Abstract
Anterior odontoid screw fixation is a safe and effective method for treatment of odontoid fractures. The screw treads should fit into the odontoid medulla, should pass the fracture line, and should pull fractured odontoid tip against body of axis in order to achieve optimum screw placement and treatment. This study has demonstrated optimal anterior odontoid screw thickness, length, and optimal angle for safe and strong anterior odontoid screw placement. Dry bone axis vertebrae were evaluated by direct measurements, X-ray measurements, and computerized tomography (CT) measurements. The screw thickness (inner diameter of the odontoid) was measured as well as screw length (distance between anterior-inferior point body of axis and tip of odontoid), and screw angle (the angle between basis of axis and tip of odontoid). The inner diameter of odontoid bone was measured as 6.5 ± 1.9 mm, the screw length was 37.6 ± 3.3 mm, and the screw angle was 62.4 ± 4.7 on CT. There was no statistical difference between X-ray and CT in the measurements of screw thickness and angle. X-ray and CT measurements are both safe methods to determine the inner odontoid diameter and angle preoperatively. Screw length should be measured on CT only. To provide safe and strong anterior odontoid screw fixation, screw thickness, length, and angle should be known preoperatively, and these can be measured on X-ray and CT.
Keywords: Axis, Screw fixation, Anatomical study, X-ray, Computerized tomography
Introduction
Fractures of the axis involving odontoid represent a fairly common entity of spinal injury accounting for 10–18% of all cervical spine fractures [1, 2, 8]. This region is responsible for the majority of the segmental axial rotation of the neck. It is well documented that this is a unique area from a biomechanical standpoint and is inherently predisposed to traumatic injuries [7].
Odontoid fractures are divided into three groups, depending on the anatomical location of the fracture, according to a widely accepted classification system proposed by Anderson and D’Alonzo in 1974. It is well recognized that displaced type II and rostral “shallow” type III fractures of the odontoid process are at the highest risk for nonunion, prompting immediate intervention and stabilization to reduce the risk of irreversible compromise of the spinal cord [3, 6]. Anterior odontoid screw fixation has been used widely and provides a high union rate and preserves axial rotation. Anterior screw fixation can decrease the rate of perioperative morbidity in elderly patients in whom greater comorbidities are more likely [9].
The purpose of the current study was to emphasize the importance of the internal odontoid diameter for anterior odontoid screw placement. Thus we aimed to demonstrate the optimal screw thickness, length, and angle according to bony odontoid measurements. We also evaluated the axis vertebra with lateral X-ray and CT for these measurements.
Materials and methods
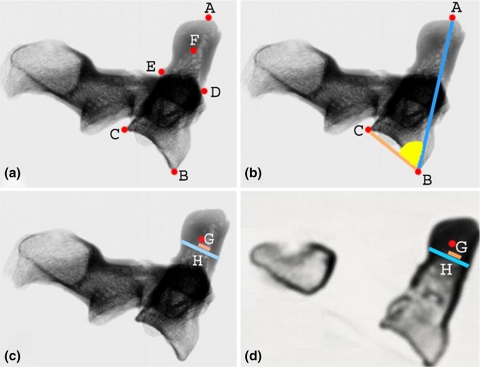
Twenty adult dry bones of axis vertebrae were obtained to evaluate the osseous anatomy of atlas from Ankara University Anatomy Department. Points and lines of vertebrae were described in Table 1. Measurements of three linear and one angular parameter were evaluated on dry bone, X-ray, and CT for each axis vertebrae (Fig. 1).
Table 1.
Description of points and lines measured on sagittal plane of axis vertebra
| A | Odontoid tip |
| B | Anterior-inferior point of the body of axis = screw entry point |
| C | Posterior-inferior point of the body of axis |
| D | Anterior-inferior point of the odontoid base |
| E | Posterior-inferior point of the odontoid body |
| F | Odontoid midpoint = middle point of odontoid tip and odontoid base |
| G | The inner diameter of the odontoid |
| H | The outer diameter of the odontoid |
| BA line | Screw length |
| ABC angle | Screw angle on axis |
Fig. 1.
a Lateral X-rays of axis vertebra demonstrates points. See Table 1 for abbreviations; b lateral X-rays of axis vertebra demonstrates ABC angle = screw angle; c lateral X-rays of axis vertebra demonstrates G the inner diameter of the odontoid; H the outer diameter of the odontoid. d Sagittal computerized tomography reconstruction demonstrating the inner diameter of the odontoid and the outer diameter of the odontoid
Anatomical measures on bony specimens were calculated to confirm the accuracy of X-ray and computerized tomography (CT) measurements. All direct anatomical measurements were performed by using a digital micrometer (Mitutoyo Corporation, Japan). Digital X-rays (47 kV, 4 mA) of axis were obtained in right lateral projection with focus-film-distance of 100 cm. Computerized tomography studies were performed with 0.5-mm-slice thickness, and parallel to base of axis. Sagittal and coronal three-dimensional (3-D) reconstructions of CT scans were then obtained. Sagittal 3-D reconstructions were prepared in an odd numbered arrangement, and central image was used for measurements in the study.
Parameters on digital X-rays and on CTs were measured using computerized image analysis software “Digital Image Tool”.
Statistical analysis
Wilcoxon matched pairs signed rank tests that utilize non-parametric data from two related samples were used to compare the results, and Friedman test was used for data from more than two related samples (p < 0.05 is significant). Variability was expressed as mean ± standard deviation.
Results
Results of anatomical, X-ray, and CT measurements are shown in Table 2.
Screw thickness X-ray and CT measurements were compared.
There was no statistical difference between X-ray and CT for the inner diameter of the odontoid (p > 0.05), and it is measured as 6.5 ± 1.9 mm, on CT.
Screw length Bone, X-ray, and CT measurements were compared.
There were statistical differences between bone and X-ray measurements (p < 0.05). An X-ray measurement may not be reliable to determine screw length.
There was no difference between bone and CT measurements (p > 0.05).
There was statistical difference between X-ray and CT measurements (p < 0.05). CT measurements are safer to determine screw length (37.6 ± 3.3 mm, on CT)
Screw angle X-ray and CT measurements were compared.
There was no statistical difference between X-ray and CT for screw angle (p > 0.05), and it is measured as 62.4 ± 4.7º, on CT.
Table 2.
Summary of values measured in axis
| X-ray | Computerized tomography | Anatomical | P value | |
|---|---|---|---|---|
| G | 6.2 ± 2.2 mm | 6.5 ± 1.9 mm | – | 0.191 |
| H | 11.8 ± 1.5 mm | 11.3 ± 0.9 mm | – | 0.131 |
| BA line | 39.9 ± 5.1 mm | 38.0 ± 4.0 mm | 37.6 ± 3.3 mm | 0.006* |
| ABC angle | 64.2 ± 4.1º | 62.4 ± 4.7º | – | 0.073 |
G The inner diameter of the odontoid, H the outer diameter of the odontoid, BA line screw length, ABC angle screw angle on axis
* Significant at the 0.05 level
Discussion
Anterior odontoid screw fixation is a safe and effective method to treat odontoid fractures. It offers several benefits including preservation of motion and axial rotation, and provides rigid internal fixation in the treatment of type II odontoid fractures. It also provides optimum conditions for bony fusion, and there is no need to harvest autologous bones graft. This technique avoids halo immobilization and has been shown to achieve a high fusion rate, similar to that of posterior atlantoaxial arthrodesis (92–100%) with a similar complication rate [4, 14, 15].
Although one or two screw techniques have been advocated, high fusion rate does not depend on the number of screws used [11, 18]. For 2-screw method, the critical transverse outer diameter of odontoid is recommended; at least 9 mm for the placement of two 3.5 mm cortical screws [16]. In our measurements, the outer diameter was found to be 11.3 ± 0.9 mm and well correlated with Schaffer et al.’s study as 11.6 mm [19], with Kandziora et al.’s study as 10.9 mm [12]. Chang et al. reported that type II odontoid fractures stabilized with a single 4.5 mm cannulated Herbert screw have increased torsional stiffness as compared with a 2-screw technique using 3.5 mm anterior odontoid screws [4]. Increasingly, many surgeons use one central screw in an attempt to purchase the cortical tip of the odontoid [4, 11].
In one anterior odontoid screw technique, the inner diameter of odontoid has an utmost importance. The screw thread should fit exactly the odontoid medulla (inner odontoid diameter) to obtain better screw placement and to obtain stronger pull force of fractured piece to main body of axis. Thinner screws may result in screw loosening whereas thicker screws may result in breaking of odontoid bone. The inner diameter of odontoid has not been published in the literature earlier. In our study, the inner diameter of odontoid is measured as 6.5 ± 1.9 mm, and the screw thickness should be close to this measure. Axial CT should be obtained for every case for determining proper screw diamater; thus some cases may deserve 5 mm screw whereas the others 8 mm.
Proper instrumentation in anterior odontoid screw technique requires that screw should pull the fractured odontoid piece against body of axis. The pressure at the fractured edges and the stabilization augment healing of the fracture. Therefore screw length is very important and should be measured preoperatively. Short screws were insufficient to pass the fracture line and do not penetrate to the odontoid tip and do not pull fractured odontoid piece. Likewise, long screws may perforate the odontoid tip and could lead to vertebral artery and neural tissue damage. The body of axis and odontoid height was reported to be 37.8 mm by Heller et al. [10], and 39.9 mm by Doherty et al. [5]. The body of axis and odontoid height does not represent correct screw length because they did not use the landmarks of real screw trajectory for anterior odontoid screw fixation. In the present study, screw length was measured as the line through anterior-inferior point of the body of axis to odontoid tip, and it represents real screw trajectory and screw angle. In our study, screw length is 37.6 mm, and this result is well correlated with the literature [5, 10]. Xu et al. reported that a lateral X-ray may not be reliable in determining the optimal screw length but it could be valuable in directing accurate screw angle in the sagittal plane [20]. Lee reported that axial, sagittal, and coronal 3-D reconstruction CT is used to determine the precise patterns of osseous injury [13]. Due to the statistical difference which was found between X-ray and CT and also X-ray and anatomical measures screw length should be measured on CT rather than X-ray.
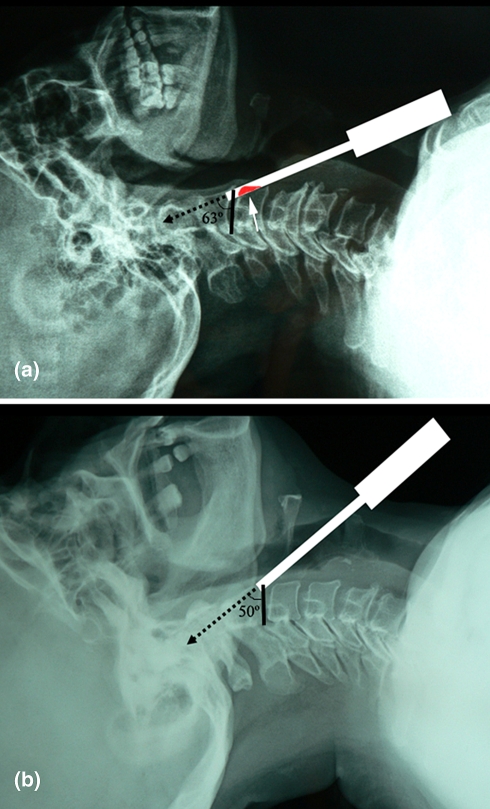
Screw insertion angle is very important in anterior odontoid screw fixation and can be evaluated preoperatively by either X-ray or CT because there is no difference between these two methods in the present study. The corpus angle is the angle between the lines of basis (CB) and screw line (AB), and this has not been published earlier in the literature (Fig. 1b). It was measured as 62.4 ± 4.7º, on CT. In preoperative evaluation, corpus angle also shows the relation of odontoid screw line and superior anterior edge of third cervical vertebra. In case where the odontoid has a bigger angle, superior anterior portion of third cervical vertebra may need to be rimmed in order to have room for screw driver, whereas odontoid with smaller angle can be screwed easily without any rimming (Fig. 2). Surgeons should be aware that physical characteristics of patients such as concomitant thoracic kyphosis, short neck, barrel chest deformity, and fracture configurations that require a flexed position to obtain and maintain reduction [4, 17], may limit the application of the technique and may prevent hyperextension and impede ideal screw trajectory during positioning. .
Fig. 2.
a Lateral cervical X-ray demonstrates if odontoid has bigger screw angle, anterior-inferior third cervical vertebra needs to be rimmed. Dotted arrow screw; white arrow third cervical vertebra’s rimmed area. b Lateral cervical X-ray demonstrates if odontoid has smaller screw angle, anterior-inferior third cervical vertebra does not need to be rimmed. Dotted arrow screw
Conclusions
Individual X-ray and CT measurements are both easy methods to determine the inner odontoid diameter and screw angle preoperatively. Screw length should be measured on 3-D CT. These measures give better understanding and imagination of the screwing step of the operation and hence, one can give easier and correct position to the patient on operating table.
Contributor Information
Erkan Kaptanoglu, Phone: +90-312-5085262, Email: erkankaptanoglu@yahoo.com.
Berker Cemil, Email: berker5@yahoo.com.
References
- 1.Alfieri A. Single-screw fixation for acute type II odontoid fracture. J Neurosurg Sci. 2001;45:15–18. [PubMed] [Google Scholar]
- 2.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–1674. [PubMed] [Google Scholar]
- 3.Carlson GD, Heller JG, Abitbol JJ. Odontoid fractures. In: Levine AM, editor. Spine trauma. Philadelphia: WB Saunders Co; 1998. pp. 227–248. [Google Scholar]
- 4.Chang KW, Liu YW, Cheng PG, et al. One Herbert double-threaded compression screw fixation of displaced type II odontoid fractures. J Spinal Disord. 1994;7:62–69. doi: 10.1097/00002517-199407010-00009. [DOI] [PubMed] [Google Scholar]
- 5.Doherty BJ, Heggeness MH. Quantitative anatomy of the second cervical vertebra. Spine. 1995;20:513–517. doi: 10.1097/00007632-199503010-00002. [DOI] [PubMed] [Google Scholar]
- 6.Fountas KN, Kapsalaki EZ, Karampelas I, et al. Results of long-term follow-up in patients undergoing anterior screw fixation for type II and rostral type III odontoid fractures. Spine. 2005;30:661–669. doi: 10.1097/01.brs.0000155415.89974.d3. [DOI] [PubMed] [Google Scholar]
- 7.Fountas KN, Machinis TG, Kapsalaki EZ, et al. Surgical treatment of acute type II and rostral type III odontoid fractures managed by anterior screw fixation. South Med J. 2005;98:896–901. doi: 10.1097/01.SMJ.0000177342.81752.74. [DOI] [PubMed] [Google Scholar]
- 8.Hanssen AD, Cabanela ME. Fractures of the dens in adult patients. J Trauma. 1987;27:928. doi: 10.1097/00005373-198708000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Harrop JS, Sharan AD, Przybylski GJ. Epidemiology of spinal cord injury after acute odontoid fractures. Neurosurg Focus. 2000;8:e4. [PubMed] [Google Scholar]
- 10.Heller JG, Alson MD, Schaffler MB, et al. Quantitative internal dens morphology. Spine. 1992;17:861–866. doi: 10.1097/00007632-199208000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Jenkins JD, Coric D, Branch CL., Jr A clinical comparison of one- and two-screw odontoid fixation. J Neurosurg. 1998;89:366–370. doi: 10.3171/jns.1998.89.3.0366. [DOI] [PubMed] [Google Scholar]
- 12.Kandziora F, Schulze-Stahl N, Khodadadyan-Klostermann C, et al. Screw placement in transoral atlantoaxial plate systems: an anatomical study. J Neurosurg. 2001;95:80–87. doi: 10.3171/spi.2001.95.1.0080. [DOI] [PubMed] [Google Scholar]
- 13.Lee SC, Chen JF, Lee ST. Management of acute odontoid fractures with single anterior screw fixation. J Clin Neurosci. 2004;11:890–895. doi: 10.1016/j.jocn.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 14.Marchesi DG. Management of odontoid fractures. Orthopedics. 1997;20:911–916. doi: 10.3928/0147-7447-19971001-06. [DOI] [PubMed] [Google Scholar]
- 15.McCullen GM, Garfin SR. Spine update: cervical spine internal fixation using screw and screw-plate constructs. Spine. 2000;25:643–652. doi: 10.1097/00007632-200003010-00020. [DOI] [PubMed] [Google Scholar]
- 16.Nucci RC, Seigal S, Merola AA, et al. Computed tomographic evaluation of the normal adult odontoid. Implications for internal fixation. Spine. 1995;20:264–270. doi: 10.1097/00007632-199502000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Reindl R, Sen M, Aebi M. Anterior instrumentation for traumatic C1–C2 instability. Spine. 2003;28:329–333. doi: 10.1097/01.BRS.0000083328.27907.3B. [DOI] [PubMed] [Google Scholar]
- 18.Sasso R, Doherty BJ, Crawford MJ, et al. Biomechanics of odontoid fracture fixation. Comparison of the one- and two-screw technique. Spine. 1993;18:1950–1953. doi: 10.1097/00007632-199310001-00004. [DOI] [PubMed] [Google Scholar]
- 19.Schaffler MB, Alson MD, Heller JG, et al. Morphology of the dens. A quantitative study. Spine. 1992;17:738–743. doi: 10.1097/00007632-199207000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Xu R, Ebraheim NA, Misson JR, et al. The reliability of the lateral radiograph in determination of the optimal transarticular C1–C2 screw length. Spine. 1998;23:2190–2194. doi: 10.1097/00007632-199810150-00009. [DOI] [PubMed] [Google Scholar]