholar]
- 13.Paik ML, Wainstein MA, Spirnak JP, Hampel N, Resnick MI. Current indications for open stone surgery in the treatment of renal and ureteral calculi. J Urol. 1998;159:374–378. doi: 10.1016/s0022-5347(01)63922-3. [DOI] [PubMed] [Google Scholar]
- 14.Dretler SP, Keating MA, Riley J. An algorithm for the management of ureteral calculi. J Urol. 1986;136:1190–1193. doi: 10.1016/s0022-5347(17)45279-7. [DOI] [PubMed] [Google Scholar]
- 15.Sinha M, Kekre NS, Chacko KN, Devasia A, Lionel G, Pandey AP, et al. Does failure to visualize the ureter distal to an impacted calculus constitute an impediment to successful lithotripsy? J Endourol. 2004;18:431–435. doi: 10.1089/0892779041271625. [DOI] [PubMed] [Google Scholar]
- 16.Roberts WW, Cadeddu JA, Micali S, Kavoussi LR, Moore RG. Ureteral stricture formation after removal of impacted calculi. J Urol. 1998;159:723–726. [PubMed] [Google Scholar]
- 17.Mugiya S, Nagata M, Un-No T, Takayama T, Suzuki K, Fujita K. Endoscopic management of impacted ureteral stones using a small caliber ureteroscope and a laser lithotriptor. J Urol. 2000;164:329–331. [PubMed] [Google Scholar]
- 18.Michel MS, Trojan L, Rassweiler JJ. Complications in percutaneous nephrolithotomy. Eur Urol. 2007;51:899–906. doi: 10.1016/j.eururo.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 19.El-Moula MG, Abdallah A, El-Anany F, Abdelsalam Y, Abolyosr A, Abdelhameed D, et al. Laparoscopic ureterolithotomy: our experience with 74 cases. Int J Urol. 2008;15:593–597. doi: 10.1111/j.1442-2042.2008.02065.x. [DOI] [PubMed] [Google Scholar]
- 20.Raboy A, Ferzli GS, Ioffreda R, Albert PS. Laparoscopic ureterolithotomy. Urology. 1992;39:223–225. doi: 10.1016/0090-4295(92)90294-7. [DOI] [PubMed] [Google Scholar]
- 21.Gaur DD. Laparoscopic operative retroperitoneoscopy: use of a new device. J Urol. 1992;148:1137–1139. doi: 10.1016/s0022-5347(17)36842-8. [DOI] [PubMed] [Google Scholar]
- 22.Jeong BC, Park HK, Byeon SS, Kim HH. Retroperitoneal laparoscopic ureterolithotomy for upper ureter stones. J Korean Med Sci. 2006;21:441–444. doi: 10.3346/jkms.2006.21.3.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nouira Y, Kallel Y, Binous MY, Dahmoul H, Horchani A. Laparoscopic retroperitoneal ureterolithotomy: initial experience and review of literature. J Endourol. 2004;18:557–561. doi: 10.1089/end.2004.18.557. [DOI] [PubMed] [Google Scholar]
- 24.Kaouk JH, Haber GP, Goel RK, Desai MM, Aron M, Rackley RR, et al. Single-port laparoscopic surgery in urology: initial experience. Urology. 2008;71:3–6. doi: 10.1016/j.urology.2007.11.034. [DOI] [PubMed] [Google Scholar]
- 25.Raman JD, Cadeddu JA, Rao P, Rane A. Single-incision laparoscopic surgery: initial urological experience and comparison with natural-orifice transluminal endoscopic surgery. BJU Int. 2008;101:1493–1496. doi: 10.1111/j.1464-410X.2008.07586.x. [DOI] [PubMed] [Google Scholar]
- 26.Jeong W, Jeon HG, Yu HS, Kim KH, Yang SC, Rha KH, et al. Embryonic-natural orifice transluminal endoscopic surgery nephrectomy. Korean J Urol. 2009;50:609–612. [Google Scholar]
- 27.Rane A, Rao P, Rao P. Single-port-access nephrectomy and other laparoscopic urologic procedures using a novel laparoscopic port (R-port) Urology. 2008;72:260–263. doi: 10.1016/j.urology.2008.01.078. [DOI] [PubMed] [Google Scholar]
- 28.Soble JJ, Gill IS. Needlescopic urology: incorporating 2-mm instruments in laparoscopic surgery. Urology. 1998;52:187–194. doi: 10.1016/s0090-4295(98)00234-9. [DOI] [PubMed] [Google Scholar]
- 29.White WM, Goel RK, Kaouk JH. Single-port laparoscopic retroperitoneal surgery: initial operative experience and comparative outcomes. Urology. 2009;73:1279–1282. doi: 10.1016/j.urology.2009.01.051. [DOI] [PubMed] [Google Scholar]
- 30.Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009;55:1198–1204. doi: 10.1016/j.eururo.2008.08.019. [DOI] [PubMed] [Google Scholar]