Abstract
Ivermectin (IVM) is exceptionally safe in humans, and is used for mass treatment of onchocerciasis and lymphatic filariasis. However, cases of encephalopathy, sometimes fatal, have been reported in a small number of individuals who harbored large numbers of Loa loa microfilariae (mf). A loss-of-function mutation in the mdr-1 gene in some dog breeds and in mice leads to accumulation of the drug in the brain, causing coma and death. This hypothesis was tested in four individuals from Cameroon who experienced a post-IVM serious adverse event (SAE) and in nine non-SAE matched controls. No loss-of-function mutation was detected in mdr-1 in any subject. However, haplotypes, associated with altered drug disposition, were present as homozygotes in two of the SAE patients (50%), but absent as homozygotes in the controls (0%). An association of high Loa mf load and a genetic predisposition to altered IVM distribution could be involved in IVM SAEs.
Introduction
The filarial nematode Onchocerca volvulus causes a disease called onchocerciasis in humans. The parasite is found mostly in sub-Saharan Africa and parts of Latin America. Mass distribution of the anthelmintic drug ivermectin (Mectizan®, Merck & Co., Whitehouse Station, NJ) to human populations living in endemic areas is the mainstay of current programs for the control of onchocerciasis. In Africa, lymphatic filariasis control is conducted using ivermectin (IVM) and albendazole in combination. Ivermectin has been reported to be exceptionally safe for this indication.1 However, instances of serious adverse events (SAEs) have been reported in a small number of people who harbored high densities of larval stages (microfilariae, [mf]) of another filarial species, Loa loa, in the blood (polyparasitism is common in people who live in O. volvulus-endemic regions). Most of these reports have been from Cameroon and the Democratic Republic of Congo.2,3 The pathophysiological and/or pharmacological basis for these rare but potentially fatal neurological SAEs is not fully understood.2,4,5 It is critical to define the mechanism(s) associated with SAEs because it may provide information on the optimal management of the cases and/or lead to the development of tools enabling identification of individuals at risk for SAEs.6 Similar concerns pertain to lymphatic filariasis control programs, which have yet to be implemented in areas where loiasis is co-endemic.
The risk of developing an SAE after IVM treatment is related to the load of L. loa mf (> 30,000 mf/mL blood) before treatment.7 In a population where the prevalence of L. loa microfilaremia is 40%, 5% of individuals will harbor more than 30,000 mf/mL.8,9 Even among the latter, relatively few will develop an SAE. In this regard, cofactors not yet characterized might play a role in the appearance of the neurological reaction in an individual.6 Potential cofactors include immune or physiological host factors. For example, at the level of the brain capillaries, L. loa co-infection with other pathogens (e.g., Plasmodium sp., O. volvulus, or others) might produce specific inflammatory damage that predisposes individuals to the development of neurological SAE after IVM treatment.
An additional possible explanation for the SAE is evident in the pharmacology of IVM. The drug is safe in humans because, when given at therapeutic doses, it is excluded from the central nervous system (CNS) by the blood-brain barrier.10 Accumulation of IVM in the brain as a consequence of massive overdoses (more than 100 times the normal doses) is associated with prolonged coma and death in humans.11 In addition, IVM is commonly used in veterinary medicine for the prevention of Dirofilaria immitis infection in dogs,12 and it has been known for some time that a few breeds of dogs, especially collies, are highly sensitive to IVM toxicity.13 This phenotype is caused by a loss-of-function mutation in a P-glycoprotein (pgp) gene called mdr-1 (ABCB1).14 This loss of function is brought about by a homozygous 4-bp deletion in the coding region of the mdr-1 gene, which results in a frame shift causing a nonsense and truncated (caused by insertion of stop codons in the frame-shifted DNA sequence) protein sequence. Collies, homozygous for the null allele, are highly sensitive to IVM and a few other drugs (notably loperamide). The pgp pump performs the primary xenobiotic exclusionary role of the blood-brain barrier. Mdr-1 encodes a protein of 1,280 amino-acids in 28 exons. It is located on chromosome 7q21.1 in humans.15
The possibility that a similar, rare and geographically restricted loss-of-function mutation exists in humans must be considered.16 A potential explanation for IVM-associated SAEs in Cameroon is that the drug penetrates into extra-vascular brain tissue in affected individuals. In these cases, high levels of IVM in the brain could cause SAEs through two possible mechanisms: either by a direct CNS-based toxicity of the drug (IVM has affinity for GABA-gated chloride channels),17 and/or by drug-induced killing of L. loa mf asymptomatically present in the brain parenchyma before treatment. The spontaneous existence of such L. loa mf in the brain tissue has been described in detail in one instance.18 In addition to possible effects of a null allele; other alterations in the mdr-1 gene could have more general effects on the pharmacokinetics of IVM. The plausibility of this scenario is enhanced by the pharmacogenetic precedent of the Δmdr-1 phenotype in dogs and because coma is a known outcome of IVM accumulation in the brain. Analyzing mdr-1 genotypes in SAE cases could rule out a null allele possibility and thus a study was conducted in Cameroon to address the issue.
Materials and Methods
Patients.
Ethical approval for this study was granted by the Cameroon Ministry of Public Health, the National Ethics Committee of Cameroon, and the Research Ethics Committee of McGill University (Montreal, Canada). The objective of the study was explained to the individuals before they agreed to participate and sign a consent form. Four individuals who survived an SAE after IVM treatment were selected by the physician in charge of the surveillance of the SAE cases in Cameroon (JK). Nine Cameroonian individuals who had never experienced an SAE were matched with the cases on sex, age, and village of residence. The patients were examined to ensure there was no condition that would make the patient unsuitable to donate 10 mL of blood. Each individual was sampled with a sterile vacutainer unit. Blood samples were labeled and processed under a code, which was not disclosed to the laboratory in which sequence information was determined.
Leukocyte RNA extraction and cDNA synthesis.
The mdr-1 gene is expressed in peripheral blood leukocytes.19,20 Leukocytes were obtained from each sample with a LeukoLOCK system kit (Ambion, Inc., Austin, TX). In Cameroon, blood samples were passed through the LeukoLOCK filter using an evacuated tube as a vacuum source. Filters were flushed with phosphate buffered saline (PBS) and leukocyte RNA was stabilized by the addition of RNAlater reagent (Ambion, Inc.). Samples were shipped to the Institute of Parasitology (McGill University, Montreal, Canada) on dry ice for completion of RNA extraction according to the manufacturer's protocol. Conversion to complementary DNA (cDNA) was performed using a QuantiTech reverse transcription kit (Qiagen Inc., Mississauga, Canada), according to the manufacturers protocol.
Mdr amplification and sequence analysis.
The complete open reading frame (ORF) of the mdr-1 cDNA was amplified from the cDNA samples by polymerase chain reaction (PCR) using 10 sets of overlapping primers (Table 1) designed based on GenBank deposited sequence NM 000927.3. The PCR amplification was confirmed by gel electrophoresis. The PCR products were sequenced using the 3730XL DNA Analyser system (McGill University/Genome Quebec Innovation Center). High Fidelity Platinum Taq DNA polymerase (Invitrogen, Burlington, ON, Canada) was used in the PCR reaction to minimize the introduction of errors during amplification. Each chromatogram was analyzed, in a blinded manner, with Sequencher 4.7 software (Gene Codes Corporation, Ann Arbor, MI). This program allowed us to discriminate at each nucleotide and select for only secondary peaks, which were more than 90% of the major nucleotide peaks on the chromatogram. This high level of discrimination provided confidence in determining homozygosity and heterozygosity at the polymorphic positions.
Table 1.
Primers used to amplify the complete open reading frame of mdr-1
| Fragments | Sense primers 5′–3′ | Antisense primers 5′–3′ |
|---|---|---|
| A | ATGGATCTTGAAGGGGACCGC | ATCGTGCACATCAAACCAGCC |
| B | GGTTGCTGCTTACATTCAGG | CCTATAGAAATATTGGCTGTAATAGC |
| C | CTGGAGCAGTAGCTGAAGAGG | GCACCTTCAGGTTCAGACCC |
| D | CCAAGTATTGACAGCTATTCG | CTGCCCACCACTCAACTGG |
| E | GTCACCATGGATGAGATTGAG | GATCCACGGACACTCCTACG |
| F | CGATGATGGAGTCATTGTGG | CGCTTGGTGAGGATCTCTCC |
| G | TACAAGAATTGATGATCCTG | GTACCTGCAAACTCTGAGC |
| H | GGGAAGATCGCTACTGAAGC | CCAGGCTCAGTCCCTGAAGC |
| I | GACAGCTACAGCACGGAAGG | GCTGTCTAACAAGGGCACGAGC |
| J | GCCAACATACATGCCTTCATCG | CACTGGCGCTTTGTTCCAGC |
Results
The complete ORF of the mdr-1 cDNA was amplified, in a blinded manner, for the 13 individuals included in the study. No loss-of-function mutation was found in any individual examined. However, polymorphism was found at cDNA positions T282C, A781G, C1236T, C3151G, and C3435T (Table 2). T282C is located between transmembrane domain 1 (TM1) and TM2, A781G between TM4 and TM5, C1236T between TM6 and the nucleotide binding domain 1, C3151G between TM12 and the nucleotide binding domain 2, and C3435T near the nucleotide binding domain 2 (Figure 1).21 Polymorphism at positions T282C, C1236T, and C3435T did not induce an amino acid change. However, the polymorphism at position A781G induced an amino acid change from isoleucine to valine, and the polymorphism at position C3151G induced an amino acid change from proline to alanine.
Table 2.
mdr-1 polymorphisms in the 13 individuals*
| Patient | SAE | T282C | A781G | C1236T | C3151G | C3435T |
|---|---|---|---|---|---|---|
| 1 | No | T/T | A/A | C/C | C/C | C/C |
| 2 | No | T/T | A/A | C/C | C/G | C/C |
| 3 | No | C/C | A/A | C/C | C/C | C/C |
| 4 | No | T/T | A/A | C/C | C/C | C/T |
| 5 | No | T/T | A/A | C/T | C/C | T/T |
| 6 | No | T/T | A/A | C/C | C/C | C/C |
| 7 | No | T/T | A/A | C/C | C/C | C/C |
| 8 | No | T/T | A/A | C/T | C/C | T/T |
| 9 | No | T/T | A/G | C/T | C/C | C/T |
| 10 | Yes | T/T | A/A | T/T | C/C | T/T |
| 11 | Yes | T/T | A/A | T/T | C/C | T/T |
| 12 | Yes | T/T | A/A | CC | C/C | C/C |
| 13 | Yes | T/T | A/A | CC | C/C | C/C |
SAE = serious adverse event.
Figure 1.
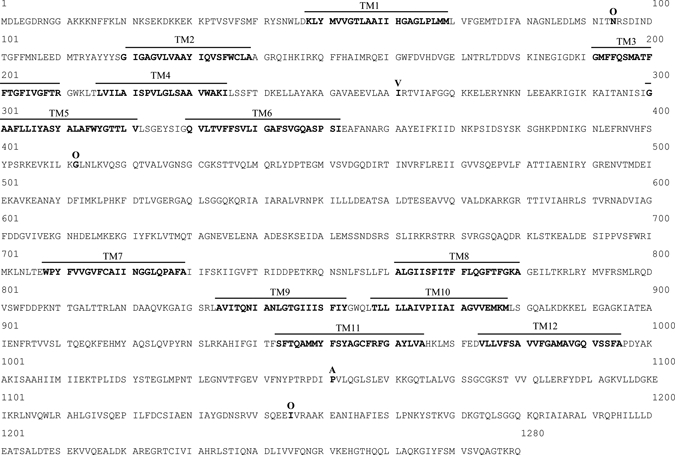
Location of the single nucleotide polymorphisms (SNPs) in the mdr-1 protein sequence. TM is used for transmembrane domain. Letter O located on the top of the protein sequence represents a silent mutation. Letters V and A are used for valine and alanine, respectively. The letters are located on the top of the protein sequence and they represent amino acid changes in the protein sequence caused by single nucleotide polymorphism at cDNA positions 781 and 3151, respectively.
The code was disclosed after the sequences were determined. It was found that no single nucleotide polymorphism (SNP) was uniformly associated with SAE cases. However, haplotypes (1236T and 3435T), associated with altered drug disposition (see Discussion), were present as homozygotes in two of the four SAE patients (50%), but absent as homozygotes in the controls (0%) (Table 2).
Discussion
The primary objective of this study was to determine if a loss-of-function mutation in mdr-1 could account for IVM SAEs. This objective has been met with a conclusion that there was no evidence that a loss-of-function mutation existed in any of the subjects. However, some interesting polymorphism was observed in the mdr-1 cDNA.
The mdr-1 gene is expressed in several tissues, including the intestine, kidney, placenta, liver, capillary endothelial cells of testis, adrenal gland, and the brain.10,22–24 So far, around 50 SNPs have been reported in the human mdr-1 gene, of which, some, such as C3435T, have been studied extensively. This SNP, although synonymous, has been reported to influence mdr-1 expression in different human tissues. However, the studies published regarding the effect of this SNP on response to different drugs are not always consistent.21,25
In our study, it was found that no SNP in the mdr-1 cDNA was uniformly associated with SAE after IVM treatment. The mdr-1 gene product plays an important role in the bioavailability of many drugs, and it is known that different ethnic groups respond differently to some drugs, possibly caused by differences in mdr-1 expression and/or sequence.26 Furthermore, the distribution of the C3435T SNP has been found to be influenced by ethnicity.27 West African populations have been reported to have a high frequency of the C/C genotype at position 3435 compared with other ethnic groups. It has been reported that 10% to 17% of the Ghanaian population,27,28 14% of the Beninese population,26 and 27% of the Sudanese population,27 carried the allele T at position 3435. In our study, the frequency of allele T was significantly higher than expected (38.5% P = 0.0002 with Ghanaian, P = 0.003 with Beninese). Interestingly, cases of SAE have been reported from Sudan, where the frequency of allele T is higher than in West Africa. As noted, the C3435T polymorphism is reported to be correlated with mdr-1 expression. Individuals with T/T genotype are reported to have lower expression of mdr-1 in intestinal epithelial cells,29 lymphoid cells, and placenta,30 than those with genotype C/C. This can lead to a difference in drug distribution.31 If a similar reduced expression occurs in the blood-brain barrier, it could result in excessive penetration of a drug into the CNS which, in the presence of a high number of L. loa microfilariae, may be responsible for adverse effects. In our study, two of the four individuals who had developed an IVM-related SAE had the 3435T/T genotype. It is also important to highlight the SNP at position 1236. Anglicheau and others32 reported that patients with the 1236CC genotype in mdr-1 had slightly but significantly lower dose-adjusted peak cyclosporin blood concentrations (−16%) (P < 0.02) and area under the curve (AUC) values (−14%) (P < 0.05) compared with 1236TT genotype carriers. Cyclosporin is a well-known substrate for MDR-1. These blood pharmacokinetic differences, even if small and measured only in the blood, may indicate the potential for significant consequences for drug concentration in the CNS, given the key role of MDR in restricting IVM access to the brain. Interestingly, two of the four SAE patients were homogygous T/T at 1236, and the three control individuals that carried the T allele were heterozygous C/T. The 1236T/2677G/3435T haplotype had been shown to have a positive association in reducing renal clearance of irinotecan, administrated intravenously.33 However, an association between this haplotype and the disposition of other drugs has not always been found.21 We did not find polymorphism at position 2677; all individuals were GG. Mdr-1 haplotypes involving C1236T, G2677T/A, and C3435T have been found to be influenced by ethnicity.26 In Benin, the 1236C/2677G/3435C haplotype is the wild-type and was present in 79.3% of the population and the TGT haplotype had a frequency of 7.5%, whereas in our Cameroonian group, the CGC haplotype was present at an allele frequency of approximately 62% of the total population tested (control + SAE patients) and the TGT haplotype had an allele frequency of approximately 27%. More interestingly, the homozygous TGT haplotype was present in 0% in the controls (non-SAE patients), but in 50% in the SAE patients. Using Fisher's exact test this difference is near the limit of significance (P = 0.077). However, it must be remembered that only four SAE patients were included. It is possible that in the two SAE patients who did not show the homozygous TGT haplotype there may be other polymorphisms, not detected by sequencing cDNA, which could affect the MDR-1 expression level.
Synonymous polymorphisms such as the SNPs at position 1236, 3435, or elsewhere in the sequence of mdr-1 may influence the functioning of the protein resulting from this ABC transporter gene.21 Recently, Sauna and others34 examined how the synonymous SNPs 1236C > T and 3435C > T might alter the functioning of human MDR-1 and have found that the 3435C > T is the key polymorphism linked to a functional change in P-glycoprotein. They showed by the use of the conformation-sensitive antibody, UIC2 against P-glycoprotein, and limited trypsin digestion that there were differences in the three-dimensional structure between the wild-type and the uncommon P-glycoprotein haplotype. This may result in a translational pause (where the synonymous codons change from frequently used to those rarely found in humans) during processing of the RNA through the ribosome, which alters the folding of the amino acid sequence with consequent effects on the functioning of the MDR-1 transporter.35
Our study was limited to four individuals that survived SAE and to the analysis of the coding region of the mdr-1 gene. Although IVM SAEs are rare and it is difficult to obtain tissue samples from SAE cases, it may be desirable to extend the study to more cases; if possible, a blood sample should be obtained from each new case of SAE and stored for subsequent analysis. Moreover, more information may be gained by investigating non-coding SNPs in introns or in the 5′ upstream or 3′ untranslated region, and by measuring mdr-1 expression in SAE patients. Uhr and others36 reported polymorphisms in an intron of the mdr-1 gene that can predict the response to antidepressant treatment with drugs previously identified as substrates of MDR-1.
From our data, it is difficult to reach definitive conclusions about the polymorphisms found in the SAE survivors, as there was no SNP detected only in the individuals who survived SAE. Four SAE survivors were examined, which is the equivalent of eight mdr-1 alleles. It is apparent that a deletion mutation like that observed in some canines is not present in these patients, and no other obvious loss-of-function mutation is evident in the coding region of mdr-1. However, there are intriguing genetic differences in mdr-1 between the SAE patients and the controls.
In humans, in addition to mdr-1, bcrp, mrp-1, mrp-2, and mrp-4 are all expressed at the luminal membrane of the brain capillary endothelial cells.37,38 It is not known which of these ABC transporters might be important in regulating the concentration of IVM that reaches brain tissue in humans. In mice, mdr-1 appears to be the dominant transporter regulating efflux of IVM across the blood-brain barrier.39 Nevertheless, there is evidence that the location and functioning of some ABC transporters may differ between humans and mice.39 The IVM profoundly inhibits human BCRP-mediated transport of mitoxantrone and other BCRP substrates, whereas polymorphisms in human bcrp have been shown to affect the disposition of a number of lipophilic drugs.40 Furthermore, it has recently been shown that IVM is actively transported by BCRP and that BCRP inhibitors increased IVM basolateral-apical permeability in Caco-2 cells overexpressing BCRP, suggesting a possible role for BCRP in regulating IVM tissue concentrations. In mdr1ab−/− mice, the BCRP inhibitor Ko143 significantly increased IVM concentrations in the brain.41 The BCRP transport of IVM could be important in the context of the SAEs observed in patients with high L. loa microfilaremia after IVM treatment, as Poller and others42 have observed that during inflammatory reactions, which can be associated with an altered blood-brain barrier, elevated levels of pro-inflammatory cytokines such as interleukin (IL)-1β, IL-6, and tumor necrosis factor α (TNF-α) can significantly reduce BCRP messenger RNA (mRNA) and protein levels, possibly increasing penetration of BCRP substrates into the brain. Future research should analyze non-coding polymorphisms in bcrp, and polymorphisms and/or changes in activity of other blood-brain ABC transporters, such as MRP-1. If possible, the number of SAE and non-SAE samples analyzed in future research should be increased. The need remains to find the pathophysiological cause of SAEs after IVM treatment to enable IVM to be safely administered in loiasis co-endemic regions for onchocerciasis and lymphatic filariasis control.
Acknowledgments
We thank the individuals that participated in this study.
Footnotes
Financial support: This study was supported by a Canadian Institutes of Health grant to RKP and by Mectizan Donation Program as part of their support to the Filariasis Research Center in Yaoundé (JK).
Authors' addresses: Catherine Bourguinat, Roger K. Prichard, and Timothy G. Geary, Institute of Parasitology, McGill University, Quebec, Canada, E-mail: roger.prichard@mcgill.ca. Joseph Kamgno, Filariasis Research Centre and Faculty of Medicine and Biomedical Sciences University of Yaoundé I, Yaoundé, Cameroon. Michel Boussinesq, Unité Mixte de Recherche 145, Institut de Recherche pour le Développement and Université Montpellier 1, Montpellier Cedex 5, France. Charles D. Mackenzie, Filarial Diseases Unit, Michigan State University, East Lansing, MI.
References
- 1.Dull HB, Meredith SE. The Mectizan Donation Programme–a 10-year report. Ann Trop Med Parasitol. 1998;92:69–71. [PubMed] [Google Scholar]
- 2.Boussinesq M, Gardon J, Gardon-Wendel N, Chippaux JP. Clinical picture, epidemiology and outcome of Loa-associated serious adverse events related to mass ivermectin treatment of onchocerciasis in Cameroon. Filaria J. 2003;2((Suppl 1)):S4. doi: 10.1186/1475-2883-2-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Twum-Danso NA. Loa loa encephalopathy temporally related to ivermectin administration reported from onchocerciasis mass treatment programs from 1989 to 2001: implications for the future. Filaria J. 2003;2((Suppl 1)):S7. doi: 10.1186/1475-2883-2-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mackenzie CD, Geary TG, Gerlach JA. Possible pathogenic pathways in the adverse clinical reactions seen following ivermectin administration to onchocerciasis patients. Filaria J. 2003;2((Suppl 1)):S5. doi: 10.1186/1475-2883-2-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boussinesq M, Kamgno J, Pion SD, Gardon J. What are the mechanisms associated with post-ivermectin serious adverse events? Trends Parasitol. 2006;22:244–246. doi: 10.1016/j.pt.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 6.Mackenzie CD, Geary T, Prichard R, Boussinesq M. Where next with Loa loa encephalopathy? Data are badly needed. Trends Parasitol. 2007;23:237–238. doi: 10.1016/j.pt.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 7.Gardon J, Gardon-Wendel N, Demanga-Ngangue Kamgno J, Chippaux JP, Boussinesq M. Serious reactions after mass treatment of onchocerciasis with ivermectin in an area endemic for Loa loa infection. Lancet. 1997;350:18–22. doi: 10.1016/S0140-6736(96)11094-1. [DOI] [PubMed] [Google Scholar]
- 8.Boussinesq M, Gardon J, Kamgno J, Pion SD, Gardon-Wendel N, Chippaux JP. Relationships between the prevalence and intensity of Loa loa infection in the Central province of Cameroon. Ann Trop Med Parasitol. 2001;95:495–507. doi: 10.1080/00034980120073184. [DOI] [PubMed] [Google Scholar]
- 9.Pion SD, Filipe JA, Kamgno J, Gardon J, Basáñez MG, Boussinesq M. Microfilarial distribution of Loa loa in the human host: population dynamics and epidemiological implications. Parasitology. 2006;133:101–109. doi: 10.1017/S0031182006000035. [DOI] [PubMed] [Google Scholar]
- 10.Cordon-Cardo C, O'Brien JP, Casals D, Rittman-Grauer L, Biedler JL, Melamed MR, Bertino JR. Multidrug-resistance gene (P-glycoprotein) is expressed by endothelial cells at blood–brain barrier sites. Proc Natl Acad Sci U S A. 1989;86:695–698. doi: 10.1073/pnas.86.2.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chung K, Yang CC, Wu ML, Deng JF, Tsai WJ. Agricultural avermectins: an uncommon but potentially fatal cause of pesticide poisoning. Ann Emerg Med. 1999;34:51–57. doi: 10.1016/s0196-0644(99)70271-4. [DOI] [PubMed] [Google Scholar]
- 12.McCall JW. The safety-net story about macrocyclic lactone heartworm preventives: a review, an update, and recommendations. Vet Parasitol. 2005;133:197–206. doi: 10.1016/j.vetpar.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 13.Paul AJ, Tranquilli WJ, Seward RL, Todd KS, Jr, DiPietro JA. Clinical observations in collies given ivermectin orally. Am J Vet Res. 1987;48:684–685. [PubMed] [Google Scholar]
- 14.Mealey KL. Therapeutic implications of the MDR-1 gene. J Vet Pharmacol Ther. 2004;27:257–264. doi: 10.1111/j.1365-2885.2004.00607.x. [DOI] [PubMed] [Google Scholar]
- 15.Ambudkar SV, Kimchi-Sarfaty C, Sauna ZE, Gottesman MM. P-glycoprotein: from genomics to mechanism. Oncogene. 2003;22:7468–7485. doi: 10.1038/sj.onc.1206948. [DOI] [PubMed] [Google Scholar]
- 16.Edwards G. Ivermectin: does P-glycoprotein play a role in neurotoxicity? Filaria J. 2003;2((Suppl 1)):S8. doi: 10.1186/1475-2883-2-S1-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bennett JL, Williams JF, Dave V. Pharmacology of ivermectin. Parasitol Today. 1988;4:226–228. doi: 10.1016/0169-4758(88)90163-9. [DOI] [PubMed] [Google Scholar]
- 18.Van Bogaert L, Dubois A, Janssens PG, Radermecker J, Tverdy G, Wanson M. Encephalitis in Loa-loa filariasis. J Neurol Neurosurg Psychiatry. 1955;18:103–119. doi: 10.1136/jnnp.18.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaudhary PM, Mechetner EB, Roninson IB. Expression and activity of the multidrug resistance P-glycoprotein in human peripheral blood lymphocytes. Blood. 1992;80:2735–2739. [PubMed] [Google Scholar]
- 20.Albermann N, Schmitz-Winnenthal FH, Z'graggen K, Volk C, Hoffmann MM, Haefeli WE, Weiss J. Expression of the drug transporters MDR1/ABCB1, MRP1/ABCC1, MRP2/ABCC2, BCRP/ABCG2, and PXR in peripheral blood mononuclear cells and their relationship with expression in intestine and liver. Biochem Pharmacol. 2005;70:949–958. doi: 10.1016/j.bcp.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 21.Leschziner GD, Andrew T, Pirmohamed M, Johnson MR. ABCB1 genotype and PGP expression, function and therapeutic drug response: a critical review and recommendations for future research. Pharmacogenomics J. 2007;7:154–179. doi: 10.1038/sj.tpj.6500413. [DOI] [PubMed] [Google Scholar]
- 22.Fojo AT, Ueda K, Slamon DJ, Poplack DG, Gottesman MM, Pastan I. Expression of a multidrug-resistance gene in human tumors and tissues. Proc Natl Acad Sci U S A. 1987;84:265–269. doi: 10.1073/pnas.84.1.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thiebaut F, Tsuruo T, Hamada H, Gottesman MM, Pastan I, Willingham MC. Cellular localization of the multidrug-resistance gene product P-glycoprotein in normal human tissues. Proc Natl Acad Sci USA. 1987;84:7735–7738. doi: 10.1073/pnas.84.21.7735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sugawara I, Kataoka I, Morishita Y, Hamada H, Tsuruo T, Itoyama S, Mori S. Tissue distribution of P-glycoprotein encoded by a multidrug resistant gene as revealed by a monoclonal antibody, MRK 16. Cancer Res. 1988;48:1926–1929. [PubMed] [Google Scholar]
- 25.Li YH, Wang YH, Li Y, Yang L. MDRl Gene polymorphisms and clinical relevance. Acta Genetica Sinica. 2006;33:93–104. doi: 10.1016/S0379-4172(06)60027-9. [DOI] [PubMed] [Google Scholar]
- 26.Allabi AC, Horsmans Y, Issaoui B, Gala JL. Single nucleotide polymorphisms of ABCB1 (MDR1) gene and distinct haplotype profile in a West Black African population. Eur J Clin Pharmacol. 2005;61:97–102. doi: 10.1007/s00228-004-0879-0. [DOI] [PubMed] [Google Scholar]
- 27.Ameyaw MM, Regateiro F, Li T, Liu X, Tariq M, Mobarek A, Thornton N, Folayan GO, Githang'a J, Indalo A, Ofori-Adjei D, Price-Evans DA, McLeod HL. MDRl pharmacogenetics: frequency of the C3435T mutation in exon 26 is significantly influenced by ethnicity. Pharmacogenetics J. 2001;11:217–221. doi: 10.1097/00008571-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Schaeffeler E, Eichelbaum M, Brinkmann U, Penger A, Asante-Poku S, Zanger UM, Schwab M. Frequency of C3435T polymorphism of MDR1 gene in African people. Lancet. 2001;358:383–384. doi: 10.1016/S0140-6736(01)05579-9. [DOI] [PubMed] [Google Scholar]
- 29.Brinkmann U, Eichelbaum M. Polymorphisms in the ABC drug transporter gene MDR1. Pharmacogenomics J. 2001;1:59–64. doi: 10.1038/sj.tpj.6500001. [DOI] [PubMed] [Google Scholar]
- 30.Hoffmeyer S, Burk O, von Richter O, Arnold HP, Brockmoller J, Johne A, Cascorbi I, Gerloff T, Roots I, Eichelbaum M, Brinkmann U. Functional polymorphisms of the human multidrug resistance gene: multiple sequence variations and correlation of one allele with P-glycoprotein expression and activity in vivo. Proc Nat1 Acad Sci U S A. 2000;97:3473–3478. doi: 10.1073/pnas.050585397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brinkmann U, Roots I, Eichelbaum M. Pharmacogenetics of the human drug-transporter gene MDR1: impact of polymorphisms on pharmacotherapy. Drug Discov Today. 2001;6:835–839. doi: 10.1016/s1359-6446(01)01892-x. [DOI] [PubMed] [Google Scholar]
- 32.Anglicheau D, Thervet E, Etienne I, Hurault De Ligny B, Le Meur Y, Touchard G, Büchler M, Laurent-Puig P, Tregouet D, Beaune P, Daly A, Legendre C, Marquet P. CYP3A5 and MDR1 genetic polymorphisms and cyclosporine pharmacokinetics after renal transplantation. Clin Pharmacol Ther. 2004;75:422–433. doi: 10.1016/j.clpt.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 33.Sai K, Kaniwa N, Itoda M, Saito Y, Hasegawa R, Komamura K, Ueno K, Kamakura S, Kitakaze M, Shirao K, Minami H, Ohtsu A, Yoshida T, Saijo N, Kitamura Y, Kamatani N, Ozawa S, Sawada J. Haplotype analysis of ABCB1/MDR1 blocks in a Japanese population reveals genotype-dependent renal clearance of irinotecan. Pharmacogenetics. 2003;13:741–757. doi: 10.1097/00008571-200312000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Sauna ZE, Kimchi-Sarfaty C, Ambudkar SV, Gottesman MM. Silent polymorphisms speak: how they affect pharmacogenomics and the treatment of cancer. Cancer Res. 2007;67:9609–9612. doi: 10.1158/0008-5472.CAN-07-2377. [DOI] [PubMed] [Google Scholar]
- 35.Kimchi-Sarfaty C, Oh JM, Kim IW, Sauna ZE, Calcagno AM, Ambudkar SV, Gottesman MM. A “silent” polymorphism in the MDR1 gene changes substrate specificity. Science. 2007;315:525–528. doi: 10.1126/science.1135308. [DOI] [PubMed] [Google Scholar]
- 36.Uhr M, Tontsch A, Namendorf C, Ripke S, Lucae S, Ising M, Dose T, Ebinger M, Rosenhagen M, Kohli M, Kloiber S, Salyakina D, Bettecken T, Specht M, Pütz B, Binder EB, Müller-Myhsok B, Holsboer F. Polymorphisms in the drug transporter gene ABCB1 predict antidepressant treatment response in depression. Neuron. 2008;57:203–209. doi: 10.1016/j.neuron.2007.11.017. [DOI] [PubMed] [Google Scholar]
- 37.Hori S, Ohtsuki S, Tachikawa M, Kimura N, Kondo T, Watanabe M, Nakashima E, Terasaki T. Functional expression of rat ABCG2 on the luminal side of brain capillaries and its enhancement by astrocytederived soluble factor(s) J Neurochem. 2004;90:526–536. doi: 10.1111/j.1471-4159.2004.02537.x. [DOI] [PubMed] [Google Scholar]
- 38.Nies AT, Jedlitschky G, König J, Herold-Mende C, Steiner HH, Schmitt HP, Keppler D. Expression and immunolocalization of the multidrug resistance proteins, MRP1-MRP6 (ABCC1-ABCC6), in human brain. Neuroscience. 2004;129:349–360. doi: 10.1016/j.neuroscience.2004.07.051. [DOI] [PubMed] [Google Scholar]
- 39.Geyer J, Gavrilova O, Petzinger E. Brain penetration of ivermectin and selamectin in mdr1a,b P-glycoprotein and bcrp-deficient knockout mice. J Vet Pharmacol Ther. 2009;32:87–96. doi: 10.1111/j.1365-2885.2008.01007.x. [DOI] [PubMed] [Google Scholar]
- 40.Merino G, Real R, Baro MF, Gonzalez-Lobato L, Prieto JG, Alvarez AI, Marques MM. Natural allelic variants of bovine ATP-binding cassette transporter ABCG2: increased activity of the Ser581 variant and development of tools for the discovery of new ABCG2 inhibitors. Drug Metab Dispos. 2009;37:5–9. doi: 10.1124/dmd.108.022715. [DOI] [PubMed] [Google Scholar]
- 41.Kis E, Lecoeur S, Menez C, Dupuy J, Kiki S, Krajcsi P, Alvinerie M, Lespine A. World Association for the Advancement of Veterinary Parasitology 22nd Conference. Calgary, Canada: 2009. p. 9. (The anthelmintic ivermectin: a substrate of breast-cancer resistant protein (BCRP)). Abstract CS2.4. [Google Scholar]
- 42.Poller B, Drewe J, Krähenbühl S, Huwyler J, Gutmann H. Regulation of BCRP (ABCG2) and P-glycoprotein (ABCB1) by cytokines in a model of the human blood-brain barrier. Cell Mol Neurobiol. 2010;30:63–70. doi: 10.1007/s10571-009-9431-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


