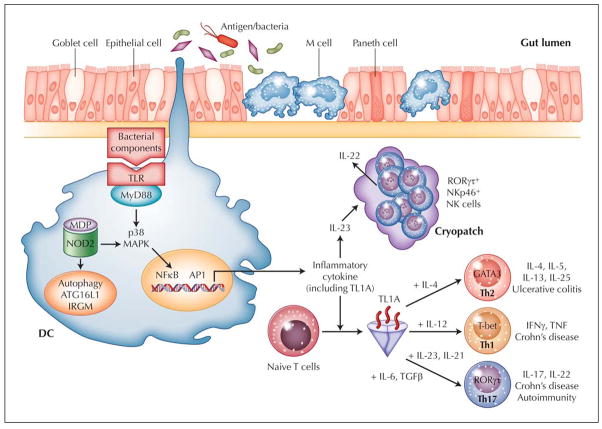
Figure 1.
Working hypothesis of inflammatory bowel disease. Intestinal immune system is in close apposition to luminal antigen/bacteria, which are separated by a single layer of epithelial cells. Goblet cells contribute to the formation of the protective mucus layer, and M cells and dendritic cells (DC) sample intestinal luminal contents. Overresponse to antigens, either through Toll-like receptors (TLR), intracellular sensor NOD2, or antigen processing via autophagy, results in stimulated DC that recruit and generate T-cell (Th1, Th2, and Th17) and NK-cell subtypes. One subpopulation of RORγt+NKp46+ NK cells that resides in gut cryptopatches is found to readily produce IL-22 in response to IL-23, likely released by DC. IL-22 may play an important role in epithelial homeostasis, bacteria clearance, and tissue repair. TL1A appears to be a critical factor important in generating Th1, Th2, and Th17 cells. For each T-helper cell differentiation program, specific transcription factors and cytokine milieu are required (indicated in the figure). Terminally differentiated T-helper cells are characterized by a specific combination of effector cytokines (indicated in the figure) that orchestrate effector function of the adaptive immune system. Crohn’s disease is a predominantly Th1- and Th17-mediated process, whereas ulcerative colitis appears to be mediated by Th2 and possibly Th17.