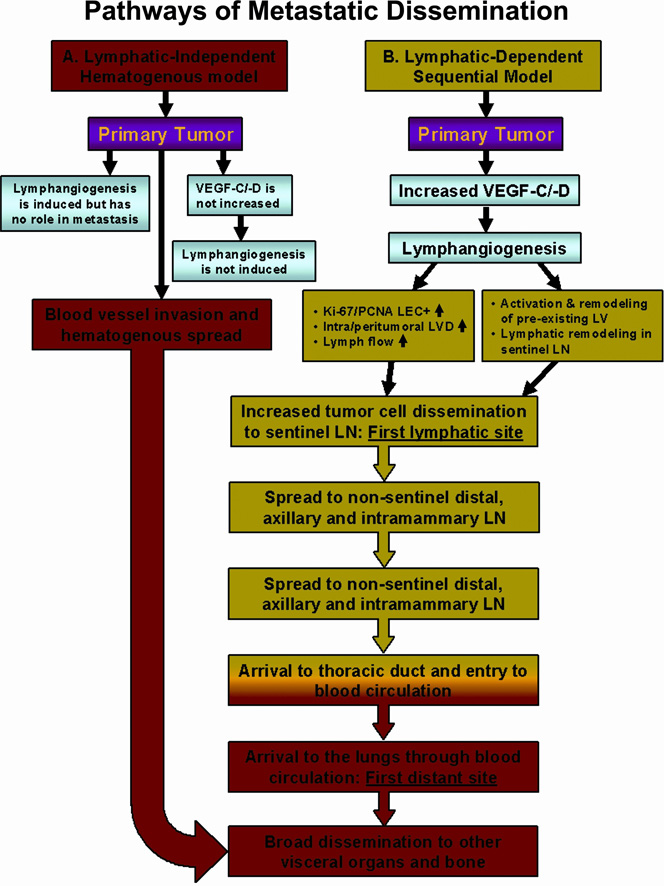
Figure 1. Comparison of lymphatic-independent (hematogenous) and lymphatic-dependent (lymphogenous) pathways of metastatic dissemination.
A. Lymphatic-independent, hematogenous metastatic model. This concept implies that lymphangiogenesis is either not induced or, if induced, new lymphatic vessels do not contribute to tumor dissemination. It is envisioned that the main disseminating pathway is through invasion of intratumoral blood vessels that deliver metastatic cells to distant organs such as lung, liver, bone, and brain. Based on this model, aggressive tumor cells may also invade pre-existing peritumoral lymphatics that transport tumor cells to loco-regional nodes; however, node-derived metastatic cells do not contribute to distant metastasis. B. Lymphatic-dependent, sequential model of dissemination in breast cancer. The second model suggests that breast tumors induce intratumoral or peritumoral lymphangiogenesis as well as remodeling of the lymphatic system in the sentinel and distal lymph nodes. This is manifested by increased number of lymphatic vessels, increased frequency of dividing lymphatic endothelial cells and increased lymph flow between the primary tumor and the sentinel node. These attributes promote tumor cell dissemination through tumor-associated lymphatic vessels to the sLN and spread to intramammary and axillary lymph nodes. Nodal metastatic cells can use either lymphatic or blood vessels for subsequent dissemination. Transport through the lymphatic system ends in the entering the thoracic duct whose contents are subsequently mixed with the venous blood, giving rise to metastatic lesions in the lungs and other visceral organs. Two models are not mutually excluding and in some tumors, hematogenous and lymphogenous metastasis may occur simultaneously.