Abstract
Introduction:
Victims of the sudden infant death syndrome (SIDS) may have preexisting abnormalities in their arousal pathways, inhibiting the progression of subcortical activation (SCA) to full cortical arousal (CA). Approximately 60% of SIDS victims are male, and it has been suggested that male infants have delayed cortical maturation compared to females. We hypothesized that CA frequency would be lower and CA threshold would be higher in male infants during both active (AS) and quiet (QS) sleep.
Methods:
50 healthy term infants (21 male, 29 female) were studied with daytime polysomnography at 2–4 weeks and 2–3 months after birth. Arousal from sleep was induced using a pulsatile air-jet to the nostrils at increasing pressures.
Results:
At 2–4 weeks, arousability from AS was similar in males and females, however during QS, male infants required a lower stimulus to induce SCA and CA. This gender difference in arousal threshold was not observed at 2–3 months. CA frequencies were similar between genders during both sleep states at both ages, though overall, CA was more frequent in AS than in QS.
Conclusions:
This study demonstrated that at 2–4 weeks, male infants were easier to arouse than female infants during QS. There were no significant effects of gender on total arousability or SCA and CA frequencies at 2–3 months, the age of peak SIDS incidence. Thus, although male infants are at greater risk of SIDS than female infants, this difference is unlikely to be associated with gender differences in CA threshold or frequency.
Citation:
Richardson HL; Walker AM; Horne RSC. Sleeping like a baby—does gender influence infant arousability? SLEEP 2010;33(8):1055-1060.
Keywords: Infant, arousal, SIDS, sleep, gender
SUDDEN INFANT DEATH SYNDROME (SIDS) REMAINS A LEADING CAUSE OF INFANT MORTALITY IN DEVELOPED COUNTRIES, WITH AN INCREASING NUMBER of deaths attributed to SIDS over recent years.1,2 Although the exact causal mechanisms remain an enigma, it is commonly thought that the final event of SIDS involves failed or impaired arousal from sleep in response to a life-threatening cardiorespiratory challenge.3–5 In support of this proposal, postmortem examinations of SIDS victims have revealed pathological evidence that prolonged or intermittent hypoxia may have preceded death.6,7 In further support of the failed arousal hypothesis, other studies have identified abnormalities in the brainstem of SIDS victims. These include disturbances in cholinergic and serotonergic (5-HT) systems,8,9 as well as structural abnormalities in medullary nuclei associated with the central control of respiratory and circulatory defensive responses and sleep/wake states.10,11
The infant arousal response is considered to be hierarchical in nature, consisting of subcortical or “brainstem” responses such as heart rate, respiratory, and behavioral changes that occur without disturbing sleep integrity, and those which progress to cortical activation with or without a full awakening.12,13 Physiological evidence suggests that despite appearing normal and apparently well prior to their deaths, SIDS victims may have had a functional deficit in the arousal process that inhibited the progression of subcortical activation (SCA) to full cortical arousal (CA).14,15 Furthermore, as previously shown in healthy infants, exposure to the major risk factors for SIDS, prone sleeping and maternal smoking, modifies the progression of stimulus-induced arousal processes from SCA to CA.16,17 Possibly, an inhibited progression of SCA to CA may provide a marker of an infant at increased likelihood of succumbing to SIDS, envisaged by Filiano and Kinney in their triple risk model for SIDS as the “vulnerable infant.”18
Approximately 60% of SIDS victims are male, and this increased prevalence of SIDS in male infants has been demonstrated consistently throughout the world.2,19–22 Inherent gender differences have been identified in the medullae of SIDS victims, including increased apoptotic neuronal cell death and decreased 5-HT1A receptor binding in male infants that may lead to altered arousal pathways and increased vulnerability to SIDS.8,11 Maturation of the central nervous system and cortical function occurs more slowly in male infants23; but it remains uncertain whether there are specific gender differences in the arousal process. We hypothesized that CA responses would be impaired in male infants when compared with female infants, contributing to the increased risk of SIDS in males. To test this hypothesis we evaluated induced arousal responses from active (AS) and quiet (QS) sleep in male and female infants, with a focus on the progression from SCA to CA.
METHODS
Ethical approval for this project was obtained from the Southern Health and Monash University Human Research Ethics Committees. Participation was voluntary, with no monetary incentive provided. Written informed parental consent was obtained prior to study commencement.
Participants
A total of 50 healthy infants were studied at 2–4 weeks and 2–3 months postnatal age. As shown by the demographic information in Table 1, all male (n = 21) and female (n = 29) infants were born at term and were of similar birth weights. Subject inclusion criteria controlled for known SIDS risk factors in that none of the mothers smoked during pregnancy, infants were predominantly breast fed and were all routinely placed supine to sleep at home.
Table 1.
Infant demographics (mean ± SEM)
| Birth | 2–4 weeks | 2–3 months | ||||
|---|---|---|---|---|---|---|
| Infants, n | Male | 21 | 20 | 17 | ||
| Female | 29 | 28 | 29 | |||
| Age | Male | 39.8 ± 0.2 wk | 22 ± 1 d | 79 ± 2 d | ||
| Female | 39.6 ± 0.2 wk | 24 ± 1 d | 78 ± 2 d | |||
| Weight, g | Male | 3505 ± 106 | 3996 ± 136 | 6027 ± 200 | ||
| Female | 3465 ± 76 | 3935 ± 97 | 5213 ± 154 | |||
Asterisk represents significant difference between male and female infants (P <0.05).
Study Protocol
Daytime polysomnography was performed in a sleep laboratory where light and noise were minimal and ambient temperature was maintained at approximately 23°C. During a routine morning feed, leads were attached for the measurement of electroencephalogram (EEG), left and right electrooculogram, mental-submental electromyogram (EMG), electrocardiogram, abdominal skin temperature (YSI 400 Series Thermistor, Mallinckrodt, Melbourne, VIC, Australia), thoracic and abdominal breathing movements (Piezo-electric sensors, Resp-ez, EPM Systems, VA, USA), and blood oxygen saturation (SpO2; BIOX 3700e pulse oximeter, Ohmeda, CO, USA). Signals were recorded with a 16-channel polygraph (Model 78A, Grass Instrument Co., Quincy, MA, USA) at a sampling rate of 500 Hz.
Infants were placed supine in a bassinet to sleep. During both AS and QS (scored according to standard criteria24), a series of trigeminal stimuli were used to assess infant arousability as previously described.25 Briefly, a pulsatile jet of air (pulse frequency of 3 Hz, for 5s duration) was delivered via a hand-held cannula, to the left and right nostrils alternately. Stimulus driving pressures ranged between 25 to 900 cm H2O (the pressure applied to the infant was much less, being a maximum of 1.4 cm H2O); beginning low (50 cm H2O), pressures were generally increased by 100 cm H2O between consecutive stimuli, until an arousal response was observed and pressures were then subsequently reduced.
Data Analysis
Responses to each stimulus were classified as either non-arousal, SCA, or CA, in accordance with the standard definitions for infant arousal from sleep.13 With the preceding 10s as the physiological baseline, SCA was identified by the presence of ≥ 2 of the following criteria within 7s of initiating the air-jet; a gross body movement, a heart rate (HR) increase ≥ 10%, an increased EMG amplitude (AS only), and a change in respiratory frequency or amplitude (QS only). CA was visually scored using the same criteria, with the addition of a shift in background EEG frequency (EEG desynchronization) for ≥ 3s.
The percentages of stimuli which resulted in a non-arousal, as well as the mean driving pressure required to elicit an arousal response (either SCA or CA), were calculated to assess total arousability. In a more detailed investigation of the arousal process, SCA and CA were then analyzed as separate components of the arousal response. SCA and CA were also analyzed as percentages of total arousal responses, excluding the non-arousing tests, to control for any differences in total arousability. In addition, as an indication of the magnitude of these responses, the peak HR change recorded during both forms of arousal, and the duration of EEG desynchronization associated with CA were also measured. Individual infants were represented by a single average value of each parameter for each sleep state (AS and QS) at each study age. To determine the effects of sleep state and gender on baseline (HR and respiratory frequency) and arousal parameters, data were first tested for normality and equal variance (Sigmastat 3.0, Systat Software Inc., Richmond, CA, USA), then compared using 2-way analysis of variance (ANOVA) with Student Newman-Keuls post hoc analysis. Statistical significance was considered as P < 0.05 and data are presented as mean ± standard error of the mean (SEM).
RESULTS
Infant numbers, ages and weights for each study are displayed in Table 1. Due to technical complications or infants being unavailable for either one of the two study ages, 6 infants were not studied longitudinally; data were missing for 1 male and 1 female at 2–4 weeks, and for 4 male infants at 2–3 months. Demographics were similar for male and female infants, though male infants were heavier at 2–3 months (P < 0.05). As shown by Table 2, the total number of air-jet stimuli was similar between genders and sleep states, with the one exception being fewer tests performed during AS in female infants at 2–3 months (P < 0.05).
Table 2.
Arousal responses to air-jet stimuli in male and female infants (data represented as mean ± SEM)
| 2–4 weeks |
2–3 months |
|||||
|---|---|---|---|---|---|---|
| Active Sleep | Quiet Sleep | Active Sleep | Quiet Sleep | |||
| Total Stimuli, n | Male | 21 ± 2 | 18 ± 2 | 19 ± 3 | 20 ± 2 | |
| Female | 21 ± 2 | 19 ± 2 | 12 ± 1*# | 19 ± 2 | ||
| Arousal Threshold, cm H2O | Male | 206 ± 22 | 242 ± 27* | 136 ± 21 | 294 ± 39# | |
| Female | 182 ± 15 | 357 ± 37# | 103 ± 12 | 336 ± 35# | ||
| Non-arousals, % | Male | 59 ± 2 | 61 ± 4 | 54 ± 3 | 63 ± 3 | |
| Female | 59 ± 2 | 65 ± 3 | 48 ± 3 | 65 ± 3# | ||
| SCA, % | Male | 26 ± 2 | 34 ± 4 | 33 ± 4 | 31 ± 3 | |
| Female | 28 ± 2 | 29 ± 3 | 37 ± 4 | 27 ± 3 | ||
| CA, % | Male | 15 ± 2 | 5 ± 1# | 12 ± 3 | 6 ± 1 | |
| Female | 13 ± 2 | 6 ± 1# | 15 ± 2 | 7 ± 2# | ||
Symbols represent significant differences;
P <0.05 male vs. female,
P <0.05 AS vs. QS.
Total Arousability
Responses to air-jet
The % of air-jet stimuli which failed to induce arousal from sleep were not different between males and females or between AS and QS at 2–4 weeks. When infants were 2–3 months, there were no significant effects of gender on the % of non-arousing air-jet tests. QS was associated with more frequent non-arousal responses (i.e. decreased arousability) than AS (ANOVA, P < 0.001); this difference was identified as significant only in the female infants after post hoc analysis (P < 0.001, Table 2).
Stimulus intensity
At both ages studied, the mean driving pressures which led to an arousal from sleep (either SCA or CA thresholds) were significantly higher during QS (P < 0.001), being generally more than doubled (Table 2); however in the male infants at 2–4 weeks, there was no QS-related increase. Consequently, when compared with the female infants, the QS arousal threshold was lower in males (P < 0.01).
SCA and CA
Arousal frequency
SCA and CA frequencies were analyzed both as percentages of total stimuli and total arousal responses; the results were the same for both methods, hence only the percentages of stimuli which resulted in SCA and CA are displayed in Table 2. Neither sleep state nor gender had any significant effects on the percentage of SCA at either age. Similarly, CA frequencies were not different between genders. However, a decreased frequency of CA was associated with QS compared with AS at both study ages (P < 0.001), this just failed to reach significance in the male infants at 2–3 months (P = 0.06).
Stimulus intensity
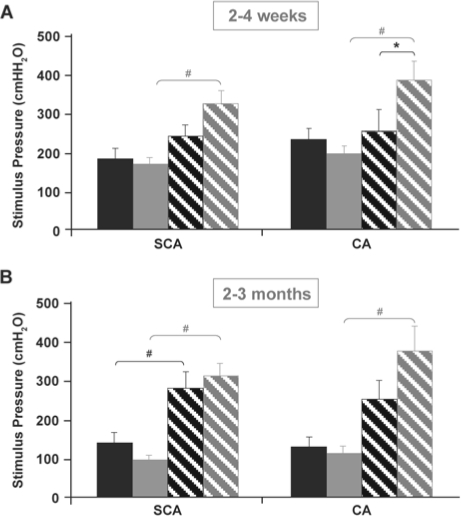
The air-jet driving pressures which induced SCA and CA are displayed in Figure 1. For both SCA and CA, arousing stimulus pressures did not differ between genders; however a significant gender-sleep state interaction was observed for CA thresholds at 2–4 weeks whereby male infants were more easily aroused (i.e. at lower pressures) from QS than females (P < 0.05). Similar trends for the males to exhibit lower arousal thresholds were also evident during QS, for SCA at 2–4 weeks and CA at 2–3 months.
Figure 1.
Mean driving pressures of air-jet stimuli which induced subcortical activation (SCA) and cortical arousals (CA) at (A) 2–4 weeks and (B) 2–3 months, in AS (solid bars) and QS (striped bars), for male (black bars) and female (grey bars) infants. *P < 0.05, male vs. female, #P < 0.05, AS vs. QS.
At both study ages, for both SCA and CA, infants required higher stimulus pressures to arouse during QS than AS (ANOVA, P < 0.001). However at 2–4 weeks, this sleep state effect was only significant in the female infants, with males exhibiting similar arousal thresholds during the two sleep states (P > 0.05, Figure 1A). At 2–3 months, SCA-inducing pressures were significantly lower during AS than QS for both genders (P < 0.01, Figure 1B). This sleep-state difference was also observed in the air-jet pressures which induced CA, though significance in post hoc analysis was confined to the female infants (P < 0.05).
Magnitude of Responses
Heart rate
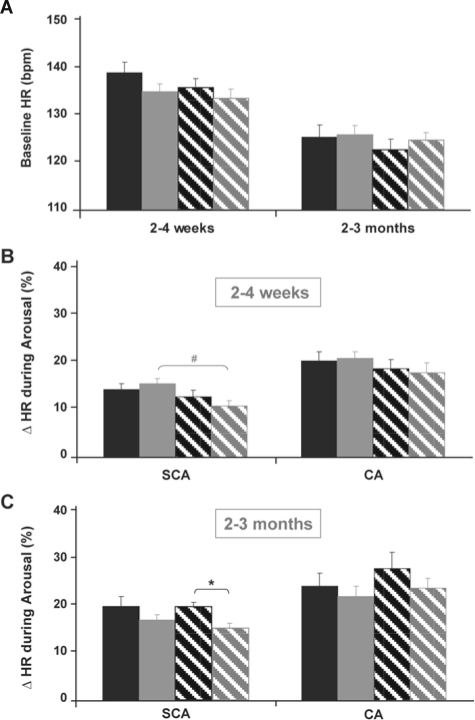
Figure 2 shows baseline HR values and the peak HR changes observed during SCA and CA. There were no effects of gender or sleep state on baseline HR (Figure 2A) or peak HR change (Figure 2B and C) during CA at either postnatal age. At 2–4 weeks, HR changes associated with SCA were reduced during QS when compared with AS in female infants only (P < 0.05, Figure 2B), and also tended to be reduced when compared with male infants in QS. A similar trend for smaller HR responses in the female infants was observed at 2-3 months, although this was significant for SCA only during QS (P < 0.05, Figure 2C).
Figure 2.
(A) Baseline HR data and (B) % HR change during arousal from sleep at 2–4 weeks and (C) at 2–3 months. Data are shown for male (black bars) and female (grey bars) infants, during both AS (solid bars) and QS (striped bars). *P < 0.05, male vs. female, #P < 0.05, AS vs. QS.
EEG desynchronization
The mean durations of EEG desynchronization associated with CA were 11.1 ± 0.8s at 2–4 weeks and 9.4 ± 0.8s at 2–3 months, and were not different between sleep states or between male and female infants.
DISCUSSION
Increased vulnerability of the male gender to SIDS and numerous other morbidities has been well-documented,26–30 with this general “male disadvantage” perhaps resulting from physiological gender differences during development.31 Given the widely proposed relationship between impaired arousability and SIDS,3–5,14 we aimed to comprehensively investigate the effects of gender on arousal from sleep processes, accounting for the progression of SCA to full CA. We demonstrated that at 2–4 weeks postnatal age, male infants were more easily aroused from QS than female infants, i.e. a smaller stimulus was required to induce both SCA and CA. However, this gender difference in arousal threshold was not observed at 2–3 months postnatal age, the age of peak SIDS risk.
Our finding that female infants appeared to sleep more soundly than male infants is consistent with previous reports of increased sleep disruption in male versus female infants; specifically, the maternal perception of their infant's sleep patterns have included more problematic crying and increased night awakenings in male infants.32,33 Similarly, another study observed shorter sleep periods at night in male infants and suggested that, throughout the first six months of age, the normal development of sleeping rhythms is delayed in males when compared with female infants.34 In addition to the development of circadian rhythms and sleep architecture, EEG patterns also undergo dramatic maturational changes throughout the first months of life. These EEG changes are particularly prominent during QS and reflect the occurrence of precise synaptogenesis and the formation of thalamocortical and intracortical connections important in sensory input and arousal.35 In the present study, the gender difference in arousal thresholds was only observed during QS, not in AS. Thus, the male infants exhibited an increased level of arousability in QS that was comparable to that in AS, not reduced arousability as exhibited by female infants. In addition, our cardiovascular analysis revealed that HR acceleration during arousals tended to be larger in the males compared with their female counterparts. Similarly, a previous study by Nagy et al. reported increased HR reactivity to the Moro (startle) reflex in males.34 It is possible that male infants arouse more readily to external stimuli that are suppressed in female infants. It may be that thalamic and extrathalamic processes which serve to filter coincident stimuli may be immature or underdeveloped when compared with female infants at the same age. The view that central nervous system maturation is delayed in male infants is further supported by our finding that the male-related decrease in induced arousal thresholds for both SCA and CA during QS was apparent at the younger age of 2–4 weeks, but not observed at 2–3 months.
In contrast to our current findings, a previous study in our laboratory identified no significant differences between male and female infants when arousal thresholds were compared throughout the first six months of life.36 We ascribe the disparity in results between these two studies to the refinement of standard criteria for defining arousal responses.13 Importantly, by distinguishing between SCA and CA, the present study represents a more sensitive approach than the earlier study which examined total arousability.
Impairment of arousal processes is considered to be an important factor in the pathogenesis of SIDS and the greater risk of male infants succumbing to SIDS has been well documented over the years.2,19–21 Despite observing gender effects on the strength of the stimulus required to elicit arousal responses, our examination of the relative frequencies of SCA and CA revealed no significant differences between male and female infants, either in relation to sleep state or postnatal age. This finding was not predicted by our starting hypothesis that male infants have inhibited CA responses when compared to female infants. We reasoned that if arousal progression from SCA to CA was compromised, there would be a decreased CA frequency and an increased SCA frequency, similar to the response patterns documented in SIDS victims preceding their deaths.14 Rather, in the present study SCA and CA frequencies were not different between male and female infants. Furthermore, the duration of EEG desynchronization associated with CA was also similar. Together, these findings suggest that once initiated, the arousal process is unchanged by gender. Thus, while the gender-related arousal threshold differences may be significant, there are no gender differences in arousal progression from SCA to CA that could increase the vulnerability of male infants to SIDS.
In the present study, approximately 60% of air-jet stimuli failed to induce an arousal response (Table 2). Rather than a physiological phenomenon, this high percentage of non-arousal responses is a reflection of the stepwise nature of the stimulus protocol. In each series of tests, air-jet stimulation commenced at a low driving pressure of 50 cm H2O and was gradually increased in intensity until an arousal response was observed. Subsequent stimuli pressures were adjusted to surround infants' arousal thresholds, thus it was expected that at least 50% of stimuli would result in a non-arousal. It is also important to note that when these non-arousing tests were excluded from data analyses, the effects of gender and sleep state on SCA and CA frequencies remained identical.
The absence of blunted arousal processes in the healthy male infants of this present study suggests that the gender-related vulnerability to SIDS is not a preexisting condition; however, we have previously demonstrated that infant arousal processes can be modified by external factors such as the major risk factors for SIDS—prone sleeping and maternal smoking.16,17 Although the increased incidence of SIDS observed in male infants may not be due to a preexisting vulnerability, it is perhaps a secondary effect of the infants' environment or situation, i.e. the gender effect may be a result of an “exogenous stress” or trigger, as postulated by the triple risk model for SIDS.18 An earlier study in the Netherlands found that more males were being placed prone to sleep than females, though authors offered no explanation for the phenomenon.37 As previously stated, male infants are perceived to be more unsettled than female infants32,33 and studies have shown that excessive crying is one of the primary reasons parents and other caregivers report for placing infants to sleep in the prone position.38 Consequently, a higher prevalence of prone sleeping as a settling technique may contribute to the increased SIDS rates in males.19,39
Our study also investigated the effects of sleep state on arousal progression, as AS and QS are physiologically distinct, and in relation to SIDS risk, researchers have yet to identify in which sleep state infants may be more vulnerable. Respiratory and cardiovascular irregularities occur more frequently during AS, perhaps necessitating an adequate arousal response for maintaining homeostasis. On the other hand, arousability is already depressed during QS,25 which may pose an increased risk, despite the cardiorespiratory stability of this state. By considering both SCA and CA, the present study adds to previous observations of the more arousable nature of infants during AS; overall, non-arousals occurred less frequently and CA more frequently in AS than in QS. The frequencies of induced SCA responses were consistent between both AS and QS, providing support for the single previous study which found no sleep state differences on spontaneous SCA until infants were 5–6 months of age.40
CONCLUSION
At 2–4 weeks, male infants are more easily aroused than female infants, though we observed no significant effects of gender on total arousability or SCA and CA frequencies at 2–3 months, the age of peak SIDS incidence. Thus, although male infants are at greater risk of SIDS than female infants, it is unlikely that this increased vulnerability is caused by a pre-existing inhibition of CA processes; however we speculate that male infants may be more susceptible to being placed in at-risk situations.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors would like to thank all the parents and infants who participated in this study.
Abbreviations
- SIDS
sudden infant death syndrome
- AS
active sleep
- QS
quiet sleep
- SCA
subcortical activation
- CA
cortical arousal
REFERENCES
- 1.Kung H, Hoyert DL, Xu J, Murphy SL. Deaths: Final data for 2005. Natl Vital Stat Rep. 2008;56(10) [PubMed] [Google Scholar]
- 2.Australian Bureau of Statistics. 2007 Causes of Death. Canberra, Australia: 2009. [Google Scholar]
- 3.Phillipson EA, Sullivan CE. Arousal: the forgotten response to respiratory stimuli. Am Rev Respir Dis. 1978;118:807–9. doi: 10.1164/arrd.1978.118.5.807. [DOI] [PubMed] [Google Scholar]
- 4.Harper RM. The cerebral regulation of cardiovascular and respiratory functions. Semin Pediatr Neurol. 1996;3:13–22. doi: 10.1016/s1071-9091(96)80024-6. [DOI] [PubMed] [Google Scholar]
- 5.Kahn A, Sawaguchi T, Sawaguchi A, et al. Sudden infant deaths: from epidemiology to physiology. Forensic Sci Int. 2002;130S:S8–S20. doi: 10.1016/s0379-0738(02)00134-2. [DOI] [PubMed] [Google Scholar]
- 6.Opdal SH, Rognum TO, Vege A, Saugstad OL. Hypoxanthine levels in vitreous humor: a study of influencing factors in sudden infant death syndrome. Pediatr Res. 1998;44:192–6. doi: 10.1203/00006450-199808000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Jones KL, Krous HF, Nadeau J, Blackbourne B, Zielke HR, Gozal D. Vascular endothelial growth factor in the cerebrospinal fluid of infants who died of sudden infant death syndrome: evidence for antecedent hypoxia. Pediatrics. 2003;111:358–63. doi: 10.1542/peds.111.2.358. [DOI] [PubMed] [Google Scholar]
- 8.Paterson DS, Trachtenberg FL, Thompson EG, et al. Multiple serotonergic brainstem abnormalities in sudden infant death syndrome. JAMA. 2006;296:2124–32. doi: 10.1001/jama.296.17.2124. [DOI] [PubMed] [Google Scholar]
- 9.Kinney HC, Filiano JJ, Sleeper LA, Mandell F, Valdes-Dapena M, White WF. Decreased muscarinic receptor binding in the arcuate nucleus in sudden infant death syndrome. Science. 1995;269:1446–50. doi: 10.1126/science.7660131. [DOI] [PubMed] [Google Scholar]
- 10.Lavezzi AM, Ottaviani G, Mauri M, Matturri L. Hypoplasia of the arcuate nucleus and maternal smoking during pregnancy in sudden unexplained perinatal and infant death. Neuropathology. 2004;24:284–9. doi: 10.1111/j.1440-1789.2004.00558.x. [DOI] [PubMed] [Google Scholar]
- 11.Machaalani R, Waters KA. Neuronal cell death in the sudden infant death syndrome brainstem and associations with risk factors. Brain. 2008;131:218–28. doi: 10.1093/brain/awm290. [DOI] [PubMed] [Google Scholar]
- 12.McNamara F, Wulbrand H, Thach BT. Characteristics of the infant arousal response. J Appl Physiol. 1998;83:219–28. doi: 10.1152/jappl.1998.85.6.2314. [DOI] [PubMed] [Google Scholar]
- 13.The International Paediatric Work Group on Arousals. The scoring of arousals in healthy term infants (between the ages of 1 and 6 months) J Sleep Res. 2005;14:37–41. doi: 10.1111/j.1365-2869.2004.00426.x. [DOI] [PubMed] [Google Scholar]
- 14.Kato I, Franco P, Groswasser J, et al. Incomplete arousal processes in infants who were victims of sudden death. Am J Respir Crit Care Med. 2003;168:1298–303. doi: 10.1164/rccm.200301-134OC. [DOI] [PubMed] [Google Scholar]
- 15.Harper RM. Impaired arousals and sudden infant death syndrome. Am J Respir Crit Care Med. 2003;168:1262–3. doi: 10.1164/rccm.2309010. [DOI] [PubMed] [Google Scholar]
- 16.Richardson HL, Walker AM, Horne RSC. Sleep position alters arousal processes maximally at the high-risk age for sudden infant death syndrome. J Sleep Res. 2008;17:450–7. doi: 10.1111/j.1365-2869.2008.00683.x. [DOI] [PubMed] [Google Scholar]
- 17.Richardson HL, Walker AM, Horne RSC. Maternal smoking impairs arousal pathways in sleeping infants. Sleep. 2008;32:515–21. doi: 10.1093/sleep/32.4.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Filiano JJ, Kinney HC. A perspective on neuropathologic findings in victims of the sudden infant death syndrome. Biol Neonate. 1994;65:194–7. doi: 10.1159/000244052. [DOI] [PubMed] [Google Scholar]
- 19.Carpenter RG, Irgens LM, England PD, et al. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet. 2004;363:185–91. doi: 10.1016/s0140-6736(03)15323-8. [DOI] [PubMed] [Google Scholar]
- 20.Blair PS, Sidebotham P, Berry PJ, Evans M, Fleming PJ. Major epidemiological changes in Sudden Infant Death Syndrome: a 20-year population-based study in the UK. Lancet. 2006;367:314–9. doi: 10.1016/S0140-6736(06)67968-3. [DOI] [PubMed] [Google Scholar]
- 21.Mage DT, Donner M. Female resistance to hypoxia: does it explain the sex difference in mortality rates? J Womens Health. 2006;15:786–94. doi: 10.1089/jwh.2006.15.786. [DOI] [PubMed] [Google Scholar]
- 22.Moon RY, Horne RSC, Hauck FR. Sudden infant death syndrome. Lancet. 2007;370:1578–87. doi: 10.1016/S0140-6736(07)61662-6. [DOI] [PubMed] [Google Scholar]
- 23.Thordstein M, Lofgren N, Flisberg A, Lindecrantz K, Kjellmer I. Sex differences in electrocortical activity in human neonates. Neuroreport. 2006;17:1165–8. doi: 10.1097/01.wnr.0000227978.98389.43. [DOI] [PubMed] [Google Scholar]
- 24.Curzi-Dascalova L, Mirmiran M. Manual of methods for recording and analyzing sleep-wakefulness states in preterm and full-term infant. Paris: Les Editions INSERM; 1996. [Google Scholar]
- 25.Parslow PM, Harding R, Cranage SM, Adamson TM, Horne RSC. Arousal responses to somatosensory and mild hypoxic stimuli are depressed during quiet sleep in healthy term infants. Sleep. 2003;26:739–44. doi: 10.1093/sleep/26.6.739. [DOI] [PubMed] [Google Scholar]
- 26.McGregor JA, Leff M, Orleans M, Baron A. Fetal gender differences in preterm birth: findings in a North American cohort. Am J Perinatol. 1992;9:43–8. doi: 10.1055/s-2007-994668. [DOI] [PubMed] [Google Scholar]
- 27.Stevenson DK, Verter J, Fanaroff AA, et al. Sex differences in outcomes of very low birthweight infants: the newborn male disadvantage. Arch Dis Child Fetal Neonatal Ed. 2000;83:F182–5. doi: 10.1136/fn.83.3.F182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vohr BH, Wright LL, Dusick AM, et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993-1994. Pediatrics. 2000;105:1216–26. doi: 10.1542/peds.105.6.1216. [DOI] [PubMed] [Google Scholar]
- 29.Banci M, Saccucci P, Dofcaci A, et al. Birth weight and coronary artery disease. The effect of gender and diabetes. Int J Biol Sci. 2009;5:244–8. doi: 10.7150/ijbs.5.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dasgupta K, O'Loughlin J, Chen S, et al. Emergence of sex differences in prevalence of high systolic blood pressure: Analysis of a longitudinal adolescent cohort. Circulation. 2006;114:2663–70. doi: 10.1161/CIRCULATIONAHA.106.624536. [DOI] [PubMed] [Google Scholar]
- 31.Elsmen E, Pupp IH, Hellstrom-Westas L. Preterm male infants need more initial respiratory and circulatory support than female infants. Acta Paediatr. 2004;93:529–33. doi: 10.1080/08035250410024998. [DOI] [PubMed] [Google Scholar]
- 32.van der Wal MF, van den Boom DC, Pauw-Plomp H, de Jonge GA. Mothers' reports of infant crying and soothing in a multicultural population. Arch Dis Child. 1998;79:312–7. doi: 10.1136/adc.79.4.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anuntaseree W, Mo-suwan L, Vasiknanonte P, Kuasirikul S, Ma-a-lee A, Choprapawan C. Night waking in Thai infants at 3 months of age: association between parental practices and infant sleep. Sleep Med. 2008;9:564–71. doi: 10.1016/j.sleep.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 34.Nagy E, Loveland KA, Orvos H, Molnar P. Gender-related physiologic differences in human neonates and the greater vulnerability of males to developmental brain disorders. J Gend Specif Med. 2001;4:41–9. [PubMed] [Google Scholar]
- 35.Heraghty JL, Hilliard TN, Henderson AJ, Fleming PJ. The physiology of sleep in infants. Arch Dis Child. 2008;93:982–5. doi: 10.1136/adc.2006.113290. [DOI] [PubMed] [Google Scholar]
- 36.Horne RSC, Parslow PM, Ferens D, Watts A-M, Adamson TM. Comparison of evoked arousability in breast and formula fed infants. Arch Dis Child. 2004;89:22–5. [PMC free article] [PubMed] [Google Scholar]
- 37.de Jonge GA, Burgmeijer RJF, Engelberts AC, Hoogenboezem J, Kostense PJ, Sprij AJ. Sleeping position for infants and cot death in the Netherlands 1985-91. Arch Dis Child. 1993;69:660–3. doi: 10.1136/adc.69.6.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Willinger MP, Ko C-WP, Hoffman HJMA, Kessler RCP, Corwin MJMD. Factors associated with caregivers' choice of infant sleep position, 1994-1998: the National Infant Sleep Position Study. JAMA. 2000;283:2135–42. doi: 10.1001/jama.283.16.2135. [DOI] [PubMed] [Google Scholar]
- 39.L'Hoir MP, Engelberts AC, van Well GTJ, et al. Risk and preventive factors for cot death in The Netherlands, a low-incidence country. Eur J Pediatr. 1998;157:681–8. doi: 10.1007/s004310050911. [DOI] [PubMed] [Google Scholar]
- 40.Montemitro E, Franco P, Scaillet S, et al. Maturation of spontaneous arousals in healthy infants. Sleep. 2008;31:47–54. doi: 10.1093/sleep/31.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]