Abstract
Advances in neuroscience are changing how mental health issues such as addiction are understood and addressed as a brain disease. Although a brain disease model legitimizes addiction as a medical condition, it promotes neuro-essentialist thinking, categorical ideas of responsibility and free choice, and undermines the complexity involved in its emergence. We propose a ‘biopsychosocial systems’ model where psycho-social factors complement and interact with neurogenetics. A systems approach addresses the complexity of addiction and approaches free choice and moral responsibility within the biological, lived experience and socio-historical context of the individual. We examine heroin-assisted treatment as an applied case example within our framework. We conclude with a discussion of the model and its implications for drug policy, research, addiction health care systems and delivery, and treatment of substance use problems.
Keywords: mental health, neuroethics, public health, sociology
Brain Biology and Addiction
Recent advances in neuroscience provide compelling evidence to support a medical perspective of problematic substance use and addiction (Dackis and O’Brien 2005). Despite these developments, the science is still in its early stages, and theories about how addiction emerges are neither universally accepted nor completely understood. Current ethical and legal debates in addiction draw upon new knowledge about the biological and neurological modification of the brain (Ashcroft, Campbell, and Capps 2007). Clinically, substance use disorders1 are characterized by compulsive engagement or impaired control over behaviour, evidence of both tolerance and withdrawal, relapse despite continued harm, impairments in social and occupational functioning, and irritability or intense cravings when a particular substance is not directly available (American Psychiatric Association 2004).
Functional brain changes occur in response to stress and other stimuli in people who have substance use problems. Recent neuroimaging studies suggest that people living with a drug addiction have considerable decreases in dopamine D2 receptors and in dopamine release (Volkow, Fowler, Wang, Baler, and Telang 2009), which may contribute to both the rewarding properties of substances and difficulties in abstaining despite adverse consequences. Brain areas such as the prefrontal cortex have been identified as being directly involved in assessing the reward potential of decision-making (Bechara and Damasio 2002; Dom, Sabbe, Hulstijn, and Van Den Brink 2005), and vulnerability to relapse. Abnormal hippocampus and anterior cingulate functioning is associated with challenges in the ability to cope with stress, in addition to problems in cognition (Kaufman, Ross, Stein, and Garavan 2003) such as salience, inhibitory control, motivation, memory, and learning (Hyman 2005). Increased activation of the dorsal striatum has been linked with a vulnerability to strong cravings (Sinha and Li 2007). In addition to the recent studies that are investigating neurogenetic contributions to a vulnerability to addiction (Uhl, Drgon, Johnson, and Liu 2009), arguments have been made for a somatic marker theory of addiction (Verdejo-Garcia and Bechara 2009).
A neurobiological perspective has the potential to provide many benefits to people with addiction in terms of psychopharmacological and other treatment options. However purely reductive, neurobiological explanations of addiction occlude a comprehensive understanding of the added influence of psychological, social, political, and other factors. The view of addiction as primarily a brain disease (Leshner 1997) disregards the extensive body of research that suggests neurogenetic explanations of mental illness contribute to negative perceptions towards people with mental illness and substance use problems (Dietrich, Matschinger, and Angermeyer 2006; Read, 2007; Read, Haslam, Sayce, and Davies 2006). This view is problematic as individuals living with an addiction are highly stigmatized. The brain disease model further implies simplistic categorical ideas of responsibility, namely that addicted individuals are unable to exercise any degree of control over their substance use (Caplan 2006, 2008). This kind of “neuro-essentialism” (Racine, Bar-Ilan, and Illes 2005) may bring about unintentional consequences on a person’s sense of identity, responsibility, notions of agency and autonomy, illness, and treatment preference.
We argue therefore for a biopsychosocial systems model of, and approach to, addiction in which psychological and sociological factors complement and are in a dynamic interplay with neurobiological and genetic factors. As Hyman (2007) has written, “neuroscience does not obviate the need for social and psychological level explanations intervening between the levels of cells, synapses, and circuits and that of ethical judgments” (p.8). Since the so-called brain disease model of addiction does not resolve the volitional nature of substance use completely, a biopsychosocial systems approach attempts to contextualize the individual, thus providing a model to better understand both responsibility and self in addiction.
This paper builds on the conceptual foundations of Hyman’s (2007) contribution on addiction and voluntary control, and extends the thinking to include perspectives that include, but also go beyond, neuroscience.
Psycho-Social Systems
Psycho-social systems are concrete entities or groups whose members act in relation to each other, such as families, religious organizations, and political parties (Bunge 2004). Social processes in addiction are investigated by examining social categories such as networks, groups, organizations and subcultures that alone cannot be explained by neurobiology. Addiction consists of interacting biological and psychosocial mechanisms because the mechanism (e.g., the behaviour) contributing to addiction involves action within a social system. The larger societal structure either restricts or enhances interactions between agents in a social system (Bunge 1997). Such actions require explanations at both the systemic and individual levels.
Every learned action, whether pro-social or anti-social, may be prompted by social conditions such as a lack of resources, conflict, social norms, peer pressure, an underlying drive (e.g., hunger, sex, craving), or a combination of these factors (Bunge 1997). Addiction-related behaviours affect the health of both individuals and communities, either protectively or harmfully. The behaviours influence the extent an individual is able to mobilize and access resources to achieve goals and adapt to adverse situations (Raphael 2004). For example, an individual’s socioeconomic status is correlated with increased negative consequences from substance use, such as increased sharing of used injecting equipment and higher prevalence rates of Human Immunodeficiency Virus (HIV) and hepatitis C (Strike, Myers, and Millson 2004).
There are several processes that actively contribute to substance use with inputs and outputs on biological and psycho-social levels. One example is drug craving that may be experienced as strong, intense urges for immediate gratification that may impair rational thought about future planning (Elster and Skog 1999). Cravings can be cue-elicited by environmental stimuli (Childress, Mozely, McElgin et al. 1999; Loewenstein 2000), and continued exposures to environmental stimuli may instigate a perpetual cycle of cravings and possibly irreversible brain changes that can occur long after an individual has become abstinent. Factors such as drug availability within the environment can increase craving and consequently the vulnerability for relapse (Weiss 2005). Recent research has suggested that enriched environments produce long-term neural modifications that decrease neural sensitivity to morphine-induced reward (Xu, Hou, Gao, He, and Zhang 2007). Accordingly, the social environment can increase the frequency of cravings, which may contribute to increased drug consumption, and thus increase the probability that affected individuals will participate in a series of habituated behaviours that facilitate using (Levy 2007b).
Rates of substance use and dependence vary across, and even within, cultural and social groups (Wallace 1999; Wallace, Bachman, O’Malley et al. 2002). Factors such as availability and peer modeling account for the inter- and intra-group disparities (Thomas 2007). These factors may indicate a certain level of group risk for problematic substance use, but cannot verify either the likelihood of substance use occurring within the group or which individuals within the group are more likely to be affected. These factors are not inherent in the composition of the social structure, are neither stable nor persistent, but are governed by the social values and norms of that social system or group (Bunge 2003).
Social norms regulate behaviour and may act as informal mechanisms of social control. Social groups construct norms that affect individual behaviour, prevalence, and substance use patterns. Group membership in which substance use is socially acceptable, encouraged, or perhaps coerced is significantly associated with patterns of use (Lauer and Lauer 2002). Group norms around social acceptance of substance use dictate variance in consumption rates among diverse ethnic and cultural groups (Caetano and Clark 1998). It is these systemic features that give individuals, in part, motives for action.
Both social norms and laws influence attitudes, perceptions, and beliefs of the effects of substances and considerably affect consumption rates (Babor, Caetano, Casswell et al. 2003; Hawkins, Catalano, and Miller 1992). Proponents of a ‘war on drugs’, for example, believe that laws and policies that are lenient towards substance use are linked with greater prevalence of use and criminal activity. However, research findings have not confirmed this claim. In one study comparing cannabis use in San Francisco (where cannabis is criminalized) and Amsterdam (de facto decriminalization), there was no evidence to support claims that criminalization laws reduce use or that decriminalization increases use. In fact, San Francisco reported a higher cannabis use rate than Amsterdam (Reinarman, Cohen and Kaal 2004).
Shifts in norms and laws can propel changes in behaviours associated with substance use and the prevalence of substance misuse (Hawkins et al. 1992). An example of a profound shift that has occurred since the latter part of the 20th century is tobacco use and a dramatic decline in smoking rates (Health Canada 2007). Progress in the understanding of the pharmacokinetics and pharmacodynamics of nicotine addiction has led to interventions that have helped many individuals curb smoking behaviour. However, the full understanding of these normative shifts includes not just the development of medical interventions for smoking cessation, but also the powerful social and public health efforts to destabilize smoking behaviour. Therefore, smoking has become less acceptable as a normative method of social interaction.
Neuroethics and the Brain Disease Model
Long-standing debates concerning the moral status of addiction have arisen from one of two perspectives: either addiction is a disease of the brain, or addiction is a matter of weak will. The former absolves responsibility and the latter condemns the person, and thus distinguishes between deontological and utilitarian positions. Supporters of the brain disease model cite recent neuroscience research wherein addiction is ontologically reducible to the level of brain cells (Dackis and O’Brien 2005; Volkow and Li 2005). The claim is that a brain disease paradigm will decrease stigma associated with addiction, which should increase access to the health care system. Those inclined to the moral stance see drug use as an intentional, often criminal, act: the “person, not his autonomous brain, is the instigator of relapse and the agent of recovery” (Satel 1999, p.861). Other authors take a somewhat different approach, and conceptualize addiction as a “pleasure-oriented desire” (Foddy and Savulescu 2006, 2007), skeptical that the continued medicalization of addiction will obviate all responsibility for behaviours associated with drug use.
Substance Use, Autonomy and Decision-making
Discussions on the relationship between autonomy and decision-making capacity in addicted persons have received much attention recently in the neuroscience, law, and bioethics literature (Andreou 2008; Burns and Bechara 2007; Caplan 2006, 2008; Carter and Hall 2008a, 2008b; Hall, Capps, and Carter 2008; Levy 2006, 2007a; Morse 2007). These writings have raised questions about the autonomy of people with addictions, their ability to make a free, un-coerced choice, and the extent to which they possess mental competence to consent to research (Carter and Hall 2008a, 2008b; Charland 2002, 2003; Dehue 2002; Hall, Carter and Morely 2003a, 2003b). The view that people with addictions lack decision-making capacity is supported by research in both addiction neuroscience and the neuroscience of decision-making. For example, in non-addicted persons, studies have demonstrated that unconscious brain activation directs behaviour and, consequently, action may not be consciously controlled (Haggard 2008; Soon, Brass, Heinze, and Haynes 2008; Wegner 2002). This view, effectively, undermines intentional self-determination. For addiction, a causal neuroscientific model reinforces notions of a diseased brain. The model suggests that substance use hijacks voluntary brain mechanisms and renders individuals incapable of making rational decisions (Miller and Carroll 2006). These perspectives imply a causal neurophilosophical model of decision-making and action, one that has been critiqued by Gillett (2009). He describes the following trajectory of S_ BE1 _ BE2 _ Output, where:
“S is the stimulus conditions provoking a decision or action
BE1 is the unconscious brain events preceding an action/decision
BE2 is the conscious brain event (complex) or intention causing an action/decision
Output is a bodily movement or a decision” (p. 332).
Gilllett argues that the causal model is based on a faulty account of human autonomy and consciousness and is scientifically and conceptually questionable. Gillett challenges the neurophilosophical model of human decision-making, which, as he has previously argued (2008a), emphasizes selfishness, and “constricts the scope of reason so that it is subject to any desire or disposition that one happens to endorse at the time one acts” (p. 1215). Gillett criticizes theories of decision-making that conceptualize choice as autonomous phenomenon only if inner mental states or networks cause it.
While making a decision is itself a mental act, a mental act or event does not cause behaviour alone, but is one part of the complex process between neuronal firing and action. Once an intention has been formed for example, to use substances one is aware of the intention, though intention itself does not sufficiently cause the individual to seek out or use drugs. Other factors are at play. From a neuroscience perspective, it is difficult to see such actions as completely free, particularly when explanations of natural phenomena are understood as causally ordered. The notion of free choice becomes particularly troublesome due to the conscious experience of acting freely. As Searle (2004) argues, “there is a striking difference between the passive character of perceptual consciousness and the active character of what we might call ‘volitional consciousness’“ (41).
Action, subjective experience of action, and consequently responsibility for action is mediated by many factors, including psychological phenomenon such as an individual’s emotional processes. As a point of illustration, Damasio’s (1994) somatic marker hypothesis (SMH) provides a helpful perspective on integrating the neuropsychological domain of decision-making and human interaction with the social environment. The SMH proposes a mechanism where emotion guides or significantly influences behaviour, particularly decision-making. Somatic markers are acquired by experience and are under control of a neural “internal preference system [which] is inherently biased to avoid pain, seek potential pleasure, and is probably pretuned for achieving these goals in social situations” (Damasio 1994, 179). The brain responds to particular social cues that may provide instant pleasure, or regulate biological homeostasis, such as relief from withdrawal (Li and Sinha 2008). Brain systems that moderate feeling, memory, cognition, and engage the individual with the world influence the decision to consume or not consume a drug, or participate in a specific behaviour or series of actions. Accordingly, this cybernetic brain-environment interaction may trigger strong somatic signals such as desire, urge and anticipation (Verdejo-Garcia and Bechara 2009). In effect, this process may limit autonomy as it allows for “preference reversals” (Levy 2007a) to occur in situations where an individual would rather not use.
The degrees in which self-control is exerted, free choice is realized and desired outcomes achieved are dependent on these complex interacting biopsychosocial systems. Many post-modern theorists such as Christman (2004) have challenged the original Kantian privileging and definition of autonomy. One claim is based on the fact that decisional autonomy, or rationality, is not the most valuable human characteristic, and the individual-as-independent does not adequately characterize human beings (Russell 2009). Accordingly, the matrix of a person’s socio-historical context, life narrative, genetics, and relationships with others influence intention, decision, and action, and thus shape the brain. Autonomy, therefore, is not adequately defined just by the events in the brain or the “quality” of the decision being made. As Gillett (2009) remarks, “a decision is…not a circumscribed event in neuro-time that could be thought of as an output, and an intention is not a causal event preceding that output, but both are much more holistically interwoven with the lived and experienced fabric of one’s life” (p. 333). Many individuals who have serious addictions live in impoverished environments without suitable resources or opportunities. Thus it is the limited option for choice that is one prevailing variable, not only the reduced ability to choose alternatively.
An individual living with an addiction is in-the-world-with-others and thus acts as a being-among-others, such that the individual’s decisions and complex engagement with the world may not be as automatic as the neurophilosophical model may suggest (Gillett 2008a, 2008b, 2009). For that reason, individuals who live with an addiction may not completely be enslaved or forced by their brain in the way in which, as Levy (2007a) has previously deferred to Aristotle (1999), “a wind or people have [an agent] in their control were to carry him off” (p.30). Given the spectrum nature of substance use problems, decision-making capacity is therefore neither completely present nor absent, but may be, at some times in certain contexts, weakened. One area in particular in which these neuroethics notions of addiction may have significant impact is in the clinical setting.
Addiction Neuroethics in the Clinical Context
A future application of clinical neuroscience may allow for more precise prediction of a neurogenetic vulnerability to addiction, lead to better understanding of pharmacokinetics and pharmacodynamics of drug use, and to bring greater precision to diagnosis than is currently possible. Realizing a neurobiological or genetic susceptibility to addiction could empower life planning and the avoidance of high-risk scenarios. Individuals involved in treatment could learn effective coping strategies, modify proximal environmental triggers, and achieve other social goals. Yet when neurogenetic attributions are made entirely irrespective of their social context, individuals with mental health problems are viewed as less responsible (Mehta and Farina 1997), and the individuals themselves may perceive a limited control over their actions (Shiloh, Rashuk-Rosenthal, and Benyamini 2002). These perceptions may greatly affect addiction recovery rates (Godin and Kok 1996). As Hall and colleagues (2003a) remark, “A ‘disease’ that can be ‘seen’ in the many-hued splendor of a PET scan carries more conviction than one justified by the possibly exculpatory self-reports of individuals who claim to be unable to control their drug use” (p.1485).
When neurogenetic attributions are presented in the clinic, pharmacological treatments are often believed to be a more effective option over psychotherapy (Phelan, Yang, and Cruz-Rojas 2006). This attribution could sway those who assign the cause of their addiction to be exclusively neurological or genetically based, and not necessarily evaluate the risks and benefits of pharmacotherapy, psychotherapy, or receiving both as combination. These causal neurogenetic attributions have led some authors to advocate for involuntary treatment in addiction, arguing that, paradoxically, autonomy must be denied, “in order to create it” (Caplan 2008). In these extreme examples, a Ulysses contract (Andreou 2008) may be more respectful of autonomy, and relevant harm reduction approaches in the clinical setting may help empower a person to be more autonomous in their treatment decisions, pursue what is meaningful to him or her, and accept the accompanying responsibilities (Buchman and Russell 2009).
Notions of a pathologized self, deeply enmeshed with personal identity, may lead an individual to internally negotiate a relationship between the self and the brain (Dumit 2003). It may further challenge understandings of “accepted” identities, such as health seeking and rational, as opposed to “contested” identities, such as addict, intoxicated, and at-risk (Fry 2008). The latter may compromise an individual’s sense and experience of free will, being-in-the-world, perceptions of personal responsibility, and view abnormalities in dopamine pathways as fatalistic.
Guiding an individual’s behaviour are brain processes, somatic mechanisms, the ethical rules and norms that govern society, and the nature of the interaction. The complex combination of biological, psycho-social and systemic factors may explain why it is so difficult for some individuals to refuse drugs in the face of increasingly negative consequences. An underlying feature of these interacting systems is the human subjective experience of free voluntary actions, which problematizes laws within the natural world that every event has a cause with causally sufficient explanations.
Biopsychosocial Systems Approach
The biopsychosocial model of addiction (Figure 1) posits that intersecting biological, psycho-social and systemic properties are fundamental features of health and illness. The model includes the way in which macro factors inform and shape micro systems and brings biological, psychological and social levels into active interaction with one another. It is a model based on Engel’s original biopsychosocial model (Engel 1977) for which he argued that to develop a scientific and comprehensive description of mental health, theories that promote biological reductionism should be dismissed in favour of those that adhere to general systems theory. The contemporary model, adapted for addiction, reflects an interactive dynamic for understanding substance use problems specifically and addressing the complexity of addiction-related issues. The empirical foundation of this model is thus interdisciplinary, and both descriptive and applied.
Figure 1.
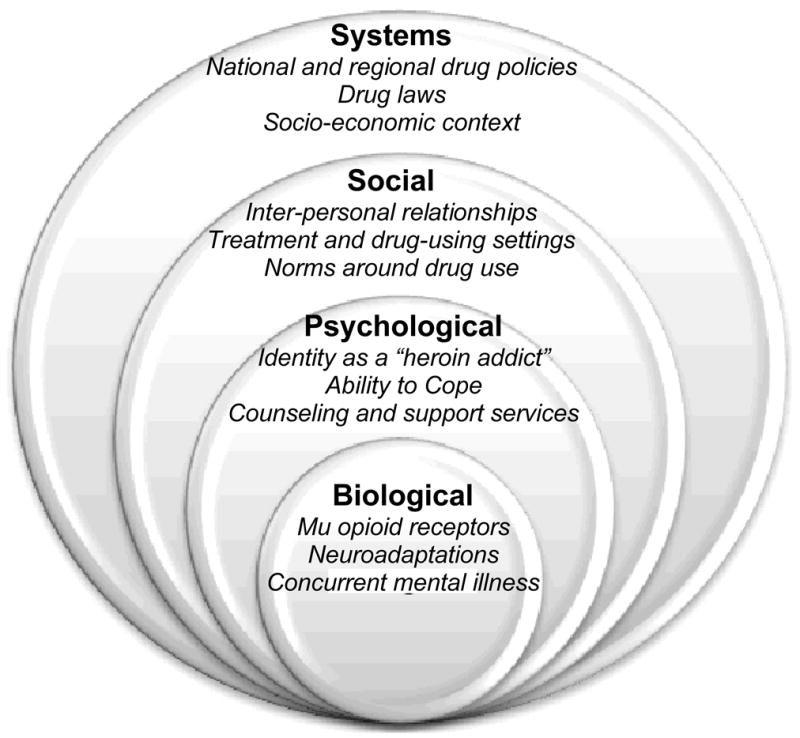
The Biopsychosocial Systems Model of Addiction. Primary features of the model are shown in boldface; variables exemplifying heroin-assisted treatment are shown in italics.
The biopsychosocial systems model is grounded in systems theory in which knowledge occurs at the intersection of the subjective and the objective, and not as an independent reality. This is a radical departure from the traditional positivist epistemology, which relies on empirical study and material proof (Bunge 1979; Heylighen, Cilliers, and Gerschenson 2007). Such new iterations of systems theory concentrate on the cognitive and social processes wherein the construction of subjective knowledge occurs. Each element of a system may be a complex system in its own right. The dynamic within these relationships can contribute to or inhibit the emergence of a complex behaviour such as problematic substance use, while regulating both inputs and outputs from changing internal and external environments. The complex behaviour contributes both positive and negative feedback, and thus affects how the complex behaviour emerges. Systems theory, therefore, balances reductionism and the intrinsic heterogeneity within systems.
The actual social component of the biopsychosocial model is limited, however. The social domain tends to account only for proximal environmental and social properties. The social does not necessarily include macrosocial circumstances, such as governmental social policies, drug policy or drug ‘strategy’ that has a direct effect on substance use rates and patterns. A systems approach strives to achieve a unification of disciplines neuroscience, biology, psychology, sociology, philosophy, economics, politics and law by examining interacting and emerging patterns from each discipline, rather than focusing on common material components (Heylighen et al. 2007). In this light, the addition of systems to the prototype biopsychosocial model allows for the inclusion of macrosocial systems as well as smaller components, such as cells and genes. Together they shape individual actions and behaviours. A systems approach allows for the inclusion of psycho-social and socially systemic explanations of addiction, which extend well beyond neurobiology while still interacting with it (Bunge 1991).
The biopsychosocial systems model implicitly calls for an integrative discussion in the ethics debate on substance use, decision-making, and responsibility. The model avoids a forced choice between brain disease and condition of a weak will, and thus provides a useful framework for overcoming a neuro-essentialist trap. Instead of focusing entirely on causal, reductive neurobiology and difficulties in decision-making, the biopsychosocial systems model places the individual in his or her social environment and integrates his or her life narrative. The model contextualizes the responsibility placed on the individual and further allows for individual members of society to reflect on their own contributions in facilitating substance misuse (Levy 2007b). The model, therefore, allows for diverse and multidimensional aspects of knowledge to be drawn upon depending on the concern to be addressed, and the tools available to address them (Cochrane 2007).
A biopsychosocial systems approach does not portray people as only controlled by the state of their brains. Addictive behaviours are neither viewed as controlled or uncontrolled but as difficult to control a matter of degree. Further, the clinically observed defining feature of addiction a loss of control is understood as a socially normative notion. Thus the claim that “an addict cannot be a fully free autonomous agent” (Caplan 2008, p.1919) is debatable. While it assumes that people are usually fully free and autonomous, contemporary discussions about autonomy as a hyper-value or hypergood (Frank 2004; Gaylin and Jennings 2003; Taylor 1989) and conceptions of relational autonomy (Sherwin 1998) necessitate a contextualized discussion of autonomy in debates about addictions (Buchman and Russell 2009). Because of a tendency to focus on extreme pathological states, the wide range of normal is often forgotten.
Heroin-Assisted Treatment: An Applied Case Example
Advances in addiction research are increasingly being applied to gain deeper knowledge about the impact of drug use on brain structure and functioning, capacity, autonomy, free choice and decision-making, behaviour, treatment, and symptom reduction. While research of this kind raises important issues about identity, and notions of health and illness, the outcomes have implications for drug policy, health care systems and delivery, and treatment for substance use problems.
Addictions research using heroin-assisted treatment (HAT) trials such as the North American Opiate Medication Initiative (NAOMI) and similar HAT studies and programs in Europe are a striking, if not controversial example of an effort to embody a biopsychosocial systems approach. The objective of these trials is to investigate the benefits and risks of administering medically supervised, pharmaceutical-grade injectable heroin to chronic opiate users where other treatment options, such as methadone maintenance therapy, have failed.
The NAOMI trial raised significant scientific, legal, ethical and political concerns, which included issues of patient safety, the controversial use of placebo control therapy, lack of equipoise, treatment discontinuation, and compassionate access to treatment (Oviedo-Joekes, Nosyk, Marsh, et al. 2009). Reflecting on these concerns, the authors stated “we [had] to be clear in our ethics applications and in our informed consent process with participants that HAT will not be available outside the context of the study” (p. 267). Although a full discussion is warranted pertaining to these challenges, these ethical concerns raised by Oviedo-Joekes et al. (2009) resonate with our present discussion.
Properties of the biopsychosocial systems model are reflected in the case example of HAT. Here, we examine some of the ethical challenges to research, service delivery, the philosophies and strategies of harm reduction, and clinical practice that HAT presents.
Integrating Cells and Society
Semi-synthetic opiates such as heroin mainly activate mu opioid receptors in the central nervous system (Koob, Sanna, and Bloom 1998). Mu receptors activate analgesia, respiratory depression, miosis, euphoria, and reduced gastrointestinal motility. Frequent and chronic opioid exposure may lead to a significant amount of neuroadaptations, which are believed to contribute to tolerance, withdrawal, and other mechanisms contributing to the cycle of compulsive use and relapse (Christie 2008).
Heroin is lipid soluble, which leads to fast penetration of the blood-brain barrier and high abuse potential (Julien 2001). The reinforcing and euphoric properties of opiates arise from increased amounts of extracellular dopamine in the ventral tegmental area and nucleus accumbens. Individuals experiencing withdrawal may suffer severe symptoms that include sweating, nausea, vomiting, abdominal pain and irritability (Koob and Le Moal 2005). The risk of mortality is increased due to overdoses; there is an increased risk of acquiring bacterial infections, and other blood-borne pathogens such as HIV and HCV, as described earlier. Concurrent mental illness and addiction the norm rather than exception further characterize individuals with severe opiate addiction (Rush, Urbanoski, Bassani, et al. 2008).
Chronic opioid dependence is associated with a high prevalence of health and psychosocial issues (Oviedo-Joekes et al 2009), such as high rates of underemployment and unemployment, involvement with the legal system, unstable housing, and street-involvement (Fischer, Rehm, Brissette, et al 2005). Research from Europe suggests that chronic heroin-injection users, who received heroin under supervision in tandem with drug treatment, were less likely to be involved in criminal activities (Killias, Aebi, and Ribeaud 1998), had better treatment retention (Haasen, Verthein, Degkwitz et al. 2007), improved social functioning, and had reduced mortality (Rehm and Fischer 2008). Data from Canadian trials (Oviedo-Joekes, Nosyk, Brissette et al., 2008), show a greater percentage of female participants compared to the European trials and a high percentage more than 70% of participants residing in precarious housing.
Additionally, a recent study by Lasnier, Brochu, Boyd, and Fischer (2009) did not find any evidence of an increase or decrease in community-based crime associated with HAT clinics in Canada.
The deontological principle of respect for persons is a characteristic feature of harm reduction efforts such as HAT. This ethical principle is justified and framed as a matter of human rights, which maintains that injection drug users, for example, have the right, like other less stigmatized members of society, to access medical and social services. This claim coincides with a recent emergence of a global advocacy movement that seeks to construct the use of drugs as a human right (Elliott, Csete, Wood, and Kerr 2005; Lines and Elliott 2007).
Hunt (2004) takes the rights-based notion further and identifies and characterizes two ethics of harm reduction. First, he describes a “weak” rights ethic, wherein individuals have the right to access good healthcare. Second, Hunt identifies a “strong” rights account that acknowledges a basic right to use drugs. Based on this definition, we believe that HAT falls into both camps HAT seeks to promote the right to access good health care, and the basic right as an individual asserting sovereignty over his or her body to inject heroin.
Stigma, Heroin Assisted Treatment, and the Biopsychosocial Systems Model
Whether or not drug use is recognized or constructed as a basic right, individuals living with an addiction are amongst the most stigmatized members of society. Although stigma is entrenched in all levels of social fabric, including health care services, it is important to understand how individuals who participate in clinical trials or treatment may perceive the supervised injecting of heroin. In a recent study examining stigma and supervised methadone maintenance therapy, Anstice, Strike, and Brands (2009) found that convenient access to services, relationships with pharmacists and dispensing staff, and characteristics of where the methadone was distributed were intimately linked with the client’s experiences of being stigmatized. Moreover, the authors noted that some methadone dispensing locations helped clients mitigate a stigmatized identity of “a drug user”; while other dispensing locations exposed or perhaps did not take adequate steps to limit or minimize this effect. Building on the findings from Anstice et al., future studies can examine ways in which treatment outcomes can be improved by reducing stigma associated with supervised treatment such as HAT.
The social burden of illicit drug addiction is estimated at billions of dollars per year (Fisher, Oviedo-Joekes, Blanken, et al. 2007). Research that involves providing drugs to individuals living with an addiction must negotiate between science, ethics, politics, law, and evidence-based medicine. For instance, despite its cost-effectiveness and ease on burden of disease, the supervised injection site (SIS) in the Downtown Eastside area of Vancouver, Canada has been repeatedly threatened with closure by politicians. The threats are based on emotional and moral attitudes towards the existence of the SIS and drug addicts generally, as opposed to empirical evidence (Des Jarlais, Arasteh, and Hagan 2008).
The structural systems of society have a significant effect not only on the provision of service delivery, but also on the design of randomized controlled trials like NAOMI, which seek to minimize the health and social burden of drug addiction. Social justice demands that politicians permit, and researchers and health care providers scientifically evaluate, more controversial methods to treat stigmatized conditions such as addiction, where other methods have either failed or provided limited benefit for the most marginalized members of society. Accordingly, Oviedo-Joekes et al (2009) describe the systems approach to heroin-assisted treatment:
“HAT is not simply a pharmacotherapy; it is a treatment approach that is situated within a context involving neighborhood factors, the local drug scene, housing, policing, medical care, and other treatment services. Its role and effectiveness is entangled with the ancillary services available, drug policies, and treatment philosophy” (p.262).
The biopsychosocial systems approach provides the impetus for a benevolent view of individuals who have a serious addiction, such as heroin, and the data to date suggest that, however unorthodox, the intervention appropriately address addiction related issues, including stigma, at both the individual and societal level.
Conclusions
Robert K. Merton observed that, “In the modern world, the visibly practical accomplishments of a science largely affect the social value placed upon it” (Merton 1961, 697). Media headlines such as “Brain’s Addiction Centre Found” (BBC 2007) speak to the power of neuroscience and its ability to construct images of the brain, such that it has become easy to defer to its account of the complex phenomena that constitute addiction. Neuroethics challenges arise when knowledge exclusively from neuroscience is deemed adequate to obtain a full understanding of a mental health disorder as complex as addiction. While the practicality of biopsychosocial systems model may allow for a more integrative explanation for addiction, it does not explain addiction entirely. Indeed, there is no single theory or approach that can offer a complete explanation for the existence of any social problem (Merton 1961). Moreover, the model does not solve the problem of free choice, as the model still, even at the systems (macro) level, has causally sufficient preceding conditions.
It is the integration of biological data and psycho-social, narrative, family information, and clinical phenomenology that will make way for more precise forecasting and earlier diagnosis than is possible today. This is one path to follow for new opportunities for treatment and intervention directed toward prevention. Accordingly, an analysis of the ethical, legal and social issues around other problems of addiction, such as prescription opiate misuse for pain management, may also be examined within the context of our proposed framework.
The application of a multi-dimensional model like the model proposed here is not revolutionary. As a rule, mental health workers are familiar with an integrative understanding of addiction, and would not recommend a treatment intervention based on biological information alone. However the rapid developments in neuroscience are moving bio-psychiatry away from the mind, and towards actions in the brain. Mind once was the place of mediation between person and situation, between the biological and the social. How these advances will impact the ethical relationship between our brains and our selves in addiction, is yet to be seen.
Acknowledgments
This paper is based on a thesis in fulfillment of the requirements for a Master of Social Work in the Collaborative Program in Addiction Studies at the University of Toronto. Special thanks to Dr. Barbara Russell and Dr. Marilyn Herie at both the Centre for Addiction and Mental Health and the University of Toronto who advised on earlier versions of the manuscript; Neil Chahal and Sofia Lombera at the National Core for Neuroethics at the University of British Columbia; the two anonymous reviewers for their thoughtful remarks. Supported by NIH/NIMH (#MH R01MH84282-04A1), the Canadian Institutes for Health Research (CNE #85117), the Michael Smith Foundation for Health Research, and the Vancouver Coastal Health Research Institute.
Footnotes
The DSM-IV-TR differentiates between Substance Dependence and Substance Abuse. In this paper we use the term “substance use disorder” or “addiction” to refer to both the complex nature of severe substance dependence and substance abuse.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders DSM-IV-TR fourth edition text revision. Washington, DC: American Psychiatric Association; 2004. [Google Scholar]
- Andreou C. Making a clean break: Addiction and Ulysses contracts. Bioethics. 2008;22:25–31. doi: 10.1111/j.1467-8519.2007.00588.x. [DOI] [PubMed] [Google Scholar]
- Anstice S, Strike CJ, Brands B. Supervised methadone consumption: Client issues and stigma. Substance Use and Misuse. 2009;44(6):794–808. doi: 10.1080/10826080802483936. [DOI] [PubMed] [Google Scholar]
- Irwin T, translator. Aristotle. Nicomachean ethics. 2. Indianapolis: Hackett Publishing Company, Inc; 1999. [Google Scholar]
- Ashcroft R, Campbell AV, Capps B. Ethical aspects of developments in neuroscience and drug addiction. In: Nutt D, Robbins TW, Stimson GV, Ince M, Jackson A, editors. Drugs and the future. London: Elselvier; 2007. pp. 439–465. [Google Scholar]
- Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K. Alcohol: No ordinary commodity: Research and public policy. New York: Oxford University Press; 2003. [Google Scholar]
- BBC. Brain’s ‘addiction centre’ found. 2007 January Thursday 25; Retrieved 3 December 2008, from http://news.bbc.co.uk/2/hi/health/6298557.stm.
- Bechara A, Damasio H. Decision-making and addiction (part1): impaired activation of the somatic states in substance dependent individuals when pondering decisions with negative future consequences. Neuropsychologia. 2002;40:1675–1689. doi: 10.1016/s0028-3932(02)00015-5. [DOI] [PubMed] [Google Scholar]
- Buchman DZ, Russell BJ. Addictions, autonomy and so much more: A reply to Caplan. Addiction. 2009;104:1053–1055. doi: 10.1111/j.1360-0443.2009.02569.x. [DOI] [PubMed] [Google Scholar]
- Bunge M. Treatise on basic philosophy Vol. 4: A world of systems. Dordrecht: Kluwer; 1979. [Google Scholar]
- Bunge M. The power and limits of reduction. In: Agazzi E, editor. The problem of reductionism in science. Dordrecht: Kluwer Academic Publishers; 1991. pp. 31–49. [Google Scholar]
- Bunge M. Mechanism and explanation. Philosophy of the Social Sciences. 1997;27:410–465. [Google Scholar]
- Bunge M. Emergence and convergence. Toronto: University of Toronto Press; 2003. [Google Scholar]
- Bunge M. How does it work? The search for explanatory mechanisms. Philosophy of the Social Sciences. 2004;34:182–210. [Google Scholar]
- Burns K, Bechara A. Decision making and free will: A neuroscience perspective. Behavioral Science and the Law. 2007;25:263–280. doi: 10.1002/bsl.751. [DOI] [PubMed] [Google Scholar]
- Caetano R, Clark C. Trends in alcohol consumption patterns among Whites, Blacks and Hispanics: 1984 and 1995. Journal of Studies on Alcohol. 1998;59:659–668. doi: 10.15288/jsa.1998.59.659. [DOI] [PubMed] [Google Scholar]
- Caplan AL. Ethical issues surrounding forced, mandated or coerced treatment. Journal of Substance Abuse Treatment. 2006;31:117–120. doi: 10.1016/j.jsat.2006.06.009. [DOI] [PubMed] [Google Scholar]
- Caplan AL. Denying autonomy in order to create it: The paradox of forcing treatment upon addicts. Addiction. 2008;103:1919–1921. doi: 10.1111/j.1360-0443.2008.02369.x. [DOI] [PubMed] [Google Scholar]
- Carter A, Hall W. Informed consent to opioid agonist maintenance treatment: Recommended ethical guidelines. International Journal of Drug Policy. 2008a;19(1):79–89. doi: 10.1016/j.drugpo.2007.09.007. [DOI] [PubMed] [Google Scholar]
- Carter A, Hall W. The issue of consent in research that administers drugs of addiction to addicted persons. Accountability in Research. 2008b;15(4):209–225. doi: 10.1080/08989620802388689. [DOI] [PubMed] [Google Scholar]
- Charland LC. Cynthia’s dilemma: Consenting to heroin prescription. The American Journal of Bioethics. 2002;2(2):37–47. doi: 10.1162/152651602317533686. [DOI] [PubMed] [Google Scholar]
- Charland LC. Heroin addicts and consent to heroin therapy: A comment on Hall et al. Addiction. 2003;98(11):1634–1635. doi: 10.1046/j.1360-0443.2003.00567.x. [DOI] [PubMed] [Google Scholar]
- Childress AR, Mozely PD, McElgin W, Fitzgerald J, Reivich M, O’Brian CP. Limbic activation during cue-induced cocaine craving. American Journal of Psychiatry. 1999;156:11–18. doi: 10.1176/ajp.156.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christie MJ. Cellular neuroadaptations to chronic opioids: Tolerance, withdrawal and addiction. British Journal of Pharmacology. 2008;154(2):384–396. doi: 10.1038/bjp.2008.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christman J. Relational autonomy, liberal individualism, and the social constitution of selves. Philosophical Studies. 2004;117:143–164. [Google Scholar]
- Cochrane TI. Brain disease or moral condition? Wrong question. American Journal of Bioethics (AJOB-Neuroscience) 2007;7(1):24–25. doi: 10.1080/15265160601064108. [DOI] [PubMed] [Google Scholar]
- Dackis C, O’Brien C. Neurobiology of addiction: treatment and public policy ramifications. Nature Neuroscience. 2005;8(11):1431–1436. doi: 10.1038/nn1105-1431. [DOI] [PubMed] [Google Scholar]
- Damasio AR. Descartes’ error. New York: Harper Collins; 1994. [Google Scholar]
- Dehue T. A Dutch treat: Randomized controlled experimentation and the case of heroin-maintenance in the Netherlands. History of the Human Sciences. 2002;15(2):75–98. [Google Scholar]
- Des Jarlais DC, Kamyar A, Hagan H. Evaluating Vancouver’s supervised injection facility: Data and dollars, symbols and ethics. Canadian Medical Association Journal. 2008;179(11):1105–1106.4. doi: 10.1503/cmaj.081678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietrich S, Matschinger H, Angermeyer MC. The relationship between biogenetic causal explanations and social distance toward people with mental disorders: Results from a population survey in Germany. The International Journal of Social Psychiatry. 2006;52(2):166–174. doi: 10.1177/0020764006061246. [DOI] [PubMed] [Google Scholar]
- Dom G, Sabbe B, Hulstijn W, Van Den Brink W. Substance use disorders and the orbitofrontal cortex. British Journal of Psychiatry. 2005;187:209–220. doi: 10.1192/bjp.187.3.209. [DOI] [PubMed] [Google Scholar]
- Dumit J. Is it me or my brain? Depression and neuroscientific facts. Journal of Medical Humanities. 2003;24(1–2):35–47. [Google Scholar]
- Elliott R, Csete J, Wood E, Kerr T. Harm reduction, HIV/AIDS, and the human rights challenge to global drug control policy. Health and Human Rights. 2005;8:104–138. [PubMed] [Google Scholar]
- Elster J, Skog O-J. Getting hooked: Rationality and addiction. Cambridge, U.K: Cambridge University Press; 1999. [Google Scholar]
- Engel GL. The need for a new medical model: A challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- Fischer B, Rehm J, Brissette S, Brochu S, Bruneau J, El-Guebaly, et al. Illicit opioid use in Canada: Comparing social, health, and drug use characteristics of untreated users in five cities (OPICAN study) Journal of Urban Health. 2005;82(2):250–266. doi: 10.1093/jurban/jti049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer B, Oviedo-Joekes E, Blanken P, Haasen C, Rehm J, Schechter MT, Strang J, van den Brink W. Heroin-assisted treatment (HAT) a decade later: A brief update on science and politics. Journal of Urban Health. 2007;84(4):552–562. doi: 10.1007/s11524-007-9198-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foddy B, Savulescu J. Addiction and autonomy: Can addicted people consent to the prescription of their drug of addiction? Bioethics. 2006;20:1–15. doi: 10.1111/j.1467-8519.2006.00470.x. [DOI] [PubMed] [Google Scholar]
- Foddy B, Savulescu J. Addiction is not an affliction: Addictive desires are merely pleasure-oriented desires. The American Journal of Bioethics (AJOBNeuroscience) 2007;7:29–32. doi: 10.1080/15265160601064157. [DOI] [PubMed] [Google Scholar]
- Frank A. Ethics as process and practice. Internal Medicine Journal. 2004;34:355–357. doi: 10.1111/j.1445-5994.2004.00622.x. [DOI] [PubMed] [Google Scholar]
- Fry CL. A social neuroethics of addiction: Revealing public and private identities and self understanding. Poster at the 1st Annual Meeting of the Neuroethics Society; Washington, D.C., USA. 2008. [Google Scholar]
- Gaylin W, Jennings B. The perversion of autonomy: Coercion and constraints in a liberal society. Washington: Georgetown University Press; 2003. [Google Scholar]
- Gillett G. Autonomy and selfishness. The Lancet. 2008a;372(9645):1214–1215. doi: 10.1016/s0140-6736(08)61507-x. [DOI] [PubMed] [Google Scholar]
- Gillett G. Subjectivity and being somebody: Human identity and neuroethics. Exter: Imprit Academics; 2008b. [Google Scholar]
- Gillett G. Intention, autonomy, and brain events. Bioethics. 2009;23(6):330–339. doi: 10.1111/j.1467-8519.2009.01726.x. [DOI] [PubMed] [Google Scholar]
- Godin G, Kok G. The theory of planned behavior: A review of its applications to health-related behaviors. American Journal of Health Promotion. 1996;11:87–98. doi: 10.4278/0890-1171-11.2.87. [DOI] [PubMed] [Google Scholar]
- Haasen C, Verthein U, Degkwitz P, Berger J, Krausz M, Naber D. Heroin-assisted treatment for opioid dependence. British Journal of Psychiatry. 2007;191:55–62. doi: 10.1192/bjp.bp.106.026112. [DOI] [PubMed] [Google Scholar]
- Haggard P. Human volition: Towards a neuroscience of will. Nature Reviews Neuroscience. 2008;9:934–946. doi: 10.1038/nrn2497. [DOI] [PubMed] [Google Scholar]
- Hall W, Capps B, Carter A. The use of depot naltrexone under legal coercion: The case for caution. Addiction. 2008;103:1922–1924. doi: 10.1111/j.1360-0443.2008.02370.x. [DOI] [PubMed] [Google Scholar]
- Hall W, Carter L, Morely KI. Addiction, neuroscience and ethics. Addiction. 2003a;98(7):867–870. doi: 10.1046/j.1360-0443.2003.00400.x. [DOI] [PubMed] [Google Scholar]
- Hall W, Carter L, Morely KI. Addiction, ethics and scientific freedom. Addiction. 2003b;103:873–874. doi: 10.1046/j.1360-0443.2003.00457.x. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Health Canada. Canadian tobacco use monitoring survey. 2007 August 25, 2008. Retrieved December 5, 2008, from http://www.hc-sc.gc.ca/hl-vs/tobac-tabac/researchrecherche/stat/ctums-esutc_2007-eng.php.
- Heylighen F, Cilliers P, Gerschenson C. Complexity and philosophy. In: Bogg J, Geyer R, editors. Complexity, science and society. Radcliffe: Oxford University Press; 2007. [Google Scholar]
- Hunt N. Public health or human rights: What comes first? International Journal of Drug Policy. 2004;15(4):231–237. [Google Scholar]
- Hyman SE. Addiction: a disease of learning and memory. The American Journal of Psychiatry. 2005;162(8):1414–1422. doi: 10.1176/appi.ajp.162.8.1414. [DOI] [PubMed] [Google Scholar]
- Hyman SE. The neurobiology of addiction: Implications for voluntary control of behavior. The American Journal of Bioethics (AJOB-Neuroscience) 2007;7(1):8–11. doi: 10.1080/15265160601063969. [DOI] [PubMed] [Google Scholar]
- Julien RM. A primer of drug action. 9. New York: Worth Publishers; 2001. [Google Scholar]
- Kaufman J, Ross T, Stein E, Garavan H. Cingulate hypoactivity in cocaine users during a GO-NOGO task as revealed by event-related functional magnetic resonance imaging. The Journal of Neuroscience. 2003;23:7839–7843. doi: 10.1523/JNEUROSCI.23-21-07839.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killias M, Aebi M, Ribeaud D. Effects of heroin prescription on police contacts among drug-addicts. European Journal on Criminal Policy and Research. 1998;6(3):433–438. [Google Scholar]
- Koob GF, Le Moal M. Plasticity of reward neurocircuitry and the ‘dark side’ of drug addiction. Nature Neuroscience. 2005;8:1442–1444. doi: 10.1038/nn1105-1442. [DOI] [PubMed] [Google Scholar]
- Koob GF, Sanna PP, Bloom FE. Neuroscience of addiction. Neuron. 1998;21(3):467–476. doi: 10.1016/s0896-6273(00)80557-7. [DOI] [PubMed] [Google Scholar]
- Lasnier B, Brochu S, Boyd N, Fischer B. A heroin prescription trial: Case studies from Montreal and Vancouver on crime and disorder in the surrounding neighbourhoods. International Journal of Drug Policy. 2009 doi: 10.1016/j.drugpo.2009.04.003. in press. [DOI] [PubMed] [Google Scholar]
- Lauer RH, Lauer JC. Social problems and the quality of life. 8. New York: McGraw Hill Higher Education; 2002. [Google Scholar]
- Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278:45–57. doi: 10.1126/science.278.5335.45. [DOI] [PubMed] [Google Scholar]
- Levy N. Autonomy and addiction. Canadian Journal of Philosophy. 2006;36(3):427–448. [Google Scholar]
- Levy N. Neuroethics: Challenges for the 21st century. New York: Cambridge University Press; 2007a. [Google Scholar]
- Levy N. The social: A missing term in the debate over addiction and voluntary control. American Journal of Bioethics. 2007b;7:35–36. doi: 10.1080/15265160601064173. [DOI] [PubMed] [Google Scholar]
- Li CS, Sinha R. Inhibitory control and emotional stress regulation: neuroimaging evidence for frontal-limbic dysfunction in psycho-stimulant addiction. Neuroscience and Biobehavioral Reviews. 2008;32:581–597. doi: 10.1016/j.neubiorev.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lines R, Elliott R. Injecting drugs into human rights advocacy. International Journal of Drug Policy. 2007;18:453–457. doi: 10.1016/j.drugpo.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Loewenstein G. Willpower: A decision theorist’s perspective. Law and Philosophy. 2000;19:51–76. [Google Scholar]
- Mehta S, Farina A. Is being sick really better? Effect of the disease view of mental disorder on stigma. Journal of Social and Clinical Psychology. 1997;16(4):405–419. [Google Scholar]
- Merton RK. Social problems and sociological theory. In: Merton RK, Nisbet RA, editors. Contemporary Social Problems. New York: Harcourt; 1961. pp. 697–737. [Google Scholar]
- Miller WR, Carroll KM. Drawing the science together: Ten principles, ten recommendations. In: Miller WR, Carroll KM, editors. Rethinking substance abuse: What the science shows, and what we should do about it. New York: The Guilford Press; 2006. pp. 293–311. [Google Scholar]
- Morse SJ. Voluntary control of behavior and responsibility. The American Journal of Bioethics. 2007;7(1):12–36. doi: 10.1080/15265160601063993. [DOI] [PubMed] [Google Scholar]
- Oviedo-Joekes E, Nosyk B, Brissette S, Chettiar J, Schneeberger P, Marsh DC, et al. The North American opiate medication initiative (NAOMI): Profile of participants in North America’s first trial of heroin-assisted treatment. Journal of Urban Health. 2008;85(6):812–825. doi: 10.1007/s11524-008-9312-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oviedo-Joekes E, Nosyk B, Marsh DC, Guh D, Brissette S, Gartry C, et al. Scientific and political challenges in North America’s first randomized controlled trial of heroin assisted treatment for severe heroin addiction: Rationale and design of the NAOMI study. Clinical Trials. 2009;6(3):261–271. doi: 10.1177/1740774509105222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan J, Yang L, Cruz-Rojas R. Effects of attributing serious mental illnesses to genetic causes on orientations to treatment. Psychiatric Services. 2006;57:382–387. doi: 10.1176/appi.ps.57.3.382. [DOI] [PubMed] [Google Scholar]
- Racine E, Bar-Ilan O, Illes J. fMRI in the public eye. Nature Reviews Neuroscience. 2005;6(2):159–164. doi: 10.1038/nrn1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raphael D. Introduction to the social determinants of health. In: Raphael D, editor. Social determinants of health: Canadian perspectives. Toronto: Canadian Scholars’ Press Inc; 2004. [Google Scholar]
- Read J. Why promoting biological ideology increases prejudice against people labelled “schizophrenic”. Australian Psychologist. 2007;42(2):118–128. [Google Scholar]
- Read J, Haslam N, Sayce L, Davies E. Prejudice and schizophrenia: A review of the ‘mental illness is an illness like any other’ approach. Acta Psychiatrica Scandinavica. 2006;114:303–318. doi: 10.1111/j.1600-0447.2006.00824.x. [DOI] [PubMed] [Google Scholar]
- Rehm J, Fischer B. Should heroin be prescribed to heroin misusers? Yes. British Medical Journal. 2008;336(7635):70. doi: 10.1136/bmj.39421.593692.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinarman C, Cohen PD, Kaal HL. The limited relevance of drug policy: Cannabis in Amsterdam and in San Francisco. American Journal of Public Health. 2004;94:836–842. doi: 10.2105/ajph.94.5.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush B, Urbanoski K, Bassani D, Castel S, Wild TC, Strike C, Kimberly D, Somers J. Prevalence of co-occurring substance use and other mental disorders in the Canadian population. Canadian Journal of Psychiatry. 2008;53(12):800–809. doi: 10.1177/070674370805301206. [DOI] [PubMed] [Google Scholar]
- Russell B. Patient autonomy writ large. The American Journal of Bioethics. 2009;9(2):32–34. doi: 10.1080/15265160802654244. [DOI] [PubMed] [Google Scholar]
- Satel SK. What should we expect from drug abusers? Psychiatric Services. 1999;50:861. doi: 10.1176/ps.50.7.861. [DOI] [PubMed] [Google Scholar]
- Searle JR. Freedom and neurobiology. New York: Columbia University Press; 2004. [Google Scholar]
- Sherwin S. A relational approach to autonomy in health care. In: Sherwin S, editor. The Politics of Women’s Health: Exploring agency and autonomy. Philadelphia: Temple University Press; 1998. pp. 19–47. [Google Scholar]
- Shiloh S, Rashuk-Rosenthal D, Benyamini Y. Illness causal attributions. An exploratory study of their structure and associations with other illness cognitions and perceptions of control. Journal of Behavioral Medicine. 2002;25:373–394. doi: 10.1023/a:1015818532390. [DOI] [PubMed] [Google Scholar]
- Sinha R, Li CSR. Imaging stress- and cue-induced drug and alcohol craving: Association with relapse and clinical implications. Drug and Alcohol Review. 2007;26:25–31. doi: 10.1080/09595230601036960. [DOI] [PubMed] [Google Scholar]
- Soon CS, Brass M, Heinze HJ, Haynes JD. Unconscious determinants of free decisions in the human brain. Nature Neuroscience. 2008;11(5):543–545. doi: 10.1038/nn.2112. [DOI] [PubMed] [Google Scholar]
- Strike CJ, Myers T, Millson M. Finding a place for needle exchange programs. Critical Public Health. 2004;14(3):261–275. [Google Scholar]
- Taylor C. Sources of the self: The making of modern identity. Cambridge: Harvard University Press; 1989. [Google Scholar]
- Thomas YF. The social epidemiology of drug abuse. American Journal of Preventive Medicine. 2007;32(6S):S141–S146. doi: 10.1016/j.amepre.2007.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhl G, Drgon T, Johnson C, Liu Q-R. Addiction genetics and pleiotropic effects of common haplotypes that make polygenic contributions to vulnerability to substance dependence. Journal of Neurogenetics. 2009 doi: 10.1080/01677060802572929. [Epub ahead of Print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdejo-Garcia A, Bechara A. A somatic marker theory of addiction. Neuropharmacology. 2009;56:48–62. doi: 10.1016/j.neuropharm.2008.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N, Li TK. The neuroscience of addiction. Nature Neuroscience. 2005;8:1429–1430. doi: 10.1038/nn1105-1429. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ, Baler R, Telang F. Imaging dopamine’s role in drug abuse and addiction. Neuropharmacology. 2009;56:3–8. doi: 10.1016/j.neuropharm.2008.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace JJ. The social ecology of addiction: Race, risk and resilience. Pediatrics. 1999;103:1122–1127. [PubMed] [Google Scholar]
- Wallace JJ, Bachman J, O’Malley P, Johnston L, Schulenberg J, Cooper S. Tobacco, alcohol, and illict drug use: Racial and ethnic differences among U.S. high school seniors, 1976–2000. Public Health Reports. 2002;117(suppl 1):S67–S75. [PMC free article] [PubMed] [Google Scholar]
- Weiss F. Neurobiology of craving, conditioned reward and relapse. Current Opinion in Pharmacology. 2005;5:9–19. doi: 10.1016/j.coph.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Wegner D. The illusion of conscious will. Cambridge: MIT Press; 2002. [Google Scholar]
- Xu Z, Hou B, Gao Y, He F, Zhang C. Effects of enriched environment on morphine-induced reward in mice. Experimental Neurology. 2007;204(2):714–719. doi: 10.1016/j.expneurol.2006.12.027. [DOI] [PubMed] [Google Scholar]


