Abstract
Many studies have attempted to better elucidate the effect of foot orthoses on gait dynamics. To our knowledge, most previous studies exclude the first few steps of gait and begin analysis at steady-state walking. These unanalyzed steps of gait may contain important information about the dynamic and complex processes required to achieve equilibrium for a given gait velocity. The purpose of this study was to quantify gait initiation and determine how many steps were required to reach steady state walking under three footwear conditions: barefoot, habitual shoes, and habitual shoes with a prefabricated foot orthoses. Fifteen healthy subjects walked 50 meters at habitual speed in each condition. Wearing habitual shoes with the prefabricated orthoses enabled subjects to reach steady state walking in fewer steps (3.5 steps ± 2.0) compared to the barefoot condition (5.2 steps ± 3.0; p=0.02) as well as compared to the habitual shoes condition (4.7 steps ± 1.6; p=0.05). Interestingly, the subjects’ dynamic medial-lateral balance was significantly improved (22%, p<0.05) by using foot orthoses compared to other footwear conditions. These findings suggest that foot orthoses may help individuals reach steady state more quickly and with a better dynamic balance in the medial-lateral direction, independent of foot type. The findings of this pilot study may open new avenues for objectively assessing the impact of prescription footwear on dynamic balance and spatio-temporal parameters of gait. Further work to better assess the impact of foot orthoses on gait initiation in patients suffering from gait and instability pathologies may be warranted.
Keywords: gait, orthotic devices, outcome assessment (health care)
1. Introduction
The gait initiation phase is the transient period between upright posture and steady state gait[1]. Walking at a constant mean velocity is considered ‘steady-state’ activity where the body is neither accelerating nor decelerating (i.e. relatively low inter-cycle speed variability). Various aspects of steady-state walking have been analyzed extensively in an attempt to better understand both healthy and pathological gait[2, 3]. However, limited focus has been placed on the other two components of human locomotion: gait initiation and stopping. The dynamic processes of gait initiation and stopping are much more complex since the human body needs to accelerate and decelerate, respectively, often in a limited amount of time. As a result, the skills necessary to maintain stability, weight transfer, foot clearance, etc., become more critical during these transition phases than during the steady-state conditions[1, 4–6]. Such requirements become even more significant in patients with neurological disorders, lower limb complications, and in older adults, where there are inherent difficulties with postural stability and gait[1, 7, 8].
Both sensory input and muscular actions are necessary to create the postural and dynamic conditions for progression and reaching a given gait velocity. Recently, it has been suggested that foot orthoses may act as proprioceptive stimulators or gait perturbation devices[9, 10]. This theory has lead to preliminary investigation into the role of foot orthoses in postural control and balance[11–13]. Despite the fact that an appropriate equilibrium is of key importance in a faster gait initiation, little attention has been paid to examining the impact of using foot orthoses to improve gait initiation.
One of the major obstacles in assessing the impact of foot orthoses on gait initiation is measuring natural locomotion. In the gait lab, there are apparatus limitations, subject targeting, and subsequent methodological issues that constrain this assessment. Camera-based motion analysis systems [14–17] demonstrate high accuracy for assessing locomotion, but the number of consecutive strides that can be measured is limited. Instrumented treadmills are also not well suited for this purpose due to the constraints on the base of gait as well as the frictional and inertial changes they impart on the gait initiation process. Instrumented mats also have length limitations that make it difficult to accurately identify the acceleration and deceleration phases of walking. A larger number of consecutive strides should be measured to assess inter-cycle gait speed variability, an important variable for reaching steady state walking. Motion capture with body-worn sensors offers an appropriate alternative for assessing human locomotion continuously over long periods of time outside of a gait laboratory and in a free condition [15, 16]. A range of body-attached sensors including electromechanical switches, goniometers, accelerometers, gyroscopes, pedometers, and actometers, have been used in several clinical studies to capture and analyze human movement performance in free-living conditions[15, 17–19].
In a recent work[16], we found that when laboratory constraints are removed, subjects frequently change their walking patterns. In this prior study, elderly subjects were found to walk significantly faster outdoors despite excellent test-retest reliability (ICC>0.9) for both measurements inside and outside a gait laboratory [16]. These results seem to indicate that at least some gait parameters assessed inside of a gait laboratory environment may not replicate the subject’s gait outdoors where they are most likely to wear their prescribed footwear.
The purpose of this new research was to assess spatio-temporal parameters of gait initiation outside of a gait laboratory. Our objective was twofold: 1) examine whether the type of footwear may impact the number of steps required to reach steady state walking, 2)assess the impact of foot orthoses on spatio-temporal parameters of gait during both steady state and gait initiation phases. It was hypothesized that foot orthoses may improve the dynamics necessary to induce the appropriate equilibrium for reaching a given gait velocity.
2. Method
2.1 Subjects
Eligible subjects were recruited from students and employees at the Rosalind Franklin University of Medicine and Science (North Chicago, IL, USA) by verbal communication. Interested individuals were scheduled a time to come to the Human Performance Laboratory, provide informed consent, and consequently participate in the trial. Fifteen healthy subjects (6 female, 9 male) were recruited with an average age 24.2 ±1.78 years, average height 173.77 ±14.02 cm, and average weight 76.44 ±17.5 kg. All subjects were naïve to the foot orthoses used in this study. The study received ethical approval in accordance with the local Institutional Review Board. All subjects provided informed consent prior to the start of testing. Subjects were excluded if they had active musculoskeletal conditions, pain, or fatigue.
2.2. Apparatus
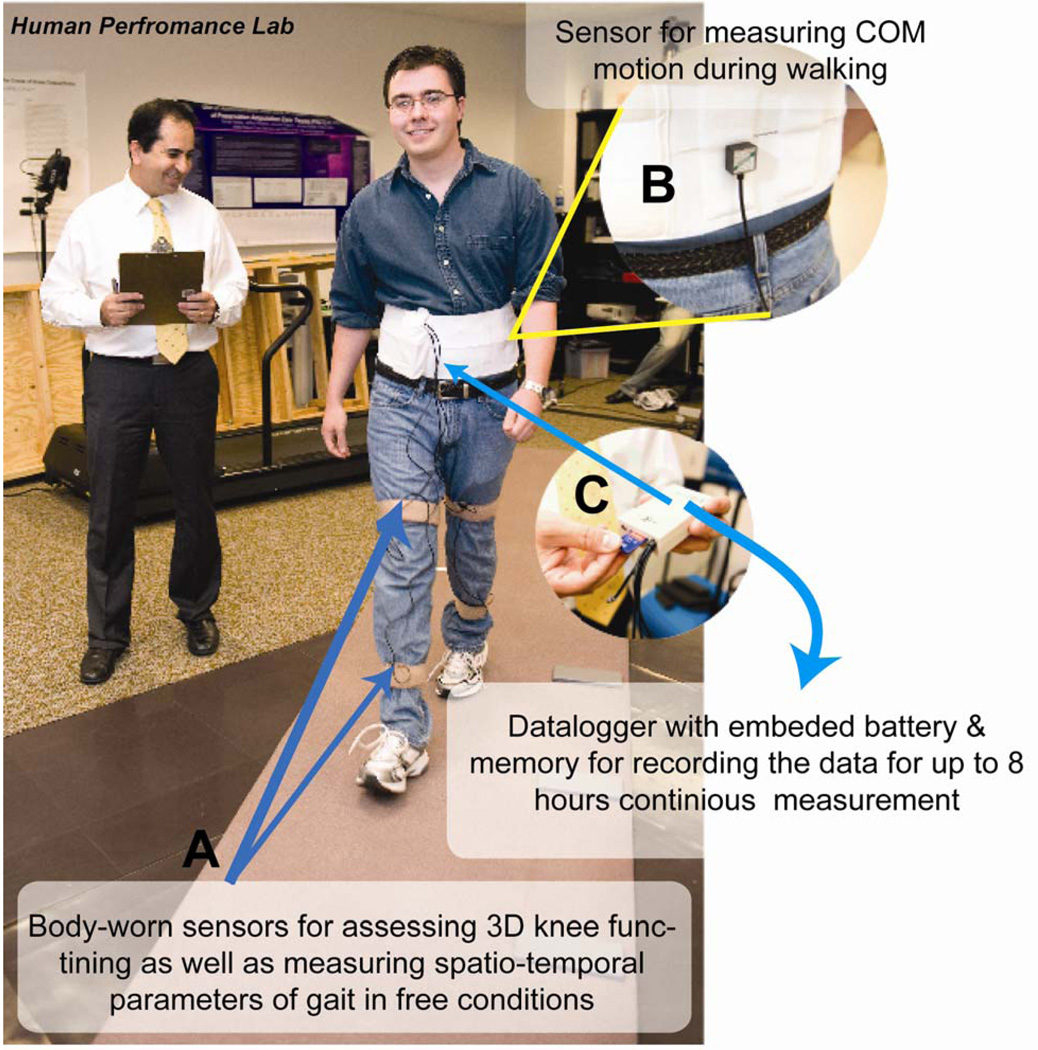
Gait analysis was performed using five miniature sensors attached to right and left anterior shins, right and left anterior thighs, and posteriorly to the lumbar region using elastic bands (Figure 1). The sensors attached to lower-limbs were a uniaxial gyroscope (ADXRS 250, Analog device) that allows measuring the angular velocity of the segment around the mediolateral axis (flexion-extension). The sensors attached to the lumbar region included a triaxial accelerometer and a triaxial gyroscope that permitted measuring the range of motion of center of mass (COM) for each gait stride in both the anterior-posterior and medial-lateral directions. Signals from sensors were digitized (16 bit) at a sampling rate of 200 Hz by a light portable data logger (Physilog®, BioAGM, CH) and stored for off-line analysis on a Secure Digital (SD) memory card (2Mb). The method for calculating spatio-temporal parameters of gait has been described in detail and validated in previous publications [2, 20]. To summarize, the gait phases are determined from the precise moments of heel-strike (initial foot contact) and toe-off (terminal foot contact). These moments are extracted from gyroscopes attached to each shank through a local minimal peak detection scheme [20]. Based on the subject’s height as well as using a biomechanical model, spatial parameters (i.e., lower limb stride length and stride velocity), can be estimated by integrating the angular rate of rotation of the thigh and shank [20]. Finally, to assess center of mass displacement during walking (e.g., medial-lateral & anterior-posterior rotation of center of mass per cycle), another sensor is attached to the lumbosacral region. This sensor provides range of motion estimates for center of mass for each cycle and therefore allows us to assess a subject’s postural control during gait [21].
Figure 1.
Physilog Gait Analysis device- For extracting spatio-temporal parameters of gait four sensors (uniaxial gyroscope) were attached to right and left anterior shins, right and left anterior thighs (Fig. 1A) and one sensor (combination of a triaxial accelerometer and a triaxial gyroscope) was attached posteriorly to the lumbar region using elastic bands (Fig. 1B). Signals from sensors were digitized (16 bit) at a sampling rate of 200 Hz by a light portable data logger (Physilog®, BioAGM, CH) and stored for off-line analysis on a SD memory card (Fig. 1C).
2.3 Subject Preparation & Protocol of Measurement
Subjects were tested in random order under the following footwear conditions: 1) barefoot, 2) habitual shoes, and 3) habitual shoes with Birkenstock Blue-Footbed prefabricated arch-support orthoses (Birkenstock USA, Navato, CA). The tests were conducted indoors in a well lit, level hallway with tile flooring. Subjects were instructed to walk at their habitual speed down the hallway and stop once they reached a predetermined stopping point of 50 meters. Subjects were then asked to turn around and return to the starting point, constituting the second trial. The first trial was considered a warm-up trial, and only the second trial was used for final analysis. Participants repeated the walking trials under each of the two remaining conditions. Equipment or sensors were not repositioned between trials.
2.4 Estimation of gait initiation and steady-state phases of gait
A previously defined algorithm[22] was used to identify the start of steady state walking and estimate the number of steps required to reach steady state gait. In summary, the standard deviation (SD) of velocity of six successive strides (six right and six left steps) was calculated from the first stride on (for example: SD of strides 1, 2, 3, 4, 5, 6 and 2, 3, 4, 5, 6, 7,…. and 15, 16, 17, 18, 19, 20). For example, by assuming the first left stride as initiating the gait, the vector of velocity (V) represents the first 20 alternating stride velocities if left and right foot was defined as:
with SV= stride velocity; L=left; R=right;
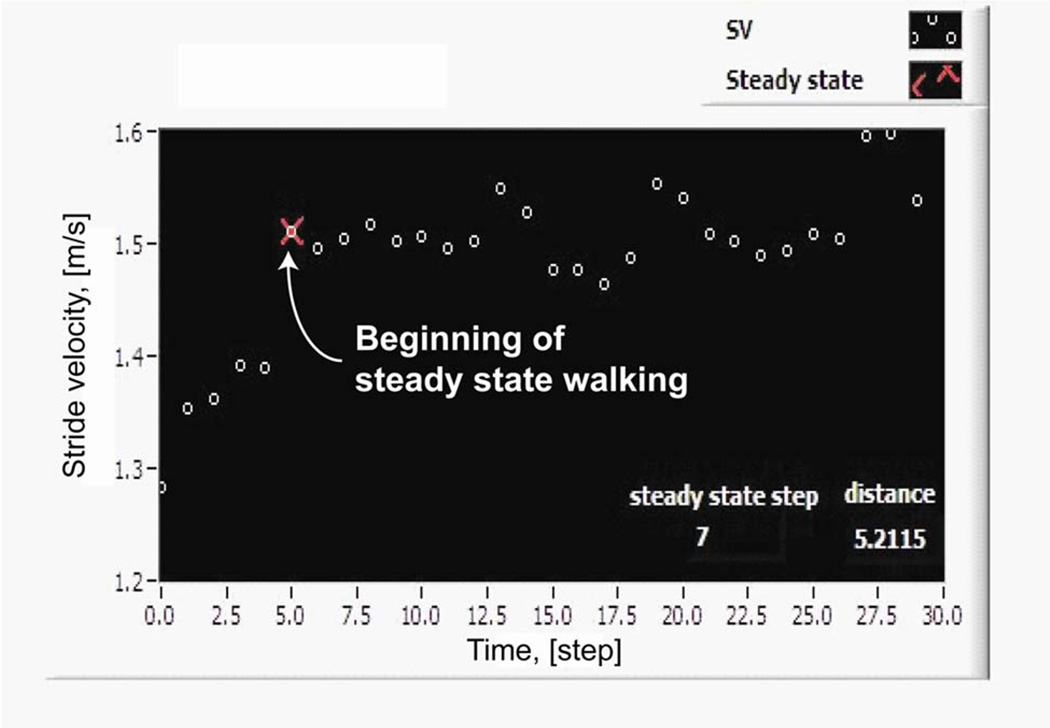
The marker of the beginning of steady state walking was the first stride of the group of six strides with a SD below the median SD of the first 40 strides (20 left and 20 right strides) ±6%. The rationale for this algorithm was that at least two strides (1 left plus 1 right) had to be observed to exclude a limping effect with increases or decreases in velocity. SD of gait speed was considered most appropriate as it represents steadiness of walking[22]. We considered that six consecutive strides instead of two, provides a more valid representation of steady state walking. The median SD of all strides instead of the mean SD was used as a reference in order to counteract possible outliers or possible decreases in velocity at the end of the observed gait cycles. Six percent tolerance was chosen arbitrarily and based on primary observation of the inter-participant variation around the steady state value[22]. A program based on LabVIEW (ver 8.5, NI, USA) was developed to identify and illustrate the beginning point of steady state according to the above algorithm and also to determine the number of steps and distance from gait start until steady state walking was achieved (Figure 2). The face validity of the algorithm was checked by comparing results with velocity/stride plots.
Figure 2.
Estimation of gait initiation – A graphical interface was designed using LabVIEW to visualize the beginning step of steady state walking based on statistical inter-cycle variability of gait speed over the first 20 cycles (40 steps).
2.5 Gait parameters
Physilog® provides a wide range of spatio-temporal parameters of gait, but in this study, we investigated only the mean of gait cycle time (GCT), stride velocity (SV), double support time (DS), the range of COM motion in medial-lateral (COMML) and anterior-posterior (COMAP) directions, as well as their inter-cycle variability expressed by their coefficient of variation (CV). The CV was defined as: (standard deviation)/(mean value)×100. Mean and CV values were estimated prior to reaching steady-state gait and ten strides after reaching gait steady state. Additionally, the number of steps and the distance required to achieve steady state walking were estimated for each trial.
2.6 Statistical Analysis and Power Analysis
Comparisons across the three walking conditions for each walking task (type of footwear) were made using ANOVA and a Post Hoc test of Scheffe. Comparisons between each paired condition were made using a paired one-tailed Student’s t test. For all tests an alpha level of 0.05 was considered statistically significant. Pearson’s correlation coefficient was calculated for examining the correlation between gait speed and number of steps required to achieve steady state walking. All calculations were made using Matlab (MathWorks, Ver 7.4 (R2007a)).
3. Results
3.1 The impact of foot orthoses on gait initiation
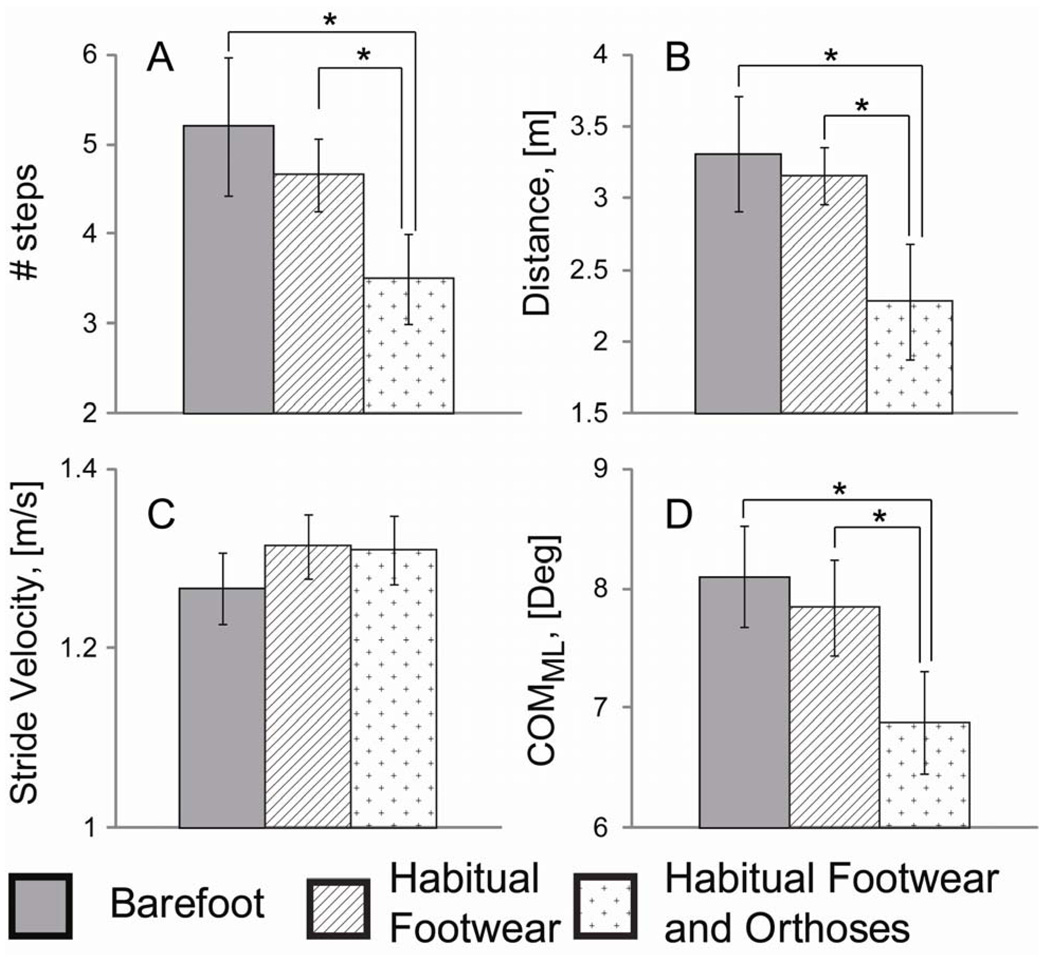
The results demonstrated that by wearing foot orthoses with their habitual footwear, subjects needed significantly fewer steps to reach steady state walking (Fig. 3A) compared to a barefoot condition (−49%, p<0.05) as well as compared to shod with their standard footwear alone (−34%, p<0.05). The average number of steps for reaching gait steady-state was 3.5±2.0 (95% CI =[1.25,8] steps, minimum = 1 step, maximum= 8 steps) wearing foot orthoses, and was increased to 4.66±1.58 (95% CI=[2.25,8.25] steps, minimum=2 steps, maximum= 8 steps) and 5.20±3.0 (95% CI=[1,10.75] steps, minimum=1 step, maximum=11 steps), respectively, for habitual footwear alone and barefoot trials(Table 1). A similar tendency was observed for the distance required to achieve steady state (Fig. 3B). The distance to reach steady state for the foot orthoses condition was on average 2.28±0.80 m (95%CI=[0.71,6.21], minimum=0.71 m, maximum=6.23 m) and was increased by 38% (p<0.05) in the habitual footwear alone (average 3.16 m ±0.91, 95%CI=[1.36 4.49], minimum=1.14 m, maximum=4.52 m) and by 45% (p<0.05) in the barefoot condition (average 3.31 m ±0.98, 95%CI=[0,7.2], minimum=0 m, maximum=7.30 m). Although the gait initiation was improved for habitual footwear alone compared to barefoot condition (12% reduction in the number of steps and 5% reduction in the distance required achieving steady state), the improvement was not significant.
Figure 3.
A) Number of steps required to reach steady state gait over each footwear condition; B) Walking distance required to achieve gait steady state over each footwear condition; C) Average of stride during steady state across three footwear conditions; The average of inter-cycle range of motion for COM in medial-lateral direction (COMML) across three footwear conditions. By using foot orthoses, gait initiation was improved by reducing the COMML, number of steps and walking distance required to reach steady state walking, compared to the shod only and barefoot conditions.
Table 1.
Spatio-temporal parameters of gait cross three different footwear conditions: 1) barefoot, 2) habitual footwear, 3) habitual footwear with Birkenstock Blue-Footbed prefabricated arch-support orthoses.
| Gait parameter | Barefoot Mean±SD |
Habitual Footwear Mean±SD |
Habitual Footwear and Orthoses Mean±SD |
|||
|---|---|---|---|---|---|---|
| Average | CV(%) | Average | CV(%) | Average | CV(%) | |
| Number of Step * | 5.20±3.0 | - | 4.66±1.58 | - | 3.50±2.0 | - |
| Distance**, [m] | 3.31±0.98 | - | 3.16±0.91 | - | 2.28±0.80 | - |
| Stride Velocity, [m/s] | 1.27±0.17 | 2.0±0.5 | 1.31±0.14 | 1.8±.5 | 1.31±0.15 | 1.9±0.6 |
| Gait Cycle Time, [s] | 1.01±0.07 | 1.4±0.6 | 1.07±0.08 | 1.1±0.4 | 1.06±0.07 | 1.2±0.4 |
| Double Support, [%] | 21.7±2.1 | 11.7±5.6 | 20.1±2.0 | 10.0±7.5 | 19.5±2.2 | 11.7±9.3 |
| COMAP, [Deg] | 5.22±3.2 | 14.0±4.6 | 5.08±2.1 | 13.3±6.7 | 5.66±3.4 | 14.9±6.0 |
| COMML, [Deg] | 7.62±1.9 | 10.4±3.9 | 7.63±1.8 | 8.7±3.7 | 6.22±1.6 | 9.6±4.6 |
Average of number of steps required to achieve steady state walking
Average of walking distance required to steady state walking
No correlation was found between the subject’s average speed and the number of steps required to reach steady state during any of the three footwear conditions (r=0.38, p=0.38 for barefoot; r=0.22, p=0.42 for habitual footwear; and r=0.23, p=0.40 for orthoses condition). Similarly, there was no observed correlation observed between the distance required to reach steady state and the subject’s gait speed (r=0.46, p=0.08 for barefoot; r=0.13, p=0.63 for habitual footwear; and r=0.29, p=0.30 for foot orthoses condition).
3.2 The impact of footwear condition on spatio-temporal parameters of gait
Table 1 summarizes the average and CV values for the selected spatio-temporal parameters of gait across the three footwear conditions. By using foot orthoses, despite of an increase on average by 5% (p<0.001, mean=+50ms, 95%CI=[25,56]ms) in gait cycle time, the gait speed was moderately increased on average by 3% (p=0.08, mean=+4cm/s, 95%CI=[−3,16]cm/s) compared to the barefoot condition (Fig. 3C). No significant difference was observed between habitual footwear with foot orthoses trials (p=0.89, mean=+0.7cm/s, 95%CI=[−10.4,11.8]cm/s). On the same note, double support time was significantly reduced on average by 11% (p<0.01, mean=−2.2%, 95%CI=[−3.77, −0.60]%) when subjects wore foot orthoses compared to the barefoot walking. But double support time remained the same between habitual footwear and foot orthoses trials (p=0.18). Interestingly, by using foot orthoses, the COMML was significantly reduced (Fig. 2D) on average by 22% (p<0.05, mean= −1.41 deg, 95%CI=[−3.58 −0.12] deg) and 23% (p<0.05, mean=−1.40deg, 95%CI=[−3.47 −0.01]deg), respectively, compared to habitual shoes and barefoot conditions for both gait initiation and steady state phases. However, no significant difference was observed for COMAP across footwear condition trials (p>0.1). We did not observe any significant difference for inter-cycle gait variability across all foot conditions and all estimated gait parameters (p>0.05).
4. Discussion
4.1. The impact of foot orthoses on gait initiation
We believe this study is the first quantification of gait initiation parameters across three footwear conditions. We found that wearing habitual shoes with prefabricated foot orthoses enabled subjects to reach steady state walking in 3.5 steps compared to 5.2 steps for the barefoot condition and 4.7 steps for the habitual shoes alone condition. These results put into context other studies that have described the minimum steps necessary to achieve stable estimates of plantar pressure. McPoil and colleagues, described 3–5 trials were needed to achieve stable estimates of plantar pressure using a two-step method over typical mid-gait strides[23]. The authors also acknowledged that the measured quantities were different using both methods[23]. We were surprised by the findings that the barefoot condition did not have the least number of steps to reach steady state. Softer midsoles in shoes have been implicated as dampening mechanoreceptor activity in the soles of the feet[24]. These findings may suggest that orthoses can help individuals reach steady state walking faster and provide for a shorter gait initiation phase. We were not entirely surprised by this finding as contoured orthoses have a better chance at stimulating more mechanoreceptor activity in the soles of the feet independent of foot type. Orthoses can also help provide stabilizing forces during gait[25–28], which may allow a wearer to reach steady state faster than without an orthoses due to increased postural stability. This potential explanation was also supported elsewhere in our data. We found that during both steady state and gait initiation phases, the dynamic balance in the medial-lateral direction was significantly improved (p<0.05) by using foot orthoses on average by 23% compared to other footwear conditions.
4.2 The impact of foot orthoses on spatio-temporal parameters of gait
Our results suggest that gait is deteriorated (i.e. longer gait initiation, lower gait speed and increase in double support time) during barefoot condition compared to both shod alone and shod with foot orthoses conditions. As indicated previously, our results also suggest that foot orthoses improve dynamic postural control during walking by reducing the COM range of motion in medio-lateral direction. Other authors have described improved postural control with foot orthoses using a variety of measures. Cobb and colleagues described improvements in center of pressure velocity after six weeks of custom foot orthoses in their patients with forefoot varus [11]. Another study of older adults reported significant improvement in Berg Balance scores in subjects wearing prefabricated foot orthoses. The improvement was seen immediately as well as 6 weeks later[12]. However, another study of middle-aged women did not find significant changes in the base of support or medial/lateral or anterior/posterior stability after four weeks of wearing various textured foot orthoses. [13].
The step-to-step transition during double support has important implications for the movement of the COM in the medio-lateral direction. It may describe 60–70% of metabolic energy expenditure during walking [29]. Several other authors have suggested minimizing the body’s center of gravity displacement from the line of progression will significantly reduce the muscular effort of walking, and consequently, save energy[30–32]. This in turn could reduce fatigue and back pain[33]. However, further study would be necessary to experimentally validate this hypothesis.
4.3 Study Limitation
There are potential limitations to our study. First, this cross-sectional study in naïve foot orthoses users may not allow enough time to adapt to the new orthoses condition. In such a scenario, the orthoses would represent challenge for the CNS because the subject does not have sufficient experience walking in orthoses to maintain normal gait and thus takes longer to accommodate for an altered walking surface. This notion is reinforced by studies that have shown a “negative” impact on spatiotemporal gait parameters when subjects walk on irregular surfaces under dual task conditions[34]. Second, there may be residual confounding in our results from lack of strict inclusion and exclusion criteria in this healthy subject population free from significant orthopedic conditions. Finally, although statistically significant differences were observed, it would be helpful to see these findings replicated in a larger study.
5. Conclusion
In conclusion, under single task walking conditions, the shod with foot orthoses condition resulted in significantly fewer number of steps needed to reach steady state walking. Considering that many falls in elderly people occur during initiating walking[18, 35], the developed algorithm for discriminating between gait initiation and gait steady state, may represent a new potential target for interventions designed to mitigate the risk of falling and/or improve postural stability.
Acknowledgements
This study was supported by Award Number T35DK074390 from the National Institute of Diabetes And Digestive And Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes And Digestive And Kidney Diseases or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Miller CA, Verstraete MC. A mechanical energy analysis of gait initiation. Gait Posture. 1999;9(3):158–166. doi: 10.1016/s0966-6362(99)00008-9. [DOI] [PubMed] [Google Scholar]
- 2.Aminian K, Trevisan C, Najafi B, Dejnabadi H, Frigo C, Pavan E, Telonio A, Cerati F, Marinoni EC, Robert P, Leyvraz PF. Evaluation of an ambulatory system for gait analysis in hip osteoarthritis and after total hip replacement. Gait & Posture. 2004;20(1):102–107. doi: 10.1016/S0966-6362(03)00093-6. [DOI] [PubMed] [Google Scholar]
- 3.Aminian K, Najafi B, Bula C, Ph LPFR. Spatio-temporal parameters of gait measured by an ambulatory system using miniature gyroscopes. Journal of Biomechanics. 2002;35(5):689–699. doi: 10.1016/s0021-9290(02)00008-8. [DOI] [PubMed] [Google Scholar]
- 4.Nissan M. The initiation of gait in lower limb amputees: some related data. J Rehabil Res Dev. 1991;28(2):1–12. doi: 10.1682/jrrd.1991.04.0001. [DOI] [PubMed] [Google Scholar]
- 5.Brunt D, Santos V, Kim HD, Light K, Levy C. Initiation of movement from quiet stance: comparison of gait and stepping in elderly subjects of different levels of functional ability. Gait Posture. 2005;21(3):297–302. doi: 10.1016/j.gaitpost.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Brunt D, Liu S-M, Trimble M, Bauer J, Short M. Principles underlying the organization of movement initiation from quiet stance. Gait & Posture. 1999;10(2):121. doi: 10.1016/s0966-6362(99)00020-x. [DOI] [PubMed] [Google Scholar]
- 7.Liu S-M, Brunt D, Bauer J. Principles underlying the organization of gait initiation and stepping. Gait & Posture. 1998;7(2):173. doi: 10.1016/s0966-6362(99)00020-x. [DOI] [PubMed] [Google Scholar]
- 8.Elble RJ, Cousins R, Leffler K, Hughes L. Gait initiation by patients with lower-half parkinsonism. Brain. 1996;119(Pt 5):1705–1716. doi: 10.1093/brain/119.5.1705. [DOI] [PubMed] [Google Scholar]
- 9.Nigg BM. The role of impact forces and foot pronation: a new paradigm. Clin J Sport Med. 2001;11(1):2–9. doi: 10.1097/00042752-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Richie DH., Jr. Effects of foot orthoses on patients with chronic ankle instability. J Am Podiatr Med Assoc. 2007;97(1):19–30. doi: 10.7547/0970019. [DOI] [PubMed] [Google Scholar]
- 11.Cobb SC, Tis LL, Johnson JT. The effect of 6 weeks of custom-molded foot orthosis intervention on postural stability in participants with >or=7 degrees of forefoot varus. Clin J Sport Med. 2006;16(4):316–322. doi: 10.1097/00042752-200607000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Mulford D, Taggart HM, Nivens A, Payrie C. Arch support use for improving balance and reducing pain in older adults. Appl Nurs Res. 2008;21(3):153–158. doi: 10.1016/j.apnr.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Wilson ML, Rome K, Hodgson D, Ball P. Effect of textured foot orthotics on static and dynamic postural stability in middle-aged females. Gait Posture. 2008;27(1):36–42. doi: 10.1016/j.gaitpost.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Winter DA. Human balance and posture control during standing and walking. Gait & Posture. 1995;3(4):193. [Google Scholar]
- 15.Aminian K, Najafi B. Capturing human motion using body-fixed sensors: Outdoor measurement and clinical applications. Computer Animation and Virtual Worlds. 2004;15(2):79–94. [Google Scholar]
- 16.Najafi B, Helbostad JL, Moe-Nilssen R, Zijlstra W, Aminian K. Does walking strategy in older people change as a function of walking distance? Gait Posture. 2009;29(2):261–266. doi: 10.1016/j.gaitpost.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Zijlstra W, Aminian K. Mobility assessment in older people: new possibilities and challenges. Eur J Ageing. 2007;4:3–12. doi: 10.1007/s10433-007-0041-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Najafi B, Aminian K, Loew F, Blanc Y, Robert PA. Measurement of stand-sit and sit-stand transitions using a miniature gyroscope and its application in fall risk evaluation in the elderly. Ieee Transactions on Biomedical Engineering. 2002;49(8):843–851. doi: 10.1109/TBME.2002.800763. [DOI] [PubMed] [Google Scholar]
- 19.Najafi B, Aminian K, Paraschiv-Ionescu A, Loew F, Bula CJ, Robert P. Ambulatory system for human motion analysis using a kinematic sensor: Monitoring of daily physical activity in the elderly. Ieee Transactions on Biomedical Engineering. 2003;50(6):711–723. doi: 10.1109/TBME.2003.812189. [DOI] [PubMed] [Google Scholar]
- 20.Aminian K, Najafi B, Bula C, Leyvraz PF, Robert P. Spatio-temporal parameters of gait measured by an ambulatory system using miniature gyroscopes. Journal of Biomechanics. 2002;35(5):689–699. doi: 10.1016/s0021-9290(02)00008-8. [DOI] [PubMed] [Google Scholar]
- 21.Deillon V, Najafi B, Thomi M, Piot-Ziegler C, Rochat S, Bula C, Aminian K. Evaluation of standing balance using a body fixed kinematic sensor, ESMAC Abstracts 2004. Gait & Posture. 2004;20 Supplement 1:S61–S112. [Google Scholar]
- 22.Lindemann U, Najafi B, Zijlstra W, Hauer K, Muche R, Becker C, Aminian K. Distance to achieve steady state walking speed in frail elderly persons. Gait Posture. 2008;27(1):91–96. doi: 10.1016/j.gaitpost.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 23.McPoil TG, Cornwall MW, Dupuis L, Cornwell M. Variability of plantar pressure data. A comparison of the two-step and midgait methods. J Am Podiatr Med Assoc. 1999;89(10):495–501. doi: 10.7547/87507315-89-10-495. [DOI] [PubMed] [Google Scholar]
- 24.Robbins S, Waked E, Allard P, McClaran J, Krouglicof N. Foot position awareness in younger and older men: the influence of footwear sole properties. J Am Geriatr Soc. 1997;45(1):61–66. doi: 10.1111/j.1532-5415.1997.tb00979.x. [DOI] [PubMed] [Google Scholar]
- 25.MacLean C, Davis IM, Hamill J. Influence of a custom foot orthotic intervention on lower extremity dynamics in healthy runners. Clin Biomech (Bristol, Avon) 2006;21(6):623–630. doi: 10.1016/j.clinbiomech.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 26.MacLean CL, Davis IS, Hamill J. Short- and long-term influences of a custom foot orthotic intervention on lower extremity dynamics. Clin J Sport Med. 2008;18(4):338–343. doi: 10.1097/MJT.0b013e31815fa75a. [DOI] [PubMed] [Google Scholar]
- 27.Maclean CL, Davis IS, Hamill J. Influence of running shoe midsole composition and custom foot orthotic intervention on lower extremity dynamics during running. J Appl Biomech. 2009;25(1):54–63. doi: 10.1123/jab.25.1.54. [DOI] [PubMed] [Google Scholar]
- 28.Nester CJ, van der Linden ML, Bowker P. Effect of foot orthoses on the kinematics and kinetics of normal walking gait. Gait Posture. 2003;17(2):180–187. doi: 10.1016/s0966-6362(02)00065-6. [DOI] [PubMed] [Google Scholar]
- 29.Kuo AD. The six determinants of gait and the inverted pendulum analogy: A dynamic walking perspective. Hum Mov Sci. 2007;26(4):617–656. doi: 10.1016/j.humov.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 30.Perry J. Gait analysis of normal and pathological function. Thorofare: Slack Inc; 1992. [Google Scholar]
- 31.Malanga G, Delisa J. Clinical Observation. In: DeLisa J, editor. Gait analysis in the science of rehabilitation. Baltimore: Diane Publishing; 2000. p. 2. [Google Scholar]
- 32.Seymour R. Prosthetics and orthotics: lower limb and spinal. Philadelphia: Lippincott, Williams & Wilkins; 2002. [Google Scholar]
- 33.Wrobel J, Edgar S, Cozzetto D, Maskill J, Peterson P, Najafi B. A proof in concept study for measuring gait speed, steadiness, and dynamic balance under various footwear conditions outside of the gait lab? Journal of the American Podiatric Medical Association. 2010 doi: 10.7547/1000242. (In Press) [DOI] [PubMed] [Google Scholar]
- 34.Menant JC, Steele JR, Menz HB, Munro BJ, Lord SR. Effects of walking surfaces and footwear on temporo-spatial gait parameters in young and older people. Gait Posture. 2009;29(3):392–397. doi: 10.1016/j.gaitpost.2008.10.057. [DOI] [PubMed] [Google Scholar]
- 35.Nyberg L, Gustafson Y. Patient falls in stroke rehabilitation. A challenge to rehabilitation strategies. Stroke. 1995;26(5):838–842. doi: 10.1161/01.str.26.5.838. [DOI] [PubMed] [Google Scholar]