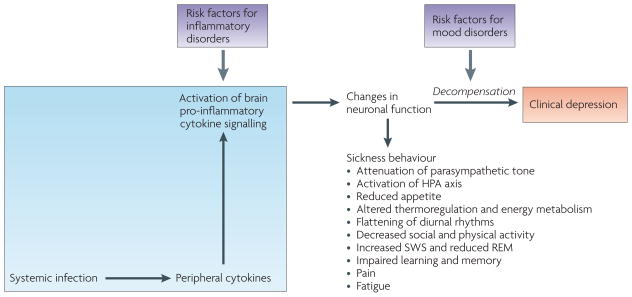
Figure 4. Depression as a consequence of decompensation of the mechanisms that regulate sickness.
Sickness behaviour in response to an infectious episode is normally reversible owing to the ability of the immune system to clear infectious pathogens and to the recovery mechanisms that oppose the production and action of pro-inflammatory cytokines, both in the periphery and the brain. Clinical evidence shows that depression can develop on a background of sickness with which it shares many of the neurovegetative and psychological components. Studies in animals show the same phenomenon. Decompensation of the mechanisms that regulate sickness behaviour can occur in vulnerable patients whose inflammatory response is more intense because the balance between pro- and anti-inflammatory mediators is shifted towards inflammation (for example, hyperproduction of tumour necrosis factor-α (TNF-α), insufficient production of interleukin (IL)-10 and glucocorticoid resistance). It can also occur in patients whose brain sensitivity to immune-mediated events is higher because of disturbed neurotransmitter metabolism, for example, less efficient serotonergic functioning owing to homozygosity for the short allele of the serotonin transporter gene. HPA, hypothalamus–pituitary–adrenal; SWS, slow-wave sleep; REM, rapid-eye movement sleep.