Abstract
Background and objectives. Rates of dialysis withdrawal are higher among the elderly and lower among Blacks, yet it is unknown whether preferences for withdrawal and engagement in advance care planning also vary by age and race or ethnicity.
Design, setting, participants and methods. We recruited 61 participants from two dialysis clinics to complete questionnaires regarding dialysis withdrawal preferences in five different health states. Engagement in advance care planning (end-of-life discussions), completion of advance directives and ‘do not resuscitate’ or ‘do not intubate’ (DNR/DNI) orders were ascertained by a questionnaire and from dialysis unit records.
Results. The mean age was 62 ± 15 years; 38% were Black, 11% were Latino, 34% were White and 16% of participants were Asian. Blacks were less likely to prefer dialysis withdrawal as compared with Whites (odds ratio 0.16, 95% confidence interval 0.03–0.88) and other race/ethnicity groups, and this difference was not explained by age, education, comorbidity and other confounders. In contrast, older age was not associated with preferences for withdrawal. Rates of engagement in end-of-life discussions were higher than for documentation of advance care planning for all age and most race/ethnicity groups. Although younger participants and minorities were generally less likely to document treatment preferences as compared with older patients and Whites, they were not less likely to engage in end-of-life discussions.
Conclusions. Preferences for withdrawal vary by race/ ethnicity, whereas the pattern of engagement in advance care planning varies by age and race/ethnicity. Knowledge of these differences may be useful for improving communication about end-of-life preferences and in implementing effective advance care planning strategies among diverse haemodialysis patients.
Keywords: advance care planning, dialysis withdrawal, elderly, race, treatment preferences
Introduction
Nearly one in five patients with end-stage renal disease (ESRD) receiving dialysis withdraws from dialysis before death [1,2]. Clinical practice guidelines on the withdrawal of dialysis advocate for a shared decision-making process which takes into account individual treatment preferences along with prognostic information [3,4]. These treatment preferences can be communicated through an advance directive so that patient autonomy can be respected in the event a patient is unable to communicate his or her wishes. However, despite recognition of the need for better communication about treatment goals, only 13–35% of ESRD patients complete advance directives [5–7]. The result is that the burden of decision making is often placed on surrogates whose substituted judgements are only weakly correlated with a patient's own preferences [8].
Nationally, rates of dialysis withdrawal vary substantially by age and race. Those over the age of 75 are three times more likely to withdraw from dialysis compared with those of ages 45–59, whereas Black patients are half as likely to withdraw from dialysis compared with White or Asian patients [1,2]. These variations are presumed to reflect differences in treatment preferences. Differences in engagement in advance care planning could also account for this variation, yet no studies in ESRD patients have addressed these issues.
Traditional models of advance care planning have focused on documentation of treatment goals, and discussions of treatment preferences between patients and clinicians were viewed as promoting this goal. In support of this type of advance care planning model, studies have shown that provision of written materials about advance directives increase advance directive completion rates [5,9]. Nevertheless, this model may work less well for patients with language, social or cultural barriers hindering completion of an advanced directive, or for younger patients who may not perceive the need to complete advance directives as imminent, and this has led some to propose patient-centred approaches that do not focus solely on documentation as the end point of advance care planning [10–12]. While age and race differences in documentation of advance directives have been previously noted, few studies have evaluated other aspects of advance care planning, such as end-of-life discussions, among ESRD patients.
We studied a diverse population of ESRD patients on haemodialysis to characterize patient preferences for dialysis withdrawal and engagement in advance care planning. We hypothesized that younger patients and minorities would be less likely to prefer dialysis withdrawal, and less likely to engage in multiple aspects of advance care planning including end-of-life discussions, completion of advance directives and completion of ‘do not resuscitate’ (DNR) or ‘do not intubate’ (DNI) orders.
Methods
Participants
From April 2007 to February 2008, we recruited participants from the University of California San Francisco Mt. Zion Hemodialysis Center and the San Francisco Veterans Affairs Medical Center Hemodialysis Center, which together provide dialysis care for ∼150 patients. Potential participants were excluded if they were not fluent in English or if they had an active psychiatric disorder such as schizophrenia, dementia or a learning disability (∼23% of the clinic patients were excluded). The Committees on Human Research at UCSF and the San Francisco Veterans Affairs Medical Center approved the study, and all participants signed informed consent.
Measures
Enrolled participants completed a study questionnaire that assessed demographic, clinical and psychosocial characteristics. Participation in an end-of-life discussion was ascertained by two questionnaire items: ‘Did your doctor or nurse ever discuss with you … how you feel about the use of machines and other medical treatments to prolong your life when there is no chance of you getting better?’ and ‘… whether you want to be resuscitated if you stopped breathing?’ [13]. An affirmative response to either question was used to indicate participation in an end-of-life discussion. The presence of an advance directive and of a DNR/DNI order was ascertained by the review of the medical record.
To assess preferences for dialysis withdrawal, we used a modified version of the Dialysis Living Will [14]. Participants were asked to rate their likelihood of dialysis withdrawal in five different health states: current health, moderate stroke resulting in wheelchair dependency, dementia, terminal cancer and coma. Participants rated treatment preferences in each state as definitely continue dialysis, probably continue dialysis, probably stop dialysis or definitely stop dialysis. Preference for dialysis withdrawal for each health state was defined as a response of ‘probably withdraw’ or ‘definitely withdraw’.
Covariates
Demographic and psychosocial characteristics such as age, sex, race (White, Black, Asian), ethnicity, education (categorized as some high school, high school graduate or college education), household income (<$20 000/year, $20 000–$50 000/year, >$50 000/year) and living arrangements (alone, with family or friends, or in a skilled nursing facility) were ascertained by a questionnaire. We used the Illness Effects Questionnaire (IEQ) to assess perceived burden of illness [15]. Scores on the IEQ range from 20 to 140, higher scores indicate higher illness burden. Depressive symptoms were ascertained using the Geriatric Depression Scale (GDS) short form [16]. A score of 6 or greater on the GDS was defined as having depressive symptoms. Global quality of life was ascertained with the Satisfaction with Life Scale (SWLS) [17]. Scores range from 5 to 35; higher scores indicate higher quality of life. Faith and spirituality was assessed with a questionnaire item ascertaining the importance of faith or spiritual beliefs in the participant's life. Length of time on dialysis and comorbidity were assessed by the chart review, and a Charlson comorbidity index score was calculated for each participant [18].
Analysis
Characteristics of the cohort were compared by age and by race/ethnicity using analysis of variance or Fisher's exact test, as appropriate. We compared treatment preferences for each health state by age and race/ethnicity groups using Fisher's exact test. Age was categorized as <50, 50–75 and >75 years of age. Since there were no non-White Latino participants, self-report of race and ethnicity was categorized as Black, Latino White (hereafter Latino), non-Latino White (hereafter White) or Asian. We evaluated whether clinical and psychosocial characteristics accounted for age and race/ethnicity differences in treatment preferences using logistic regression. For these analyses, we defined preference for withdrawal as a response of ‘probably withdraw’ or ‘definitely withdraw’ in at least one of the five health states queried. We first determined the unadjusted association, expressed as an odds ratio (OR) and 95% confidence interval (95% CI), for each of the clinical and psychosocial variables age, race/ethnicity, education, years on dialysis, Charlson index, IEQ score, SWLS score, depressive symptoms and faith or spirituality with treatment preference. We then developed a parsimonious multivariable adjusted model that included age, race/ethnicity, education and other clinical or psychosocial variables significant at the P < 0.1 level to determine whether multivariable adjustment attenuated the association between age, race/ethnicity and treatment preference.
We compared the proportion of patients engaging in the various aspects of advance care planning: end-of-life discussions, completion of advance directives and completion of a DNR/DNI order by age and race/ethnicity using Fisher's exact test. Similar to the models constructed for treatment preferences, we determined the association of age, race/ethnicity, education, years on dialysis, Charlson index, IEQ score, SWLS score, depressive symptoms and faith or spirituality with each aspect of advance care planning in an unadjusted and parsimonious multivariable adjusted model. Based on the previous literature, we also evaluated end-of-life discussions as a potential predictor in the models of advance directive completion. Because there were so few patients who completed DNR/DNI orders, we were not able to obtain stable point estimates for this outcome in the logistic models. All analyses were performed with SAS v9.1 (Cary, NC, USA).
Results
Participant characteristics
Sixty-two participants were enrolled in the study. One participant did not complete the study questionnaire and was excluded from analysis. The mean age was 62 ± 15 years, the mean length of time on dialysis was 4 ± 3 years and the mean IEQ score was 74 ± 25, indicating moderate illness burden, comparable with previous studies in ESRD patients [15]. Eighteen percent (n = 11) were <50 years of age, 61% (n = 37) were 50–75 years of age and 21% of participants (n = 13) were >75 years of age. Thirty-eight percent (n = 23) were Black, 11% (n = 7) were Latino, 34% (n = 21) were White and 16% (n = 10) of participants were Asian. There were significant differences in education and faith/spirituality by race/ethnicity groups (Table 1). There was a trend towards higher comorbidity among older patients (P = 0.06), but no differences in any other participant characteristics by age (data not shown).
Table 1.
Demographic and clinical characteristics of haemodialysis participants in the San Francisco completing survey (N = 61)
| P-value for | ||||||
|---|---|---|---|---|---|---|
| All subjects | Black | Latino | White | Asian | comparison across | |
| (N = 61) | (N = 23) | (N = 7) | (N = 21) | (N = 10) | race/ ethnicity groups | |
| Mean ± standard deviation | ||||||
| Age (years) | 62 ± 15 | 62 ±13 | 51 ± 19 | 67 ± 14 | 58 ± 18 | 0.1 |
| Years on dialysis | 4 ± 3 | 4 ± 4 | 4 ± 2 | 4 ± 2 | 4 ± 3 | 0.9 |
| Charlson comorbidity indexa | 3 ± 2 | 3 ± 2 | 2 ± 1 | 3 ± 2 | 4 ± 2 | 0.2 |
| Illness effects questionnairea | 74 ± 25 | 71 ± 30 | 80 ± 28 | 77 ± 23 | 70 ± 14 | 0.7 |
| Satisfaction with life scalea | 17 ± 7 | 16 ± 7 | 21 ± 8 | 15 ± 6 | 17 ± 7 | 0.2 |
| Frequency (N) | ||||||
| Men % (N) | 74 (45) | 70 (16) | 100 (7) | 76 (16) | 60 (6) | 0.3 |
| Diabetes % (N) | 48 (29) | 43 (10) | 29 (2) | 52 (11) | 60 (6) | 0.6 |
| Living arrangements % (N) | 0.6 | |||||
| Alone | 34 (21) | 43 (10) | 43 (3) | 28 (6) | 20 (2) | |
| With family/friends | 59 (36) | 52 (12) | 57 (4) | 57 (12) | 80 (8) | |
| Nursing facility | 7 (4) | 4 (1) | 0 (0) | 14 (3) | 0 (0) | |
| Education % (N) | 0.02 | |||||
| Less than high school | 16 (10) | 35 (8) | 14 (1) | 0 (0) | 10 (1) | |
| High school graduate | 25 (15) | 26 (6) | 14 (1) | 19 (4) | 40 (4) | |
| College education | 59 (36) | 39 (9) | 71 (5) | 81 (17) | 50 (5) | |
| Faith or spiritual beliefs importanta % (N) | 68 (40) | 87 (20) | 57 (4) | 45 (9) | 78 (7) | 0.02 |
| Depressive symptoms % (N) | 48 (29) | 43 (10) | 71 (5) | 48 (10) | 40 (4) | 0.6 |
aData on 59 participants available.
Treatment preferences
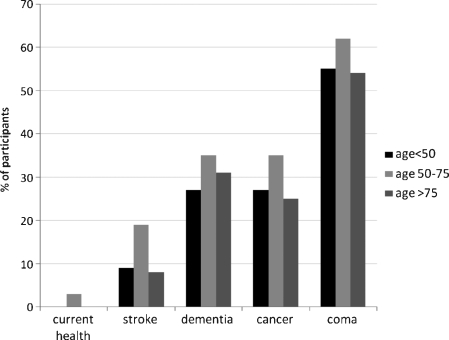
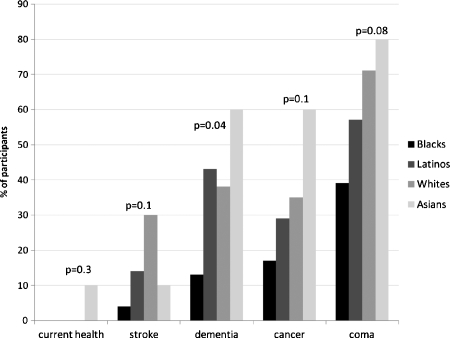
Overall, 2% of participants (n = 1) would probably or definitely withdraw in their current state of health, 15% in the event of moderate stroke, 33% in the event of dementia, 32% in the event of terminal cancer and 59% in the event of coma. Age was not associated with preference for withdrawal in any of the five health states (Figure 1). In contrast, there were significant or borderline significant associations between race and preference for withdrawal, with Blacks being less likely to prefer withdrawal in all health states, and Asians being more likely to prefer withdrawal in all health states except stroke (Figure 2).
Fig. 1.
Proportion of participants (N = 61) who would probably or definitely withdraw from dialysis in different health states, by age group. P-values for comparison across age groups are not significant for all health states. N = 11 for <50 years of age, N = 37 for 50–75 years of age and N = 13 for >75 years of age.
Fig. 2.
Proportion of participants (N = 61) who would probably or definitely withdraw from dialysis in different health states, by race/ethnicity. P-values are for comparison across race/ethnicity groups. N = 23 for Blacks, N = 7 for Latinos, N = 21 for Whites and N = 10 for Asians.
In unadjusted analyses, only the Charlson comorbidity index in addition to Black race was significantly associated with a preference for withdrawal in at least one of the five health states (Table 2). There was no significant association between age, male sex, years on dialysis, illness burden, quality of life, education, depressive symptoms or faith/spirituality with preferences. In a parsimonious model adjusted for age, education and Charlson comorbidity index, Black race remained strongly associated with a reduced likelihood of preferring dialysis withdrawal in at least one health state compared with Whites. After adjustment, Latino and Asian race/ethnicity was associated with a reduced likelihood of preferring withdrawal relative to Whites, but this was not statistically significant. The Charlson comorbidity index also remained independently associated with preference for withdrawal; each 1 point increase in comorbidity was associated with a 60% increased odds for preferring withdrawal (OR 1.60, 95% CI 1.04–2.47).
Table 2.
Association of demographic and clinical characteristics with preference for dialysis withdrawal in at least one health state (current health, stroke, dementia, terminal cancer or coma)
| Unadjusted odds ratio | Adjusteda odds ratio | |
|---|---|---|
| Characteristic | (95% confidence interval) | (95% confidence interval) |
| Age (per decade) | 0.97 (0.70–1.37) | 0.76 (0.47–1.22) |
| Race/ethnicity | ||
| White | Referent | Referent |
| Black | 0.26 (0.07–0.91) | 0.16 (0.13–0.85) |
| Latino | 0.53 (0.09–3.14) | 0.53 (0.07–3.80) |
| Asian | 1.60 (0.26–9.83) | 0.96 (0.13–7.35) |
| Male | 0.57 (0.17–1.91) | – |
| Years on dialysis | 0.91 (0.77–1.08) | – |
| Education | ||
| Less than high school | Referent | Referent |
| High school graduate | 1.50 (0.30–7.53) | 0.55 (0.08–3.88) |
| College education | 1.57 (0.38–6.43) | 0.65 (0.10–4.22) |
| Charlson comorbidity index | 1.40 (1.01–1.93) | 1.60 (1.04–2.47) |
| Illness effects questionnaire (per 10 points) | 0.85 (0.68–1.06) | – |
| Satisfaction with life scale (per 10 points) | 0.70 (0.32–1.50) | – |
| Faith or spiritual beliefs important | 0.56 (0.18–1.78) | – |
| Depressive symptoms | 0.74 (0.27–2.06) | – |
aModel adjusted for age, race, education and Charlson comorbidity index.
Advance care planning
Overall, 57% of participants reported having an end-of-life discussion with a health care provider, 38% had completed an advance directive and 10% had a DNR/DNI order in their dialysis chart. Among the individual aspects of advance care planning, there were significant differences in end-of-life discussions and DNR/DNI orders by race/ethnicity, with Blacks and Asians being more likely to engage in end-of-life discussions and Latinos less likely to engage in end-of-life discussions as compared with Whites (Table 3); conversely, no Black or Latino participants completed DNR/DNI orders as compared with 10% of Asians and 24% of Whites. There were trends for lower completion rates of advance directives and DNR/DNI orders among participants <50 years, but this did not reach statistical significance. These patterns remained similar after multivariable adjustment for age, race and education (Table 4). There was no association between male sex, years on dialysis, Charlson comorbidity index, illness burden, quality of life, depressive symptoms or faith/spirituality with participation in any aspect of advance care planning. There was a strong association between having an end-of-life discussion with a higher likelihood of completing an advanced directive that was of borderline significance after adjustment for other demographic characteristics (OR 4.38, 95% CI 0.97–19.89).
Table 3.
Proportion of participants engaging in steps of advance care planning by age and race/ethnicity groups (N = 61)
| End-of-life | Advance | ||
|---|---|---|---|
| discussion | directive | DNR/DNI | |
| Characteristic | % (N) | % (N) | order % (N) |
| Overall | 57 (35) | 38 (23) | 10 (6) |
| Age | |||
| <50 years (N = 11) | 64 (7) | 18 (2) | 0 (0) |
| 50–75 years (N = 37) | 57 (21) | 41 (15) | 11 (4) |
| >75 years (N = 13) | 54 (7) | 46 (6) | 15 (2) |
| P-value | 0.9 | 0.3 | 0.5 |
| Race | |||
| Black (N = 23) | 70 (16) | 30 (7) | 0 (0) |
| Latino (N = 7) | 29 (2) | 14 (1) | 0 (0) |
| White (N = 28) | 38 (8) | 43 (9) | 24 (5) |
| Asian (N = 10) | 90 (9) | 60 (6) | 10 (1) |
| P-value | 0.01 | 0.2 | 0.05 |
DNR/DNI—do not resuscitate or do not intubate.
Table 4.
Adjusted association of demographic and clinical characteristics with participation in advanced care planning
| Adjusted OR (95% CI) | ||
|---|---|---|
| End-of-life | Advanced directive | |
| Characteristic | discussion | completion |
| Age (per decade) | 0.86 (0.55–1.33) | 1.65 (1.00–2.72) |
| Race/ethnicity | ||
| White | Referent | Referent |
| Black | 2.20 (0.53–9.23) | 0.61 (0.11–3.42) |
| Latino | 0.42 (0.05–3.35) | 0.36 (0.03–4.44) |
| Asian | 11.32 (1.16–110.94) | 3.59 (0.46–27.74) |
| Education | ||
| Less than high school | Referent | Referent |
| High school graduate | 0.43 (0.05–3.60) | 0.39 (0.04–3.54) |
| College education | 0.25 (0.03–1.99) | 3.13 (0.44–22.44) |
| End-of-life discussion | – | 4.38 (0.97–19.89) |
Results are presented as odds ratio (OR) and 95% confidence intervals (95% CI). Models are adjusted for all covariates shown.
Discussion
In a diverse population of ESRD patients, age and race/ethnicity had distinct patterns of association with treatment preferences and with engagement in advance care planning. Black race was associated with a reduced likelihood of preferring dialysis withdrawal, whereas age was not associated with preferences for withdrawal. End-of-life discussions were more common than documentation of advance care planning and strongly associated with completion of an advanced directive. Contrary to our hypothesis, younger patients and minorities did not have lower rates of engagement in each of the various aspects of advance care planning; rather the specific pattern of engagement differed by age and race/ethnicity groups. This suggests that documentation of advance directives or DNR/DNI orders does not fully describe engagement in the advance care planning process, particularly for younger patients and minorities.
We found that preferences for dialysis withdrawal parallel national practice patterns of dialysis withdrawal with respect to race, but not age. This suggests that surrogate decision makers may be underestimating the preferences of elderly ESRD patients for aggressive care. In the current study, the majority of participants over the age of 75 preferred to continue dialysis in each of the health states described except for coma, and even for coma 45% preferred to continue dialysis. These findings are consistent with previous studies demonstrating that treatment preferences in seriously ill older adults vary widely, and studies in ESRD patients which found that older age was not associated with preference for CPR or dialysis withdrawal [8,19,20]. The tendency of surrogate decision makers to underestimate preferences for aggressive care among elderly patients has also been observed in other settings, including withholding of acute dialysis in hospitalized patients [21]. Potential explanations for this observation include substitution of a surrogate decision maker's values and preferences for the patient's own values and preferences. These findings also highlight the ethical dilemma faced by surrogate decision makers when confronted with withdrawal decisions where estimated prognosis conflicts with patient preferences; in such cases, formal ethical consultation may be required [3]. More research is also needed to determine whether patients understand the usual outcome of resuscitation efforts [22].
In contrast, preferences for dialysis withdrawal generally paralleled national practice patterns of dialysis withdrawal by race, that is, Blacks were much less likely to prefer dialysis withdrawal regardless of health status as compared with other race/ethnicity groups. Even in the case of irreversible coma, fewer than half of all Black participants preferred dialysis withdrawal, whereas 67–80% of White and Asian participants would prefer withdrawal. These findings are in contrast to the results of Pruchno et al., who found that Black race was associated with a spouse's substituted judgement regarding dialysis withdrawal, but not with patient preferences [8]. Although no previous studies have reported preferences among Latino or Asian ESRD patients in the USA, similar to our findings Miura et al. reported that 55–82% of ESRD patients in Japan would prefer dialysis withdrawal in the setting of terminal cancer and dementia, respectively. Consistent with previous studies in non-ESRD populations [23,24], these racial differences were unchanged after adjustment for comorbidity, illness burden, education, quality of life, depressive symptoms and faith or spiritual beliefs, suggesting that unmeasured cultural values may be responsible for these observations.
Completion rates of advance directives and DNR/DNI orders by age and race/ethnicity were similar to those in the general population [10,25]; however, evaluation of these rates in isolation would generally underestimate the frequency of engagement in the advance care planning process, and this was especially true for younger patients and minorities. For example, although they had low rates of advance directive completion, younger patients and Blacks were more likely (rather than less likely) to engage in end-of-life discussions with health care providers. There may be several reasons that end-of-life discussions did not translate into documentation of treatment goals in these groups, including a view of dialysis as life-sustaining therapy versus supportive therapy (particularly for patients awaiting transplantation), or reliance on family members rather than health care providers to carry out health care preferences. They may also not see a need to complete an advance directive if they do not want any treatment limitations. Alternatively, though perhaps less likely, younger patients and Blacks may have been more likely to recall having had an end-of-life discussion with a health care provider. For these reasons, written documentation may not be the appropriate outcome or quality indicator of the advance care planning process in all patients. Indeed, some qualitative studies have highlighted the importance of end-of-life discussions in strengthening relationships with loved ones, rather than documentation of treatment goals [12,26]. Additional studies are needed to determine whether a patient-centred model that is not exclusively focused on documentation of treatment goals, as has been recently described [11,26], may ultimately lead to improved end-of-life ESRD care.
A variety of instruments exist to measure participation in advance care planning and treatment preferences, and the choice of instruments used may have specific implications for interpretation. We used two questionnaire items to define an end-of-life discussion. These items have predictive validity based on their association with meaningful advance care planning outcomes in previous studies [13,27,28], a conclusion supported by our results demonstrating a 4-fold higher likelihood of completing an advanced directive among those with an end-of-life discussion defined by these items. Nevertheless, they may be subject to recall bias and they do not provide information about the extent of involvement in or the content of end-of-life discussions. Alternative methods for ascertaining participation in end-of-life discussions, such as through in-depth interviews, may provide complementary information. Similarly, the elicitation of treatment preferences may focus on interventions, health states or outcomes of treatment. We used the Dialysis Living Will since this is a widely used tool for measurement of end-of-life treatment preferences in ESRD patients [8,14,19]. We focused on dialysis withdrawal in five specific health states; thus, our findings may not apply to other life-sustaining interventions. Previous research has demonstrated that health states and expected outcomes influence decision making more than the specific interventions considered [14,29], and that among ESRD patients, continuation of dialysis is a surrogate for preferences for other life-sustaining interventions [14].
There are several limitations of this study. We only recruited English-speaking patients from two dialysis clinics from the west coast, and our study sample was small, particularly for the Asian and Latino race/ethnicity groups. Although our population is similar to other geographic regions in terms of age and diabetes, there may be other characteristics of the study population related to geographic areas that are not captured in these data. Thus, the results may not be generalizable to non-English-speaking patients or to patients in different geographic regions or rural centres. In addition, because this was a cross-sectional study, we were unable to link preferences or advance care planning practices to individual participant outcomes or subsequent decisions. Furthermore, we did not assess communication with family members or satisfaction with the advance care planning process, which would be potentially useful adjunctive measures of the success of advance care planning.
In summary, we found significant differences in treatment preferences by race/ethnicity as well as differences in engagement in advance care planning by age and race/ethnicity. Knowledge of these differences may be useful for improving communication about end-of-life preferences and in implementing effective advance care planning strategies among diverse ESRD patients.
Acknowledgments
This work is supported by grant P30-AG15272 for the Center for Aging in Diverse Communities (CADC) under the Resource Centers for Minority Aging Research program by the National Institute on Aging, the National Institute of Nursing Research, and the National Center on Minority Health and Health Disparities, a Paul B. Beeson Career Development Award in Aging (K23 AG028952 to MKT) from the National Institute of Aging, and KL2 RR024130 from the National Center for Research Resources.
Conflict of interest statement. None declared.
References
- 1.Kurella M, Kimmel PL, Young BS, et al. Suicide in the United States end-stage renal disease program. J Am Soc Nephrol. 2005;16:774–781. doi: 10.1681/ASN.2004070550. [DOI] [PubMed] [Google Scholar]
- 2.Port FK, Wolfe RA, Hawthorne VM, et al. Discontinuation of dialysis therapy as a cause of death. Am J Nephrol. 1989;9:145–149. doi: 10.1159/000167954. [DOI] [PubMed] [Google Scholar]
- 3.Galla JH The Renal Physicians Association and the American Society of Nephrology. Clinical practice guideline on shared decision-making in the appropriate initiation of and withdrawal from dialysis. J Am Soc Nephrol. 2000;11:1340–1342. doi: 10.1681/ASN.V1171340. [DOI] [PubMed] [Google Scholar]
- 4.Cohen LM, Germain MJ, Poppel DM. Practical considerations in dialysis withdrawal:‘to have that option is a blessing’. JAMA. 2003;289:2113–2119. doi: 10.1001/jama.289.16.2113. [DOI] [PubMed] [Google Scholar]
- 5.Holley JL, Nespor S, Rault R. The effects of providing chronic hemodialysis patients written material on advance directives. Am J Kidney Dis. 1993;22:413–418. doi: 10.1016/s0272-6386(12)70144-0. [DOI] [PubMed] [Google Scholar]
- 6.Holley JL, Stackiewicz L, Dacko C, et al. Factors influencing dialysis patients’ completion of advance directives. Am J Kidney Dis. 1997;30:356–360. doi: 10.1016/s0272-6386(97)90279-1. [DOI] [PubMed] [Google Scholar]
- 7.Sehgal AR, Weisheit C, Miura Y, et al. Advance directives and withdrawal of dialysis in the United States, Germany, and Japan. JAMA. 1996;276:1652–1656. [PubMed] [Google Scholar]
- 8.Pruchno RA, Lemay EP, Jr, Feild L, et al. Predictors of patient treatment preferences and spouse substituted judgments: the case of dialysis continuation. Med Decis Making. 2006;26:112–121. doi: 10.1177/0272989X06286482. [DOI] [PubMed] [Google Scholar]
- 9.Sudore RL, Schickedanz AD, Landefeld CS, et al. Engagement in multiple steps of the advance care planning process: a descriptive study of diverse older adults. J Am Geriatr Soc. 2008;56:1006–1013. doi: 10.1111/j.1532-5415.2008.01701.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson KS, Kuchibhatla M, Tulsky JA. What explains racial differences in the use of advance directives and attitudes toward hospice care? J Am Geriatr Soc. 2008;56:1953–1958. doi: 10.1111/j.1532-5415.2008.01919.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davison SN, Torgunrud C. The creation of an advance care planning process for patients with ESRD. Am J Kidney Dis. 2007;49:27–36. doi: 10.1053/j.ajkd.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 12.Singer PA, Martin DK, Lavery JV, et al. Reconceptualizing advance care planning from the patient's perspective. Arch Intern Med. 1998;158:879–884. doi: 10.1001/archinte.158.8.879. [DOI] [PubMed] [Google Scholar]
- 13.Wenger NS, Kanouse DE, Collins RL, et al. End-of-life discussions and preferences among persons with HIV. JAMA. 2001;285:2880–2887. doi: 10.1001/jama.285.22.2880. [DOI] [PubMed] [Google Scholar]
- 14.Singer PA, Thiel EC, Naylor CD, et al. Life-sustaining treatment preferences of hemodialysis patients: implications for advance directives. J Am Soc Nephrol. 1995;6:1410–1417. doi: 10.1681/ASN.V651410. [DOI] [PubMed] [Google Scholar]
- 15.Kimmel PL, Peterson RA, Weihs KL, et al. Psychosocial factors, behavioral compliance and survival in urban hemodialysis patients. Kidney Int. 1998;54:245–254. doi: 10.1046/j.1523-1755.1998.00989.x. [DOI] [PubMed] [Google Scholar]
- 16.Burke WJ, Roccaforte WH, Wengel SP. The short form of the Geriatric Depression Scale: a comparison with the 30-item form. J Geriatr Psychiatry Neurol. 1991;4:173–178. doi: 10.1177/089198879100400310. [DOI] [PubMed] [Google Scholar]
- 17.Kimmel PL, Emont SL, Newmann JM, et al. ESRD patient quality of life: symptoms, spiritual beliefs, psychosocial factors, and ethnicity. Am J Kidney Dis. 2003;42:713–721. doi: 10.1016/s0272-6386(03)00907-7. [DOI] [PubMed] [Google Scholar]
- 18.Beddhu S, Bruns FJ, Saul M, et al. A simple comorbidity scale predicts clinical outcomes and costs in dialysis patients. Am J Med. 2000;108:609–613. doi: 10.1016/s0002-9343(00)00371-5. [DOI] [PubMed] [Google Scholar]
- 19.Miura Y, Asai A, Nagata S, et al. Dialysis patients’ preferences regarding cardiopulmonary resuscitation and withdrawal of dialysis in Japan. Am J Kidney Dis. 2001;37:1216–1222. doi: 10.1053/ajkd.2001.24525. [DOI] [PubMed] [Google Scholar]
- 20.Tsevat J, Cook EF, Green ML, et al. Health values of the seriously ill. SUPPORT investigators. Ann Intern Med. 1995;122:514–520. doi: 10.7326/0003-4819-122-7-199504010-00007. [DOI] [PubMed] [Google Scholar]
- 21.Hamel MB, Teno JM, Goldman L, et al. SUPPORT Investigators. Patient age and decisions to withhold life-sustaining treatments from seriously ill, hospitalized adults. Study to understand prognoses and preferences for outcomes and risks of treatment. Ann Intern Med. 1999;130:116–125. doi: 10.7326/0003-4819-130-2-199901190-00005. [DOI] [PubMed] [Google Scholar]
- 22.Clarke DE, Goldstein MK, Raffin TA. Ethical dilemmas in the critically ill elderly. Clin Geriatr Med. 1994;10:91–101. [PubMed] [Google Scholar]
- 23.Mebane EW, Oman RF, Kroonen LT, et al. The influence of physician race, age, and gender on physician attitudes toward advance care directives and preferences for end-of-life decision-making. J Am Geriatr Soc. 1999;47:579–591. doi: 10.1111/j.1532-5415.1999.tb02573.x. [DOI] [PubMed] [Google Scholar]
- 24.Kwak J, Haley WE. Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontologist. 2005;45:634–641. doi: 10.1093/geront/45.5.634. [DOI] [PubMed] [Google Scholar]
- 25.Welch LC, Teno JM, Mor V. End-of-life care in black and white: race matters for medical care of dying patients and their families. J Am Geriatr Soc. 2005;53:1145–1153. doi: 10.1111/j.1532-5415.2005.53357.x. [DOI] [PubMed] [Google Scholar]
- 26.Davison SN, Simpson C. Hope and advance care planning in patients with end stage renal disease: qualitative interview study. BMJ. 2006;333:886. doi: 10.1136/bmj.38965.626250.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169:480–488. doi: 10.1001/archinternmed.2008.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fried TR, Bradley EH, Towle VR, et al. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346:1061–1066. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]