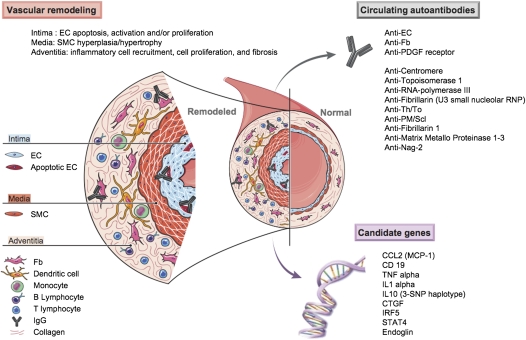
Figure 2.
Pulmonary vascular remodeling in systemic sclerosis–related pulmonary arterial hypertension (SSc-PAH). This schematic features inflammatory mediators, cells, and mechanisms involved in the pulmonary vascular remodeling of SSc-PAH. Vascular changes affect all three layers (i.e., intima, media, adventitia) of the pulmonary vessel, and involve endothelial cell (EC) apoptosis, EC activation with increased expression of cell adhesion molecules, and inflammatory cell recruitment leading to vessel obliteration. A number of circulating autoantibodies including classic autoantibodies, such as anti-centromere, anti-topoisomerase 1, anti–RNA-polymerase III, anti-fibrillarin (U3 small nucleolar ribonucleoprotein [RNP]), anti-Th/To, and anti- polymyositis/scleroderma (PM/Scl), and more recently anti-fibrillarin 1, anti–matrix metalloproteinases (MMP) 1–3, anti–novel antigen (nag)-2 (nonsteroidal antiinflammatory drug-activated gene), and evidence that anti-fibroblast (Fb) antibodies, anti-EC antibodies (AECA), and anti–platelet-derived growth factor (PDGF) receptor antibodies might exert a pathogenic role. An increasing number of candidate genes have been reported to be associated with SSc in different cohorts, including, among others, a variant in the promoter of chemokine (C-C motif) ligand 2 (monocytes chemotactic protein-1) (CCL2 [MCP-1]), two variants in cluster of differentiation 19 (CD19), a promoter and coding polymorphism in tumor necrosis factor (TNF)-α, a variant in the promoter of IL-1α gene, a three–single-nucleotide polymorphism (SNP) haplotype in IL-10, a polymorphism in the connective tissue growth factor (CTGF) promoter region, the interferon regulatory factor 5 (IRF5) rs2004640 GT substitution, and the signal transducer and activator of transcription 4 (STAT4) rs7574865 single nucleotide polymorphism. Specific mechanisms are further detailed in the text. SMC = smooth muscle cell.