Abstract
Background
The aims of this study were to determine the prevalence and incidence of patellofemoral pain (PFP) in young female athletes and prospectively evaluate measures of frontal plane knee loading during landing to determine their relationship to development of PFP. We hypothesized that increased dynamic knee abduction measured during preseason biomechanical testing would be increased in those who developed PFP relative to teammates who did not develop PFP.
Methods
Middle and high school female athletes (n=240) were evaluated by a physician for PFP and for landing biomechanics prior to their basketball season. The athletes were monitored for athletic exposures and PFP injury during their competitive seasons.
Findings
At the beginning of the season, the point prevalence of PFP was 16.3 per 100 athletes. The cumulative incidence risk and rate for the development of new unilateral PFP was 9.66 per 100 athletes and 1.09 per 1000 athletic exposures, respectively. All new PFP developed in middle school athletes who demonstrated mean International Knee Documentation Committee score of 85.6 ± 7.7 at diagnosis. The new PFP group demonstrated increased knee abduction moments at initial contact (95% CI: 0.32 to 4.62 Nm) on the most-symptomatic limb and maximum (95% CI: 1.3 to 10.1 Nm; p=0.02) on the least-symptomatic (or no symptoms) limb relative to the matched control limbs. Knee abduction moments remained increased in the new PFP group when normalized to body mass (p<0.05).
Interpretation
The increased knee abduction landing mechanics in the new PFP group indicate that frontal plane loads contribute to increased incidence of PFP.
Keywords: Patellofemoral Pain Syndrome, Anterior Knee Pain, Biomechanics, Neuromuscular Control, Knee Valgus
Introduction
Retropatellar and peripatellar pain, clinically referred to as patellofemoral pain (PFP), is a common pain disorder experienced by young adult and adolescent athletes who participate in jumping cutting and pivoting sports.(Heintjes et al., 2005, Louden et al., 2004, Natri et al., 1998, Witvrouw et al., 2000, Kannus et al., 1987) Up to 40% of clinical visits for knee problems are attributed to PFP (Natri et al., 1998, Kannus et al., 1987) and adolescent females and young adult women are affected more often (2 to 10 times) with PFP than their male counterparts.(Robinson and Nee, 2007, Fulkerson, 2002, Fulkerson and Arendt, 2000) Fairbanks and colleagues reported PFP symptoms can affect up to 30% of young students (13-19 years) and the symptoms may cause 74% to limit their sport activities or lead to sports cessation.(Blond and Hansen, 1998, Fairbank et al., 1984) Symptoms of PFP that restrict young athletes from participating in recreational activities may also limit them from the health benefits of regular physical activity.(CDC, 2006, Heintjes et al., 2005, Crossley et al., 2005, Christou, 2004) In addition, current evidence contradicts the assumption that PFP runs a benign and self-limiting course; on the contrary, PFP is a likely contributor to long term patellofemoral osteoarthritis.(Utting et al., 2005)
Prior biomechanical investigations have reported altered neuromuscular strategies in patients with active symptomatic PFP.(Bolgla et al., 2008, Willson et al., 2008, Robinson and Nee, 2007, MacIntyre et al., 2006) Differences in whole body power and static alignments found in patients with symptomatic PFP may also be risk factors that contribute to the genesis of PFP. Witvrouw and colleagues conducted one of the early investigations that aimed to prospectively determine the intrinsic risk factors for the development of PFP.(Witvrouw et al., 2000) Prior to the start of physical education training they evaluated male and female students enrolled in a physical education class for anthropometric variables, motor performance, general joint laxity, lower leg alignment characteristics, muscle length and strength, static and dynamic patellofemoral characteristics, and psychological parameters. Over a two year period, they found that shortened quadriceps muscles, an altered vastus medialis obliquus muscle reflex response time, decreased explosive strength and jumping power, and a hypermobile patella were significantly related to the incidence of PFP. A recent study by Stefanyshyn and colleagues prospectively followed long distance runners to determine predictive factors that lead to PFP. Their results indicated an increased knee frontal plane impulse moment was evident during single support stance phase of running in subjects who developed PFP.(Stefanyshyn et al., 2006) Similarly, Rauh and colleagues reported that high school cross-country runners with abnormal frontal plane static alignments (Q-angle measures of 20 or more degrees) were more likely to miss practice or competition from an injury to their knee.(Rauh et al., 2007) While increased frontal plane alignments and loads are associated with patellofemoral pain and knee injury incidence in endurance athletes, this association has not been reported in random, intermittent, dynamic sport (Bloomfield et al., 2007) athletes.(Cahue et al., 2004, Huberti and Hayes, 1984)
Altered or decreased neuromuscular control during the execution of sports movements, which result in excessive resultant out of plane (especially frontal plane) knee joint motion and load, appear to increase risk of acute knee injury in female athletes and may contribute to the development of PFP.(Hewett et al., 2005) Army recruits who landed from a jump with a combination of reduced knee flexion, increased out of plane hip rotation and frontal plane foot laxity were at increased risk for the development of PFP.(Boling et al., 2009) Previous authors have suggested that abnormal frontal plane kinematics and moments that are associated with acute injury may also be related to PFP development in young athletes, but this relationship has not been prospectively examined in random, intermittent, dynamic sport populations who develop PFP injury.(Powers, 2003, Hewett et al., 2005) At small knee flexion angles (19-22 degrees) commonly reported in female athletes when initiating a landing, abnormal frontal plane patellofemoral joint kinematics are evident in PFP patients.(Ford et al., 2010, MacIntyre et al., 2006) Specifically, at 19 degrees of knee flexion, patients with symptomatic PFP pain presented with a laterally aligned patella, which is also associated with increased knee abduction.(MacIntyre et al., 2006) Cumulatively, the current evidence indicate that increased frontal plane knee alignments and loads, especially at small knee flexion angles similar to those found at initial contact of a jump landing, should be evaluated to determine their contribution to PFP onset.
The absence of consensus regarding factors that increase the risk of PFP in random, intermittent, dynamic sport athletes limit the potential to optimize prevention and treatment of this disorder in these populations. The objectives of this study were 1) to determine the prevalence and incidence of patellofemoral pain (PFP) in young female athletes, and 2) to prospectively determine the relationships between measures of frontal plane knee loading during landing and development of patellofemoral pain. We hypothesized that increased dynamic knee abduction measured during preseason biomechanical testing of landing mechanics would be increased in those who developed PFP relative to teammates who did not develop PFP.
Methods
Subjects
Female basketball players were recruited from a county public school district with five middle schools and three high schools. From the six high school and fifteen middle school basketball teams identified from these schools, 174 middle school and 66 high school basketball players (mean age 13.4 years, height 160.6 cm, mass 54.5 kg and percent of adult stature 91.1%) agreed to participate in this study. Group specific (PFP and CTRL) demographic and anthropometric data are presented in Table 1.
Table 1.
Mean (±1SD) demographic and static anthropometrics for the CTRL and PFP groups.
| CTRL (n=131) | New PFP (n=14) | P-value | |
|---|---|---|---|
| Age (years) | 13.4 ± 1.6 | 12.7 ± 1.0 | 0.10 |
| Adult Stature (%) | 91.1% ± 4.8% | 89.4% ± 3.7% | 0.24 |
| Height (cm) | 160.0 ± 8.0 | 160.7 ± 9.2 | 0.75 |
| Mass (kg) | 54.4 ± 11.7 | 53.1 ± 15.0 | 0.70 |
| Static Knee Abduction (deg) | 2.0 ± 3.4 | 2.5 ± 3.7 | 0.86 |
Procedures
The Institutional Review Board approved the data collection procedures and consent forms. Parental consent and athlete assent were obtained before data collection. Subjects were tested prior to the start of their competitive season. The testing consisted of anthropometrics, questionnaires to determine familial anthropometrics utilized for maturational estimates, knee exam, medical history, landing biomechanical analysis and vertical jump performance.
Knee Exam
The initial injury screening process included the Anterior Knee Pain Scale (AKPS) questionnaire.(Kujala et al., 1993) The scale is composed of 13 items that evaluate subjective symptoms and functional limitations. Minimum score is 0 points and maximum score is 100 points. An athlete with no sign of anterior knee pain would have a score of 100. All subjects with a positive AKPS (score less than 100) underwent further assessment, which included an International Knee Documentation Committee (IKDC) score for the right and left knee, a personal interview regarding current and prior knee symptoms, limitations, history and a knee physical exam by the same investigator. The AKPS is reported to be responsive, valid and demonstrates high test-retest reliability.(Crossley et al., 2004, Watson et al., 2005) In addition, the IKDC Subjective Knee Form (short form), which is a reliable and valid tool for the determination of a patient's rating of their knee symptoms, function and ability to participate in sport following knee injury, was utilized.(Irrgang et al., 2001) The constructs validated for the IKDC were swelling, pain level, and functional ability. The standardized personal interview included questions regarding the subject's severity of knee pain, participation time missed due to knee pain, timing of knee pain with activity, post play knee pain, duration of knee pain, symptoms of knee instability, and if the athlete had been evaluated by her personal physician or a specialist for the knee pain. The exam included palpation for tenderness at: medial patellofemoral ligament (MPFL), medial and lateral patellofemoral joint, medial and lateral femoral-tibial joint line, medial or lateral plica within patellofemoral joint, Gerdy's tubercle and iliotibial band, pes anserine bursa, distal pole of patella, tibial tubercle, Hoffa's fat pad, quadriceps tendon and patella tendon. Clinical tests for ligament instability, meniscal tear, and patella apprehension and mobility were also performed.
Subjects were diagnosed as having active PFP if they presented with AKPS score < 100; knee pain with or shortly following activity and also if anterior knee tenderness was present at the MPFL; medial patella facet tenderness and/or lateral patella facet tenderness; Hoffa's fat pad syndrome with fat pad swelling and tenderness over the medial and/or lateral fat pad; and plica if tenderness was present over a palpable fibrous longitudinal band between the patella and femoral condyle.
Landing Biomechanics
Three-dimensional hip, knee and ankle kinematic and kinetic data were quantified for the contact phase of three drop vertical jump (DVJ) tasks. Each subject was instrumented with 37 retroreflective markers placed on the sacrum, left posterior superior iliac spine, sternum and bilaterally on the shoulder, elbow, wrist, anterior superior iliac spine, greater trochanter, mid thigh, medial and lateral knee, tibial tubercle, mid shank, distal shank, medial and lateral ankle, heel, dorsal surface of the midfoot, lateral foot (5th metatarsal) and central forefoot (between 2nd and 3rd metatarsals). First, a static trial was conducted in which the subject was instructed to stand still with foot placement standardized to the laboratory coordinate system. This static measurement was used as each subject's neutral (zero) alignment; subsequent kinematic measures were referenced in relation to this position. In addition, the static trial was also used to calculate standing knee abduction angle measures. The drop vertical jump (DVJ) involved the subject standing on top of a box (31 cm high) with her feet positioned 35 cm apart. She was instructed to drop directly down off the box and immediately perform a maximum vertical jump, raising both arms while jumping for a basketball rebound.(Ford et al., 2003)
Three trials were collected for each subject with EVaRT (Version 4, Motion Analysis Corporation, Santa Rosa, CA) using a motion analysis system consisting of ten digital cameras (Eagle cameras, Motion Analysis Corporation, Santa Rosa, CA) positioned in the laboratory and sampled at 240 Hz. Two force platforms (AMTI, Watertown, MA) were sampled at 1200 Hz and time synchronized with the motion analysis system. The force platforms were embedded into the floor and positioned 8 cm apart so that each foot would contact a different platform during stance phase of the drop vertical jump.(Ford et al., 2003)
Data Analysis
For each subject, biomechanical variables were calculated during the drop vertical jump (DVJ) maneuver. Specifically, lower limb joint data were generated via the three-dimensional (3D) coordinates of externally mounted skin markers. Three-dimensional Cartesian marker trajectories from each trial were filtered through a low-pass filter at a cutoff frequency of 12 Hz.(Woltring et al., 1985) The vertical ground reaction force (VGRF) data recorded for each limb were used to normalize the associated kinematic data to 100% of stance at 1% increments (N=101), with initial contact defined as the instant when VGRF first exceeds 10N. From the 3D kinematic and force plate data, 3D knee abduction moments were computed using inverse dynamic analysis.(van den Bogert, 1994) Net external knee abduction moments were described in this paper and have previously demonstrated high reliability for outcome measurement in our laboratory.(Ford et al., 2007) Vertical jump height (a whole body power measurement) was calculated from the involved greater trochanter marker in the vertical axis and the recorded displacement between the standing height and the maximum height attained during the drop vertical jump.
Athlete Tracking, Follow-up, Exclusionary Criteria and Control Group
The athletes were monitored on a weekly basis for athletic exposures (AEs), new PFP injury, or any other lower extremity injury with resultant time loss, by a certified athletic trainer. AEs were defined as 1 game or practice session. The AEs of subjects with preseason PFP, or other subjects who were excluded, were not included in the compilation of total AEs. At post-season, the AKPS questionnaire was re-administered to all subjects. Athletes with a positive score on the AKPS and all athletes who had been examined preseason underwent further evaluation with a standardized personal interview and physical examination by the same physician. These data were compiled to calculate preseason prevalence and in season injury incidence of PFP.(Knowles et al., 2006)
Subjects were excluded from this study if they had tenderness at the tibial tuberosity (Osgood Schlatter's disease), midsubstance patellar tendon (patellar tendonopathy) or the inferior pole of the patella (Sinding-Larsen-Johansson disease), at either pre- (n=24) or post- (n=4) season assessment. Subjects were also excluded if they had a current knee ligament injury, prior knee surgery, recent knee trauma/contusion, and/or lower extremity stress fracture, or if they did not complete all pre-season biomechanical or strength testing (n=21). Subjects who were diagnosed with pre-season PFP were used to calculate pre-season prevalence, but were excluded from the data analyses (n=39). Finally, seven subjects were lost to follow-up (3 quit team, 3 moved from school district and one subject was out due to unknown medical issues) for the post-season assessment, leaving a total of 131 athletes without PFP at baseline or during the season whom were designated as the comparison or control group (CTRL) in the current data analyses (Figure 1). A total of 14 subjects developed new PFP during the 2007 basketball season and were categorized as the investigational group.
Figure 1.
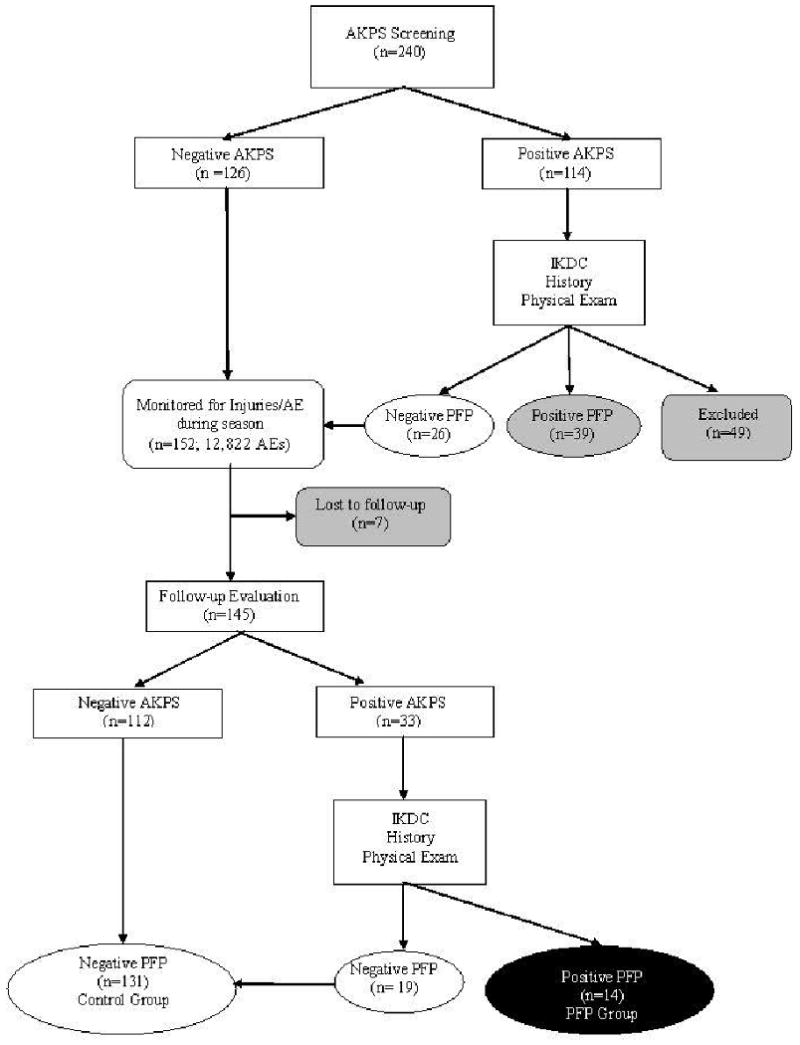
Flow chart of group identification for the referent CTRL and the PFP investigation categorization.
Statistics
Statistical means and standard deviations of all variables of interest were calculated from the three trials of the DVJ. A one-way between-groups multivariate analysis of variance was employed to investigate the group differences (CTRL vs PFP) on the dependent dynamic knee abduction variables. One way univariate ANOVA group testing was performed on the dependent static knee abduction alignment and vertical jump. The dominant limb of the CTRL group was compared to the involved limb (most symptomatic knee) of the PFP group. The non-dominant limb of the CTRL group was compared to the uninvolved limb (no symptoms or least symptomatic knee) of the PFP group.(Paterno et al., 2007) Statistical analyses were conducted in SPSS (SPSS, Version 17.0, Chicago; IL). Statistical significance was established a priori at p<0.05 to test the directional (one-sided) hypothesis that landing knee abduction load would be increased in athletes who would develop PFP.
Results
Table 1 presents the aggregate demographic and static anthropometrics that showed no inherent confounding between group effects for these measures (p>0.05). Vertical jump height performance measured during the DVJ, a measure of whole body power, was also not different between the PFP (30.1 ± 4.8 cm) and CTRL (31.8 ± 4.2 cm; p>0.05) study groups.
The point prevalence of unilateral PFP at the beginning of the season was 16.3 per 100 athletes. Prospective tracking of exposures in the middle and high school female basketball players resulted in 12,822 athlete exposures (9,109 practices; 3,713 games). The cumulative incidence risk and rate for the development of new unilateral PFP was 9.66 per 100 athletes and 1.09 per 1000 AEs, respectively. All new PFP developed in the middle school athletes who demonstrated a mean IKDC score of 85.6 ±7.7 at diagnosis.
Table 2 presents the mean knee abduction angle, moment and body mass normalized moment data measured during the drop vertical jump for each group. A one-way between-group multivariate analysis of variance was employed to investigate the group (new PFP vs CTRL) differences in dynamic knee abduction measures for the 12 dependent variables. There was a significant main effect of group membership between the new PFP and CTRL groups for the combined dependent variables (p=0.003) with a large effect size observed (partial eta squared =0.19). When evaluating the independent results for each of the dependent variables, distinct group differences were noted. Specifically, the analyses of dynamic landing mechanics indicated a significant group difference (95% CI: 0.32 to 4.62 Nm) indicative of increased knee abduction moment at initial contact in the new PFP (3.8 ± 4.2 Nm) involved limb relative to the matched CTRL limb (1.3 ± 4.7 Nm; p=0.03). This group difference of increased initial contact knee abduction load (95% CI: 0.002 to 0.084 Nm/kg) remained evident in the involved limb of new PFP subjects when moments were normalized to body mass (p = 0.04).
Table 2.
Mean (95% Confidence Interval) measurement for initial contact and peak during stance phase knee abduction kinematics and kinetics calculated during the drop vertical jump. *Significant (p<0.05) difference between PFP and CTRL groups.
| CTRL (n=131) | New PFP (n=14) | ||||||
|---|---|---|---|---|---|---|---|
| 95% Confidence Interval | 95% Confidence Interval | ||||||
| Mean | Lower | Upper | Unit | Mean | Lower | Upper | |
| Angle (IC) Involved | 1.4 | 0.8 | 1.9 | deg | 1.5 | 0.3 | 3.3 |
| Angle (IC) UnInvolved | 1.5 | 0.9 | 2.1 | deg | 1.7 | 0.1 | 3.6 |
| Angle (MAX) Involved | 8.3 | 7.1 | 9.5 | deg | 6.6 | 3.2 | 10.0 |
| Angle (MAX) UnInvolved | 8.8 | 7.6 | 9.9 | deg | 9.1 | 5.6 | 12.7 |
| Moment (IC) Involved* | 1.3 | 0.5 | 2.1 | Nm | 3.8 | 1.4 | 6.2 |
| Moment (IC) UnInvolved | 1.8 | 1.1 | 2.6 | Nm | 2.4 | 0.0 | 4.8 |
| Moment (MAX) Involved | 19.0 | 16.8 | 21.3 | Nm | 19.5 | 14.2 | 24.7 |
| Moment (MAX) UnInvolved* | 15.2 | 13.7 | 16.8 | Nm | 20.9 | 13.1 | 28.7 |
| Normalized Moment (IC) Involved* | 0.024 | 0.011 | 0.036 | Nm/kg | 0.067 | 0.028 | 0.106 |
| Normalized Moment (IC) UnInvolved | 0.034 | 0.022 | 0.045 | Nm/kg | 0.043 | 0.008 | 0.078 |
| Normalized Moment (MAX) Involved | 0.342 | 0.313 | 0.370 | Nm/kg | 0.389 | 0.301 | 0.477 |
| Normalized Moment (MAX) UnInvolved* | 0.278 | 0.256 | 0.300 | Nm/kg | 0.364 | 0.296 | 0.432 |
IC = Knee abduction moment measured at initial contact
MAX = Peak knee abduction moment
Nm = Newton*meter
With regard to loading of the uninvolved limb, the new PFP group also employed landing strategies that involved increased knee abduction loading. The maximum landing knee abduction load was increased (95% CI: 1.3 to 10.1 Nm; p=0.02) in the new PFP group who landed with 20.9 ± 13.6 Nm of maximum knee abduction load, compared to the CTRL landed who landed with only 15.2 ± 9.0 Nm of maximum knee abduction moment. The significant increase (95% CI: 0.014 to 0.157 Nm/kg) in maximum knee abduction load in the new PFP group uninvolved limb continued to be observed when moments were normalized to body mass (p=0.02).
Discussion
Patellofemoral pain (PFP) is one of the most common disorders of the lower extremity, with its greatest incidence in young, physically active female athletes. (Heintjes et al., 2005, Louden et al., 2004, Natri et al., 1998, Witvrouw et al., 2000, Kannus et al., 1987) PFP limits participation in recreational and sports activities and, more importantly, may be a precursor to long term patellofemoral osteoarthritis.(Natri et al., 1998, Utting et al., 2005, Witvrouw et al., 2000) The point prevalence of active symptomatic PFP at the beginning of the season for the current sample was 16.3 per 100 athletes. The cumulative incidence risk and rate for the development of new unilateral PFP was 9.66 per 100 athletes and 1.09 per 1000 athlete-exposures, respectively. The incidence is nearly identical to the 10% reported in a study of older (18.6 yrs; range, 17 to 21) students.(Witvrouw et al., 2000) However, if the subjects identified with preseason PFP were included in the analyses, the current sample point prevalence estimate would have increased to 22.0 per 100 athletes, a further indication of the need of pre-season screening to identify and minimize the effect of predisposing risk factors of PFP in athletes, particularly young females.
As indicated previously, prior biomechanical analyses have been beneficial to aid in the determination of altered neuromuscular strategies in patients with symptomatic PFP. However, the retrospective nature of these studies has limited the ability to determine if the suggested pathomechanics contribute to the development of PFP or if they result as sequelae of the disorder in its natural course. The purpose of this study was to prospectively evaluate measures of frontal plane knee loading during landing to determine their relationship to development of PFP. It was hypothesized that increased dynamic knee abduction load would be associated with development of new PFP in female basketball players compared to teammates without PFP (CTRL) at baseline. We observed that athletes who developed PFP during the season demonstrated increased knee abduction moment at initial contact on the most-symptomatic limb compared to their teammates without PFP. In addition, those with new PFP also demonstrate increased maximum knee abduction load in the least-symptomatic limb relative to the matched control limbs during the drop vertical jump. Interestingly, this increased dynamic knee abduction load during landing in the PFP group remained increased when the frontal plane moments were normalized to body mass. Thus, the current study results supported the hypothesis that dynamic knee abduction loading during landing activities contributes to the onset of PFP during a competitive sport season.
Female athletes exhibit increased lower extremity knee abduction alignment and load compared to males during drop landing and pivoting movements and also demonstrate increased incidence of both acute and chronic knee injury such as PFP.(Ford et al., 2003, Ford et al., 2005) These similar impaired biomechanics and neuromuscular control are probable links to the pathomechanics of PFP in young female athletes.(Powers, 2003, Hewett et al., 2005) Our prospective finding of increased initial contact and maximum knee abduction load, also observed when the frontal plane load was normalized to body mass in the PFP group's landing mechanics, suggests this potential etiological relationship. In contrast to our findings, Stefanyshyn and colleagues reported an increased external knee adduction moment during single support stance phase running in prospectively measured subjects who developed PFP.(Stefanyshyn et al., 2006) Their study reported that altered mechanics in the frontal plane were related to PFP onset in runners, albeit with external loads directed in opposite (adduction moment) direction to the knee loads identified for causality in the current report. The differences in task performance during (single leg stance during running vs bilateral landing task) are likely related to the observed differences between their report and our findings.(Stefanyshyn et al., 2006) The literature on altered proprioception and neuromuscular control in patients with PFP is sparse. Baker and colleagues found that individuals with PFP had an abnormal joint position sense.(Baker et al., 2002) However, these deficits were observed in patients with symptomatic PFP, which limits the ability to determine if the deficits precede or follow the onset of PFP. Cumulatively, the data from prior and the current investigations indicate that “out of plane” frontal plane knee loads (external knee adduction in runners, external knee abduction in athletes in cutting and landing sports) that disrupt normal sagittal plane tibiofemoral mechanics, may ultimately disrupt the normal patellofemoral mechanics that contribute to the etiology of PFP.
Witvrouw and colleagues reported that decreased vertical jump was related to PFP onset in a cohort of male and female students enrolled in physical education courses. (Witvrouw et al., 2000) These authors hypothesized that the decreased explosive power may have led to a reduction in muscular capacity to adequately absorb force during deceleration and/or landing activities. The reduced ability to dissipate forces may have been an underlying intrinsic factor which increased patellofemoral stresses and predisposition to PFP. (Witvrouw et al., 2000) The absence of observed group differences in our power measures and the concomitant increased frontal plane knee loading mechanics in PFP subjects may indicate that recruitment and neuromuscular control just prior to closed chain dynamic loading (opposed to absolute strength and power) may be important underlying neuromuscular correlates to PFP onset. Increased lower limb lever length without complementary hip strength and control has been proposed as an underlying mechanism for increased frontal plane knee motion and load in young female athletes as they mature.(Myer et al., 2008b, Hewett et al., 2004) Padua et al. examined the relationship between hip strength, quantified with a hand-held dynamometer, and joint kinematics, during a drop jump task in males and females. They reported that decreased hip strength (gluteus medius and gluteus maximus) was related to increased knee abduction alignment at initial contact and maximum measurement.(Padua et al., 2005) In a longitudinal study of 11 to 22 year old athletes, Brent and colleagues found that males demonstrated increased relative hip abduction strength when compared with females.(Brent et al., 2008) Thus, clinical focus on muscular performance and hip motor control strategies to decrease dynamic valgus postures and knee abduction loads may decrease abnormal patellofemoral loading mechanics during sports maneuvers.(Myer et al., 2005, Myer et al., 2007, Myer et al., 2004, Myer et al., 2006, Padua et al., 2005, Myer et al., 2008a)
Pilot work that evaluated trunk and hip focused neuromuscular training has shown to increase standing hip abduction strength in female athletes.(Myer et al., 2008a) This type of training, which focused on increasing hip abduction strength and recruitment, may improve the ability of female athletes to better control their increased height of center of mass and improve lower extremity alignments during initial contact to reduce loads which may contribute to the PFP onset. Accordingly, Labella et al. recently instituted a similar preseason neuromuscular training protocol to young female athletes (14.9 years) and found a reduced prevalence of knee pain at post-season follow-up.(Labella et al., 2008)
In the non-operative management of PFP, sports medicine practitioners traditionally have based their clinical assessments on static measures such as patellar alignment, patellar excursion, and patellar compression tests.(Fredericson and Yoon, 2006) Interestingly, only dynamic knee abduction measures, not static knee abduction angles, were related to the incidence of PFP in the current investigation. In a prospective study of adolescent students, Witvrouw and colleagues reported that hypermobile patella predicated PFP incidence. Conversely, MacIntyre and associates found that overall patella motion was not related to PFP.(MacIntyre et al., 2006) In a prospective study of high school female cross-country runners, Rauh and colleagues reported that runners with Q-angle measures of 20 or more degrees were more likely to injure their knee.(Rauh et al., 2007) However, recent literature does not report strong correlations between these static measures to dynamic alignments or the onset of PFP in young athletes involved in dynamic activities.(Post et al., 2002, Myer et al., 2010)
Limitations
PFP in female athletes likely has a multi-factorial etiology. Prior epidemiologic data indicates that altered muscular activation or other intrinsic factors (such as anatomical, hormonal and potentially psychological parameters) may contribute to PFP onset(Witvrouw et al., 2000) and were not controlled or investigated in the current analyses. Future investigations with larger sample sizes should aim to develop more robust PFP prediction models which include other potential contributing parameters (e.g. sport, training error, hormonal measures and potentially psychological parameters) to further elucidate risk factors for this disorder.
Another limitation to consider is that the current analyses were limited to the accuracy of the clinical diagnoses of PFP. While inter-rater error was controlled for by using one trained physician to perform all assessments, the complexity of this chronic disorder may create more diagnostic uncertainty relative to other acute knee injuries such as ACL tear. Continued efforts to accurately classify PFP into distinct injuries may allow for a better understanding of exact etiologies contributing to the onset of this syndrome.
Finally, one should consider that significant differences in knee abduction moments were measured at initial contact, where the magnitude of these measures are relatively small and with respect to relatively high intra-subject variability. Thus, while the reported differences were statistically significant, the clinical significance of these values should be further investigated. Nevertheless, PFP is a chronic disorder and it may be that the reported pathomechanics, while small in effect size, when compounded over an extended basketball season may actually provide a strong contribution to PFP onset. In addition, the increased maximum knee abduction reported in the PFP group further supports the underlying tendency between knee abduction mechanics, measured at initial contact or maximum, and development of PFP.
Conclusion
Nearly a quarter of the athletes were affected with PFP in the current sample at any cross section of the competitive season. These data provide an indication of the relevance of identification and amelioration of potential predisposing risk factors to prevent this syndrome that affects a large percentage of young female athletes. The relationship of increased knee abduction moment to PFP indicates that further examination of these potential biomechanical and neuromuscular correlates to delineate the pathomechanics of PFP is warranted. Interestingly, all of the new PFP occurrences occurred in the younger middle school aged female basketball players, which indicates that implementing trunk and hip strength neuromuscular training at an earlier age may help to minimize lower extremity pathomechanics, and thereby reduce the risk and occurrence of PFP before these athletes participate in sports in higher school levels.
Figure 2.
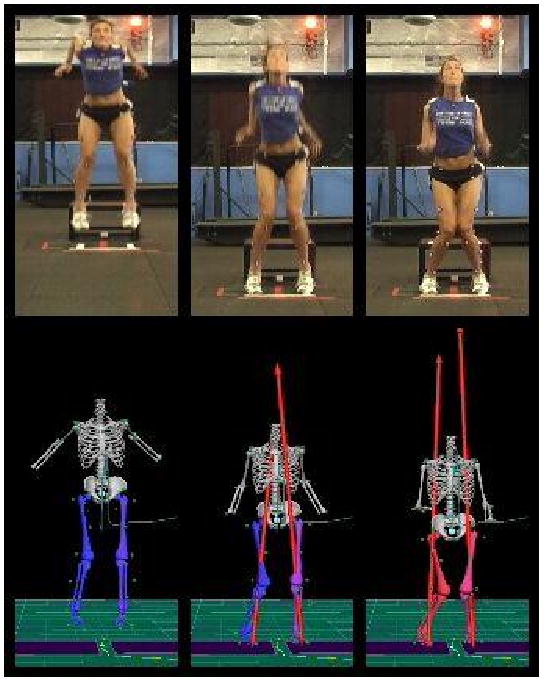
Pictorial and biomechanical depiction of athlete with high initial contact and maximum knee abduction load during the landing phase of a drop vertical jump.
Acknowledgments
The authors would like to acknowledge funding support from National Institutes of Health Grant R01-AR049735, R01-AR055563 and R01-AR056259. We would also like to thank Randy Poe, Ed Massey and Mike Blevins and the Boone County public school board and the entire Boone County school district for their participation in this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baker V, Bennell K, Stillman B, Cowan S, Crossley K. Abnormal knee joint position sense in individuals with patellofemoral pain syndrome. J Orthop Res. 2002;20:208–14. doi: 10.1016/S0736-0266(01)00106-1. [DOI] [PubMed] [Google Scholar]
- Blond L, Hansen L. Patellofemoral pain syndrome in athletes: a 5.7-year retrospective follow-up study of 250 athletes. Acta Orthop Belg. 1998;64:393–400. [PubMed] [Google Scholar]
- Bloomfield J, Polman R, O'Donoghue P, Mcnaughton L. Effective speed and agility conditioning methodology for random intermittent dynamic type sports. J Strength Cond Res. 2007;21:1093–100. doi: 10.1519/R-20015.1. [DOI] [PubMed] [Google Scholar]
- Bolgla LA, Malone TR, Umberger BR, Uhl TL. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38:12–8. doi: 10.2519/jospt.2008.2462. [DOI] [PubMed] [Google Scholar]
- Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, BEUTLER A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37:2108–16. doi: 10.1177/0363546509337934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent JL, Myer GD, Ford KR, Hewett TE. A Longitudinal Examination of Hip Abduction Strength in Adolescent Males and Females. Medicine and Science in Sports and Exercise. 2008;39 [Google Scholar]
- Cahue S, Dunlop D, Hayes K, Song J, Torres L, Sharma L. Varus-valgus alignment in the progression of patellofemoral osteoarthritis. Arthritis Rheum. 2004;50:2184–90. doi: 10.1002/art.20348. [DOI] [PubMed] [Google Scholar]
- CDC CFDC. Healthy Youth. National Center for Chronic Disease Prevention and Health Promotion. 2006 http://www.cdc.gov/HealthyYouth/physicalactivity.
- Christou EA. Patellar taping increases vastus medialis oblique activity in the presence of patellofemoral pain. J Electromyogr Kinesiol. 2004;14:495–504. doi: 10.1016/j.jelekin.2003.10.007. [DOI] [PubMed] [Google Scholar]
- Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004;85:815–22. doi: 10.1016/s0003-9993(03)00613-0. [DOI] [PubMed] [Google Scholar]
- Crossley KM, Cowan SM, Mcconnell J, Bennell KL. Physical therapy improves knee flexion during stair ambulation in patellofemoral pain. Med Sci Sports Exerc. 2005;37:176–83. doi: 10.1249/01.mss.0000152676.13197.49. [DOI] [PubMed] [Google Scholar]
- Fairbank JC, Pynsent PB, Van Poortvliet JA, Phillips H. Mechanical factors in the incidence of knee pain in adolescents and young adults. J Bone Joint Surg Br. 1984;66:685–93. doi: 10.1302/0301-620X.66B5.6501361. [DOI] [PubMed] [Google Scholar]
- Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35:1745–50. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- Ford KR, Myer GD, Hewett TE. Reliability of landing 3D motion analysis: implications for longitudinal analyses. Med Sci Sports Exerc. 2007;39:2021–8. doi: 10.1249/mss.0b013e318149332d. [DOI] [PubMed] [Google Scholar]
- Ford KR, Myer GD, Hewett TE. Longitudinal effects of maturation on lower extremity joint stiffness in female and male athletes. Am J Sports Med. 2010 doi: 10.1177/0363546510367425. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford KR, Myer GD, Toms HE, Hewett TE. Gender differences in the kinematics of unanticipated cutting in young athletes. Medicine & Science in Sports. 2005;37:124–9. [PubMed] [Google Scholar]
- Fredericson M, Yoon K. Physical examination and patellofemoral pain syndrome. Am J Phys Med Rehabil. 2006;85:234–43. doi: 10.1097/01.phm.0000200390.67408.f0. [DOI] [PubMed] [Google Scholar]
- Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30:447–56. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- Fulkerson JP, Arendt EA. Anterior knee pain in females. Clin Orthop Relat Res. 2000:69–73. doi: 10.1097/00003086-200003000-00009. [DOI] [PubMed] [Google Scholar]
- Heintjes E, Berger M, Bierma-Zeinstra S, Bernsen R, Verhaar J, Koes B. Exercise therapy for patellofemoral pain syndrome. Hobken, NJ: John Wiley & Sons, Ltd; 2005. [DOI] [PubMed] [Google Scholar]
- Hewett TE, Myer GD, Ford KR. Decrease in neuromuscular control about the knee with maturation in female athletes. J Bone Joint Surg Am. 2004;86-A:1601–1608. doi: 10.2106/00004623-200408000-00001. [DOI] [PubMed] [Google Scholar]
- Hewett TE, Myer GD, Ford KR, Heidt RS, Jr, Colosimo AJ, Mclean SG, Van Den Bogert AJ, Paterno MV, Succop P. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. Am J Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- Huberti HH, Hayes WC. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984;66:715–24. [PubMed] [Google Scholar]
- Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600–13. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- Kannus P, Aho H, Jarvinen M, Niittymaki S. Computerized recording of visits to an outpatient sports clinic. Am J Sports Med. 1987;15:79–85. doi: 10.1177/036354658701500112. [DOI] [PubMed] [Google Scholar]
- Knowles SB, Marshall SW, Guskiewicz KM. Issues in estimating risks and rates in sports injury research. J Athl Train. 2006;41:207–15. [PMC free article] [PubMed] [Google Scholar]
- Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–63. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- Labella CR, Huxford MR, Smith TL, Cartland J. Preseason Neuromuscular Exercise Program Reduces Sports-Related Knee Pain in Female Adolescent Athletes. Clin Pediatr (Phila) 2008 doi: 10.1177/0009922808323903. [DOI] [PubMed] [Google Scholar]
- Louden JK, Gajewski B, Goist-Foley HL, Louden KL. The effectiveness of exercise in treating patellofemoral-pain syndrome. J of Sport Rehab. 2004;13:323–342. [Google Scholar]
- Macintyre NJ, Hill NA, Fellows RA, Ellis RE, Wilson DR. Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome. J Bone Joint Surg Am. 2006;88:2596–605. doi: 10.2106/JBJS.E.00674. [DOI] [PubMed] [Google Scholar]
- Myer GD, Brent JL, Ford KR, Hewett TE. A pilot study to determine the effect of trunk and hip focused neuromuscular training on hip and knee isokinetic strength. Br J Sports Med. 2008a;42:614–9. doi: 10.1136/bjsm.2007.046086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myer GD, Chu DA, Brent JL, Hewett TE. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin Sports Med. 2008b;27:425–48. ix. doi: 10.1016/j.csm.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:1–7. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myer GD, Ford KR, Hewett TE. Rationale and Clinical Techniques for Anterior Cruciate Ligament Injury Prevention Among Female Athletes. J Athl Train. 2004;39:352–364. [PMC free article] [PubMed] [Google Scholar]
- Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med. 2010 doi: 10.1136/bjsm.2009.069351. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myer GD, Ford KR, Mclean SG, Hewett TE. The Effects of Plyometric Versus Dynamic Stabilization and Balance Training on Lower Extremity Biomechanics. Am J Sports Med. 2006;34:490–8. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- Natri A, Kannus P, Jarvinen M. Which factors predict the long-term outcome in chronic patellofemoral pain syndrome? A 7-yr prospective follow-up study. Med Sci Sports Exerc. 1998;30:1572–7. doi: 10.1097/00005768-199811000-00003. [DOI] [PubMed] [Google Scholar]
- Padua DA, Marshall SW, Beutler AI, Demaio M, Boden BP, Yu B, Garrett WE. Predictors of Knee Valgus Angle During a Jump-Landing Task. Med Sci Sports Exerc. 2005;37:S398. [Google Scholar]
- Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17:258–62. doi: 10.1097/JSM.0b013e31804c77ea. [DOI] [PubMed] [Google Scholar]
- Post WR, Teitge R, Amis A. Patellofemoral malalignment: looking beyond the viewbox. Clin Sports Med. 2002;21:521–46. x. doi: 10.1016/s0278-5919(02)00011-x. [DOI] [PubMed] [Google Scholar]
- Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33:639–46. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- Rauh MJ, Koepsell TD, Rivara FP, Rice SG, Margherita AJ. Quadriceps angle and risk of injury among high school cross-country runners. J Orthop Sports Phys Ther. 2007;37:725–33. doi: 10.2519/jospt.2007.2453. [DOI] [PubMed] [Google Scholar]
- Robinson RL, Nee RJ. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37:232–8. doi: 10.2519/jospt.2007.2439. [DOI] [PubMed] [Google Scholar]
- Stefanyshyn DJ, Stergiou P, Lun VM, Meeuwisse WH, Worobets JT. Knee angular impulse as a predictor of patellofemoral pain in runners. Am J Sports Med. 2006;34:1844–51. doi: 10.1177/0363546506288753. [DOI] [PubMed] [Google Scholar]
- Utting MR, Davies G, Newman JH. Is anterior knee pain a predisposing factor to patellofemoral osteoarthritis? Knee. 2005;12:362–5. doi: 10.1016/j.knee.2004.12.006. [DOI] [PubMed] [Google Scholar]
- Van Den Bogert AJ. Analysis and simulation of mechanical loads on the human musculoskeletal system: a methodological overview. Exerc Sport Sci Rev. 1994;22:23–51. [PubMed] [Google Scholar]
- Watson CJ, Propps M, Ratner J, Zeigler DL, Horton P, Smith SS. Reliability and responsiveness of the lower extremity functional scale and the anterior knee pain scale in patients with anterior knee pain. J Orthop Sports Phys Ther. 2005;35:136–46. doi: 10.2519/jospt.2005.35.3.136. [DOI] [PubMed] [Google Scholar]
- Willson JD, Binder-Macleod S, Davis IS. Lower extremity jumping mechanics of female athletes with and without patellofemoral pain before and after exertion. Am J Sports Med. 2008;36:1587–96. doi: 10.1177/0363546508315592. [DOI] [PubMed] [Google Scholar]
- Witvrouw E, Lysens R, Bellemans J, Cambier D, Vanderstraeten G. Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am J Sports Med. 2000;28:480–9. doi: 10.1177/03635465000280040701. [DOI] [PubMed] [Google Scholar]
- Woltring HJ, Huiskes R, De Lange A, Veldpaus FE. Finite centroid and helical axis estimation from noisy landmark measurements in the study of human joint kinematics. J Biomech. 1985;18:379–89. doi: 10.1016/0021-9290(85)90293-3. [DOI] [PubMed] [Google Scholar]


