Abstract
Objectives
Urban/rural residence is a critical health determinant and one researchers have historically found to distinguish health experiences. In this study, we investigated variations in older adult mortality across urban and rural areas of China and assessed mechanisms driving an urban advantage through a series of socioeconomic and health service covariates measured at individual and community levels.
Methods
We employed 15 years of mortality data from the China Health and Nutrition Survey. We calculated average annual age-specific death rates and used combinations of covariates to examine Cox proportional hazards models. We employed the 2000 Chinese Census and the 2002 Demographic Yearbook descriptively to assess reliability and provide an alternative source for mortality variation.
Results
Hazard ratios and standardized death rates showed rural mortality to be about 30% higher than urban mortality. Cadre status, amenities within the community, and average wage within the community are important determinants of mortality, and adjusting for these covariates reduced the urban advantage.
Discussion
There is great differentiation in economic and social life between urban and rural China, and this appears to be negatively influencing survival chances of older adults in rural areas. The policy implications are fairly clear: Investment in rural China is needed to reduce health inequalities.
Place of residence has, for centuries, been implicated as a health determinant. In the developed world, differences in urban and rural health go back to medieval times when urban residence was harmful owing to communicable diseases more easily transferred across populations living in cramped and unclean surroundings (Kearns, 1988; Landers, 1987; National Research Council, 2003; Woods, 2003). Although more recent trends suggest less robust differentials, several studies have noted that an urban mortality advantage exists in the United States (Clifford & Brannon, 1985; Hayward, Pienta, & McLaughlin, 1997; House et al., 2000; Kitagawa & Hauser, 1973; Smith, Anderson, Bradham, & Longino, 1995). Yet very little research has examined urban/rural mortality trends in developing countries (Eastwood & Lipton, 2000; National Research Council, 2003). What research does exist suggests that public health factors, such as access to services and safe water, make living in a city in developing countries advantageous (National Research Council, 2003). Those living in urban areas are also thought to earn higher incomes and have higher education, factors considered to be robust predictors of health (Antonovsky, 1967; Mackenbach et al., 1997; Marmot, Shipley, & Rose, 1984; Preston & Taubman, 1994). As a result, life expectancy is higher in urban areas in developing countries (Andrews, 2001; Kinsella, 2001; Langmore, 2001; National Research Council, 2003). Yet evidence also shows higher risks for lifestyle-related diseases, such as diabetes and cardiovascular disease, beginning to arise in some urban areas in the developing world, and substantial intra-urban variations in health (Bradley, Stephens, Harpham, & Cairncross, 1992; Harpham & Tanner, 1995; Stephens, 1996; Zhai & McGarvey, 1992). Therefore, although the little research that exists does point to an urban advantage, the robustness of the association, whether it holds across the entire developing world, why it exists, and whether it will continue to hold into the future are all issues requiring further attention.
Studies of urban/rural health variations can be hampered by difficulties in defining urban and rural areas, which often encroach on one another. But in China, urban and rural distinctions are quite sharp due to legal designations implemented after the establishment of the People's Republic of China in 1949, most notably, the household registration system (Kirkby, 1985). Discrete economic, population, social, and health policies treated sectors differently, and advantages, including medical coverage and economic investment, accrued to urban areas and residents. If anything, the distinction has been widening, in part a byproduct of China's rapid economic development and subsequent differential investment (England, 2005). Urban China is experiencing a well-publicized boom while development in rural areas proceeds at a slower pace. The gap in health services has also widened. China's economic reform has ushered in a decline in cooperative medicine and an increase in privatized fee-for-service, which has changed the way health care is provided in rural areas and has resulted in expensive service and decreasing access (Beach, 2001; Chen, Hu, & Lin 1993; Meng, Liu, & Shi, 2000; Shi, 1996). In the meantime, most urban residents maintain subsidized care through insurance programs financed from the national budget, have access to qualified medical personnel, and can draw on an array of resources. There are indeed few places in the world where urban and rural differences in social and economic life are so severe, a reality that has prompted the Chinese government to announce a new focus on strategies aimed at reducing gaps in economic and social development (Kahn, 2004).
Growing social and economic disparities in China across urban and rural areas can intensify health inequalities already thought to exist. But studies that have attempted to quantify these inequalities are modest in number. Although researchers have reported an urban advantage, they have less frequently studied the mechanisms accounting for this advantage. However, investigators suspect, usually anecdotally, that these mechanisms include the higher socioeconomic status and consequent superior access to health service for people living in urban areas, and the fact that urban neighborhoods are wealthier and consequently offer superior availability of health services (Fang, 1993; S. Li & Sun, 2003; Lili, 1993; Zeng, 1990). This implies that mechanisms operate on two levels—individual and community. The current study examined urban/rural variation in mortality among those aged 50 and older in China. We asked the following research question: How great is the urban advantage, and to what extent is it accounted for by a series of individual- and community-level characteristics?
Methods
Data
Data were mainly from the China Health and Nutrition Survey (CHNS), a multiwave longitudinal survey. The CHNS currently consists of six waves (1989, 1991, 1993, 1997, 2000, and 2004). It employs a multistage random cluster sampling process to draw households from urban and rural areas in nine provinces (Guangxi, Guizhou, Heilongjiang, Henan, Hubei, Hunan, Jiangsu, Liaoning, and Shandong). Urban and rural definitions for the CHNS and consequently for the current study are based on those used for administrative purposes by the central government of China. The CHNS classifies cities and suburban areas, defined as metropolitan places with populations of at least 100,000, as urban locales and classifies other areas, including towns and farming areas, as rural locales. The current study was limited to household members aged 50 and older, and sample sizes ranged from about 2,700 to 3,800 across waves. Most households were followed up across all waves, but there were also deletions and additions based on community participation. Beginning in 1993, the CHNS added households in the sample areas that had been formed by individuals included in the previous waves. From 1997 onward, the survey added new households and communities to replace those no longer participating.
A community questionnaire, completed for each primary sampling unit by knowledgeable respondents, collected information on infrastructure, services, population, and wages. A household survey interviewed one household member but collected information about everyone in the household. The current analysis employed both demographic and roster information collected from each household member as well as information collected in the community module.
We accessed data, supporting documentation, and details on sampling through the Carolina Population Center Web site (http://www.cpc.unc.edu/projects/china). At the time of writing, the Web site listed more than 100 publications, few of which focused on older adults and none of which examined mortality. Thus, this is an underused resource for questions related to the health of older adults. Good examples of publications that provide additional information on the study include Bell, Ge, and Popkin (2001), Beydoun and Popkin (2005), Entwisle and Chen (2002), and Wang, Bentley, Zhai, and Popkin (2002).
Measuring and Analyzing Mortality
Although the CHNS was not designed to study mortality, such information is available from the household register completed at each follow-up. Individuals were listed as alive and present, moved, or died. If there was a move or a death, the month was recorded. Missing cases resulted from households not being contacted, which was mostly a function of the entire community no longer participating. Community dropouts were fairly evenly distributed across urban and rural settings (about 95% of communities covered were followed up over time in both urban and rural areas). For the current study, we organized information about household members into five episodes based on survey interval (1989–1991, 1991–1993, 1993–1997, 1997–2000, and 2000–2004) and aggregated the episodic data.
We determined exact age by date of birth and date of interview. An individual aged 48 at the time of interview in 1989 could, depending on his or her exact date of birth and interview, have entered the sample population for the second interval. In this way, individuals were aged in.
We examined urban/rural variation in mortality in two ways. We determined age-specific death rates, calculated as the average yearly rate within age category, for urban and rural areas. We compared death rates calculated from the CHNS to those published from the 2000 Chinese Census (CC) and the 2002 Demographic Yearbook (DY). Then we fitted Cox proportional hazards models to predict differential survival times across urban and rural areas. We fitted these models with the assumption that correlation between survival times within communities could be accounted for by an additional random frailty effect (Box-Steffensmeier & Jones, 2004; Goldstein, 2003; Hougaard, 1995; Pickles & Crouchley, 1995). This random effect is a variable, with a mean of 1 and variance of θ estimated by the data, representing the shared frailty common to individuals within communities. Using the standard error of θ, we determined whether the shared frailty was significant and therefore should not be ignored. The model was denoted as follows:
| (1) |
where i indicates 1 through n communities and j indicates 1 through n observations within communities. Therefore, h indicates the hazard of an individual within a specific community dying at any instant, α represents the shared community effect, and xijβ represents the effects (β) of independent covariates (x) for individuals within communities on survival time. We measured survival time as the number of months of observation from the start of an episode until death or censoring, with those surviving considered censored at time of follow-up and those moving censored at time of move (movers were very evenly distributed across urban and rural areas). We used the Breslow method for ties. We initially tested the suitability of this Cox model by graphing Kaplan–Meier and Nelson–Aalen estimators and interacting variables with time. We did not find that variables violated the proportionality assumption. Because standard errors of the hazard ratios were conditioned on θ, significance was robust to within-community correlation. We conducted the Cox hazards models and all other procedures using STATA 9.2 software.
Covariates
Individual characteristics came from the household survey and varied across individuals. Community characteristics came from the community survey and were constant across individuals within communities. In choosing covariates, we first considered speculation from previous literature that socioeconomic status and health service characteristics could explain an urban advantage. We operationalized this at an individual level as indicators of socioeconomic status and related access to health service. On a community level, we operationalized this as community economic status and related availability of health services. Because we used episodic information, we treated as time varying covariates that might have carried a different value for the same person or community over time.
As for individual level measures, we coded education as no formal, some primary, or completed primary and above. We coded occupation as white collar and skilled, unskilled or agricultural, and other. The “other” category included student, homemaker, no occupation, or other occupation unclassified or difficult to classify, but the category mostly consisted of an unstated occupation or never worked. An individual who was not currently working recorded their primary occupation if they had ever worked; therefore, no occupation only included those who had never worked. A cadre is a public official holding a responsible or managerial position in the party and government and therefore may have access to some privileges. The CHNS asked whether each household member was a cadre, and we coded this dichotomously. Following Filmer and Pritchett (2001) and Rutstein and Johnson (2004), we created an index for household wealth using a principal component technique and a series of survey questions about whether the following products were contained in the household: bicycle, motorbike, car, television, camera, fan, and radio. We subsequently divided ranked scores between 0 and 100 into quintiles when included in multivariate equations. We dichotomously coded having health insurance. In addition, in order to determine whether urban/rural differences in mortality were a function of health differences across place of residence, we also considered a measure of ill health, which came from a single item asking whether the older adult was currently in ill health or had been sick or injured within the 4 weeks preceding the interview. This was dichotomously measured.
There was a degree of interplay between the various individual-level measures. Having insurance is clearly a direct measure of health care access. Cadre status is directly linked to access through specific health care privileges granted to cadres, whereas the other measures are proximate. For instance, those with higher education likely have higher a greater understanding of the health care system. Household wealth relates to income that is necessary to purchase health care.
We considered four community characteristics. Number of amenities summed the following infrastructure items existing in the community: telegraph, telephone, post office, newspaper, movie theater, paved roads, and 24-hour electricity. Average wage for an ordinary male worker was reported in Yuan and logged. We imputed about 12% of cases with missing responses using related community variables. The other two measures were related to health services. We categorized a question for distance from the center of the community to the nearest health care facility (less than ½ km, ½ to 2 km, more than 2 km), and we included a separate code for a moderate number of nonresponses (about 15% of cases). We summed number of health care facilities in the community, eliminating any that were used solely for reproductive health care.
Results
Table 1 describes the episodic data. We based the analysis on an aggregated data set involving 15,267 persons aged 50 years or older at time of the household interview that began an episode. There were a total of 778 deaths. Table 2 provides descriptive information about the covariates by urban/rural residence. All except gender differed significantly across area. Whereas most socioeconomic measures displayed a consistent and significant urban advantage, persons in urban areas were more likely to have been reported sick or injured currently or in the 4 weeks preceding the interview.
Table 1.
China Health and Nutrition Survey Survival Information for the Sample Aged 50 and Older
| Survey Interval | Starting N | Survived, Lived in Same Residence at End of Interval | Survived, Moved Before End of Interval | Died | Status Unknown |
|---|---|---|---|---|---|
| 1989–1991 | 2,799 | 2,435 | 105 | 109 | 150 |
| 1991–1993 | 2,742 | 2,351 | 52 | 131 | 208 |
| 1993–1997 | 2,708 | 1,826 | 104 | 185 | 593 |
| 1997–2000 | 3,190 | 2,464 | 129 | 153 | 444 |
| 2000–2004 | 3,828 | 2,994 | 84 | 200 | 550 |
| Total | 15,267 | 12,070 | 474 | 778 | 1,945 |
Table 2.
Descriptive Information for Covariates by Rural/Urban Residence
| Covariate | Rural (N = 8,834) | Urban (N = 4,491) |
|---|---|---|
| Demographics | ||
| Mean age | 61.8 | 62.5*** |
| Gender (% male) | 48.5 | 47.1 |
| Individual | ||
| Education | ||
| % No education | 47.5 | 38.3*** |
| % Primary | 37.9 | 34.5*** |
| % More than primary | 14.7 | 27.1*** |
| Cadre status (% who is a cadre) | 2.4 | 7.6*** |
| Occupation | ||
| % White collar/skilled | 9.2 | 22.4*** |
| % Unskilled/agricultural | 65.3 | 38.6*** |
| % Never worked/other/missing | 25.5 | 39.0*** |
| Wealth (mean wealth score)a | 43.7 | 60.8*** |
| Insurance (% who have insurance) | 17.1 | 50.5*** |
| Community | ||
| Average wage (in Yuan) | 15.5 | 17.8*** |
| Number of amenities in community | 4.0 | 5.2*** |
| Mean number medical facilities in community | 2.1 | 3.0*** |
| Distance to nearest facility | ||
| % 0–.50 km | 40.7 | 35.3*** |
| % .51–2.00 km | 28.3 | 27.4 |
| % 2.01+ km | 22.7 | 21.3* |
| % Missing information | 8.4 | 15.9*** |
| Health (% in ill health) | 10.3 | 13.3*** |
Notes:
Wealth score divided into quintiles for multivariate analysis.
p < .10
p < .01, comparing urban and rural, two-tailed test.
Table 3 compares age-specific death rates for total, urban, and rural populations across three sources. We present the table first to establish reliability of the CHNS for measuring mortality and second, to provide an initial descriptive comparison of urban/rural mortality. Deaths in the DY, based on vital registration records, were not provided by urban/rural residence, so we present only the total for this source.
Table 3.
Age Specific Death Rates in China per 1,000 Population From Three Sources by Urban/Rural Residence
| CHNS |
2000 CCa |
DYb |
|||||
|---|---|---|---|---|---|---|---|
| Age | Total Population | Urban | Rural | Total Population | Urban | Rural | Total Population |
| 50–54 | 6.7 | 5.2 | 7.3 | 5.5 | 4.3 | 6.1 | 4.6 |
| 55–59 | 9.0 | 8.1 | 9.6 | 8.7 | 6.9 | 9.6 | 8.6 |
| 60–64 | 12.6 | 8.5 | 14.9 | 14.8 | 11.7 | 16.5 | 15.3 |
| 65–69 | 24.6 | 21.0 | 26.6 | 24.4 | 20.1 | 26.6 | 24.3 |
| 70–74 | 37.9 | 29.0 | 43.1 | 42.3 | 35.2 | 45.8 | 38.4 |
| 75–79 | 58.2 | 50.6 | 63.7 | 66.5 | 56.2 | 71.2 | 57.6 |
| 80 + | 121.7 | 120.9 | 124.9 | 134.5 | 117.0 | 142.8 | 117.7 |
| Standardized death ratec | 22.8 | 19.5 | 24.8 | 24.4 | 20.3 | 26.4 | 22.4 |
Notes: CHNS = China Health and Nutrition Survey; CC = 2000 Chinese Census; DY = 2002 Demographic Yearbook.
Source: China Data Center (2006), Tables 6a, 6b, 6c.
Source: United Nations (2002a), Tables 7 and 19.
Standardized death rate using the age composition of the total sample in the 2000 Census.
Death rates from the CHNS generally corresponded to those from the CC and DY. The bottom row of the table shows death rates for the population aged 50 and older standardized using a common age and gender distribution (from the CC). The standardized death rate from the CHNS, which was 22.8, was quite similar to that from the CC (24.4) and the DY (22.4). But we should note that additional analyses revealed that death rates from CHNS varied across intervals, from a standardized rate of about 19 to 29. Significant variation over intervals could be expected given the relatively small sample sizes upon which the death rate calculation in any interval was based. So, although individual intervals were not necessarily reliable, the aggregate of the intervals seemed to be. Age-specific death rates from the CHNS were also quite similar to those from the CC and DY.
Both the CHNS and the CC confirmed a substantially higher mortality rate in rural areas. We calculated standardized rates for urban areas to be 19.5 and 20.3 from the CHNS and CC, respectively, compared to 24.8 and 26.4 for rural areas. Thus, given similar age and gender distributions, we would expect about 30% more deaths among rural elders. Both the CHNS and CC data showed urban residents to be advantaged regardless of age group.
Table 4 presents hazard ratios from Cox proportional hazards models using shared frailty to account for a latent within-community random effect. The table provides the results of a number of models. Column 1 shows a base model that adjusted for age and gender. We tested several parameterizations for age and found the best to be a categorization into 5-year intervals. Column 2 presents the results of 10 models (i–x), each of which includes base plus one additional covariate. Column 3 simultaneously adjusts for individual- and community-level covariates. Column 4 adds a variable for ill health in order to determine whether the effect of urban/rural residence works indirectly through health. We further examined models that included various combinations of covariates, adjusted for age and gender, and monitored their impact on the urban/rural coefficient and the degree to which they influenced the −2 log likelihood, which we used to approximate the explanatory power of covariates. Column 5 shows a parsimonious model that included covariates that, when added, reduced the urban/rural coefficient and substantially increased the −2 log likelihood. Because there are clear expectations regarding associations (e.g., urban morality lower than rural, higher education associated with lower mortality), one-tailed tests of significance might be suitable. We report more the conventional two-tailed results but note significance up to p < .10.
Table 4.
Cox Models Showing Hazard Ratios for Dying (N = 13,325)a
| Base |
(i–x), Single Covariatesb |
Individual + Community Characteristics |
Adding Ill Health |
Parsimonious Modelc |
|
|---|---|---|---|---|---|
| Variable | 1 | 2 | 3 | 4 | 5 |
| Rural residence | 1.32** | 1.18 | 1.19* | 1.22** | |
| Age (ref = 50–54) | |||||
| 55–59 | 1.43* | 1.40** | 1.37* | 1.40** | |
| 60–64 | 2.01*** | 1.91*** | 1.86*** | 1.95*** | |
| 65–69 | 4.03*** | 3.77*** | 3.61*** | 3.82*** | |
| 70–74 | 6.37*** | 5.82*** | 5.55*** | 6.01*** | |
| 75–79 | 9.93*** | 8.81*** | 8.31*** | 9.17*** | |
| 80 + | 22.20*** | 19.05*** | 18.79*** | 21.42*** | |
| Gender (1 = male) | 1.49*** | 1.65*** | 1.66*** | 1.53*** | |
| Education (ref = more than primary) | |||||
| No education | 1.27* | 1.10 | 1.12 | ||
| Primary education | 1.11 | 0.99 | 1.01 | ||
| Is a cadre | 0.42*** | 0.49** | 0.49** | 0.44*** | |
| Occupation (ref = skilled/white collar) | |||||
| Unskilled/agricultural | 1.38** | 1.16 | 1.11 | ||
| Never worked/other/missing | 1.42** | 1.34* | 1.28 | ||
| Wealth quintile (ref = highest) | |||||
| Lowest quintile | 1.11 | 0.95 | 0.88 | ||
| Second quintile | 1.09 | 1.02 | 0.98 | ||
| Third quintile | 1.18 | 1.08 | 1.03 | ||
| Fourth quintile | 1.11 | 1.05 | 1.01 | ||
| Has insurance | 0.83* | 0.92 | 0.88 | ||
| Log average wage | 0.89** | 0.89** | 0.86*** | 0.89** | |
| Number of amenities | 0.94*** | 0.95** | 0.94*** | 0.94*** | |
| Number medical facilities | 1.01 | 1.01 | 1.01 | ||
| Distance to nearest facility (ref = 0–.50 km) | |||||
| .51–2.00 km | 0.99 | 0.97 | 1.00 | ||
| 2.01+ km | 1.10 | 1.06 | 1.07 | ||
| Missing distance information | 0.78* | 0.80 | 0.83 | ||
| Ill health | 2.06*** | 2.15*** | 2.15*** | ||
| LL | −6824.3 | −6808.0 | −6775.6 | −6781.7 | |
| Δ −2LL from base | 32.7*** | 94.4*** | 84.2*** | ||
| θ | 0.111*** | 0.093*** | 0.103*** | 0.112*** |
Notes: i−x = 10 models (i−x), each of which includes base plus one additional covariate; LL = log likelihood.
Results of a shared frailty hazard model with standard errors of hazard ratios conditional on θ. N based on number of measured episodes.
Results represent a series of models that all adjusted for residence, age, and gender. Results for residence, age, gender, LL, and Δ −2LL not shown.
Addition of other covariates did not substantially change the urban coefficient or the Δ −2LL from base.
p < .10
p < .05
p < .01, two-tailed.
The base model showed a hazard ratio for rural of 1.32, meaning that after controlling for age and gender, mortality was 32% higher in rural areas. The results also showed a rapid increase in the hazard with increasing age, with men having a greater risk than women.
Column 2 shows partial results of ten models. Although not shown, effects for age and gender remained significant and consistent throughout. The urban/rural effect never declined to a point of insignificance across these models, and its hazard ratio varied between about 1.3 and 1.2 depending upon the specific covariate being included. Most individual-level variables were significant. Those with no education had a significantly higher hazard of mortality than those with more than primary education. Cadres had a significantly lower risk of mortality. Those with unskilled or agricultural occupations and those categorized as having an “other” occupation were at higher risk for mortality than skilled and white collar workers, and those with insurance were at lower risk. Those with lower than the highest wealth quintile were at higher risk for mortality, therefore the variable was in the expected direction, but the effect did not reach a level of statistical significance. For community-level variables, higher average wage within a community and a greater number of amenities significantly decreased mortality. Distance to nearest facility and number of facilities played no role. Those reporting ill health were substantially more likely to die than were others.
Column 3 shows effects when we considered individual and community characteristics simultaneously. The urban advantage was reduced, with the rural hazard ratio falling to 1.18. Of the individual- and community-level covariates, two of each remained statistically significant. Specifically, being a cadre reduced the hazard of dying, as did having a skilled or white collar occupation versus being in the never worked/other/missing occupation category. At the community level, number of amenities and the average wage in the community remained statistically significant when other things were adjusted. Column 4 adds the health variable to determine whether the impact of urban/rural residence on mortality works primarily through health. We did not find evidence for this. Although being in ill health greatly increased the hazard of dying, the hazard ratio for the rural area was 1.19 and statistically significant. Therefore, even accounting for whether an individual was in poor or good health, we found mortality to be higher in rural areas of China. In fact, Table 2 shows that those in rural areas were less, not more, likely to report ill health. The indirect influence of rural residence on the hazard of dying through ill health was therefore negative.
Column 5 includes the combination of covariates that most efficiently accounted for the urban advantage. Cadre status, average wage within a community, and number of amenities within a community best represented the impact of individual- and community-level factors on mortality. The descriptive results shown above suggested that people in urban areas were more likely to be cadres, and urban communities were more likely to have higher wages and a greater number of amenities than rural communities. In turn, cadres and those living in communities with higher average wages and more amenities were less likely to die than others, a result that accounted for some of the urban advantage. These three covariates alone reduced the hazard of rural residence from 1.32 in the base model to 1.22. We also included the health covariate in the final model, and those in ill health had a much higher hazard of dying than others.
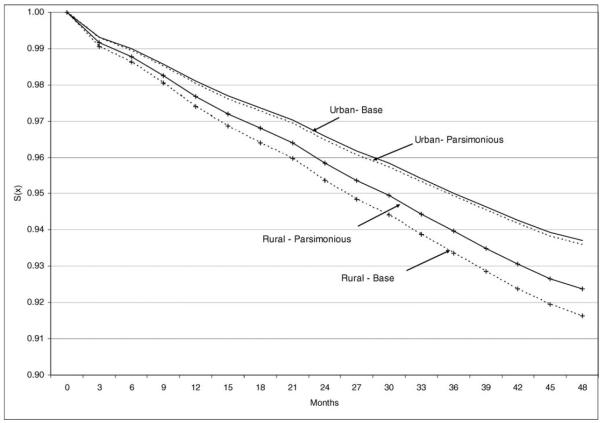
Figure 1 shows visually the net impact of urban versus rural residence on mortality based on this final parsimonious model. The figure represents underlying survival curves for a 65- to 69-year-old woman. We chose this age and gender for heuristic purposes. A person of different age and gender would have a different but proportional survival curve. Although the risk of dying remained fairly similar for urban residents in the base and parsimonious models, the risk of dying for rural residents neared urban residents when considering the parsimonious model. For instance, from the base model we determined that after 12 months an urban woman aged 65 to 69 had a .9803 probability of survival, compared with .9740 for her rural counterpart, an overall difference of .0063. When we held cadre status, average wage, number of amenities, and ill health constant, the probabilities converged to .9810 for the urban woman and .9769 for the rural, decreasing the difference to .0041. So, the base advantage was reduced by about one third. The residual two thirds of the urban advantage remained unexplained.
Figure 1.
Implied survival curves for a 65–69 year old woman by urban and rural residence assuming base and parsimonious models.
Given the strong impact of cadre status, and previous literature showing substantial mortality differences by gender and level of education, we conducted further analyses examining interactions between these covariates and urban/rural residence. We found nothing that was statistically significant. Therefore, living in an urban area had a similar advantage for women as for men and for those who were better educated as for those who were less educated. We did find that being a cadre was more advantageous in urban areas, but the small number of rural cadres in the current sample (only about 2% of rural residents were cadres) resulted in unstable standard errors and a nonsignificant interaction effect. It is therefore difficult to come to a definitive conclusion on this issue.
We explored cadre status further with the notion that resources accrued and services available to a cadre may extend to household members themselves not classified as cadres. As such, an older person may benefit from the cadre membership of a family member. In further analyses we tested variables measuring household cadre status. For instance, we tested a three-category variable coded as 1 = respondent is a cadre, 2 = respondent is not a cadre but someone else in household is, and 3 = no one in household is a cadre. These analyses indicated that the important determinant of mortality was cadre status of the older person, whereas cadre status of other household members, though having a small negative impact, was less important and statistically nonsignificant.
Discussion
Policies have treated urban and rural areas in China differently, and a byproduct of China's rapid development is growing differentiation between urban and rural social and economic life. Whereas urban China witnesses expansions of infrastructure, less investment has been made in rural China and the availability of health services may have declined owing to the dismantling of cooperative services and the introduction of pay-for-service. It is not surprising, then, that data have documented an urban mortality advantage. Still, the numbers of studies are modest, and little research has focused on old-age mortality or the mechanisms driving an urban advantage. Nevertheless, the issue is of critical importance, especially for a country undergoing population aging and a subsequent increase in the proportion at very old ages (Andrews, 2001; Kinsella, 2001; Kinsella & Phillips, 2005; Langmore, 2001; United Nations, 2002b; Zeng & George, 2001). It is reasonable to expect that these age structure changes will alter the provision of health care, making understanding the determinants of health among elders critical for the development and implementation of policy (Mayhew, 1999). The current study examined variation in mortality between urban and rural China among adults aged 50 and older. We found mortality to be about 30% higher in rural areas when controlling for age and gender based on standardized mortality rates and on results of a Cox proportional hazards model. The advantage was fairly consistent when comparing the CHNS and the 2000 Census.
The analysis also examined the extent to which variables representing socioeconomic and health service characteristics of individuals and the communities in which they live explain the urban advantage. Three turned out to be particularly important. On the individual level, it was cadre status. Urban residents were more than 3 times more likely to be cadres, and being a cadre is beneficial for survival. Traditionally, cadres were elite officials holding responsible positions within the party, and cadre status provided them with privileges that the average citizen may not have accrued (Lee, 1991, Y. Li, 2005; Nee, 1996). For instance, they may have had better access to health service, housing, or employment. Some have argued that cadres have recently become a kind of elite civil service, but they nonetheless are well positioned to take advantage of China's economic growth, being able to acquire good positions within the government employment system. As such, cadre status may be a proxy for a host of other socioeconomically related factors not accounted for in the current study and for access to health services. It might also relate to psychological resources influencing health, such as level of stress and feelings of control and self-worth. It is unsurprising that cadres have lower mortality, but it is surprising that cadre status is so important in comparison to education, occupation, and insurance. The result here supports a long-standing finding about the connection between socioeconomic status and mortality (Antonovsky, 1967; Mackenbach et al., 1997; Marmot et al., 1984; Preston & Taubman, 1994), but it suggests that the specific indicator of socioeconomic status that is critical may be culturally dependent.
On the community level, important measures were number of amenities within the community and the average wage for an ordinary male worker. Urban communities have on average a greater number of amenities and a higher wage structure. In turn, individuals living in communities with a large number of amenities and higher average wages have a lower risk of mortality. Average wage has a clear association with community wealth, which may consequently result in the availability of better and more technologically advanced resources for community members. Number of amenities, constructed by summing seven items, is also an indicator of resources available within a community as well as remoteness and level of infrastructure development. As such, amenities may be a proxy for a congregation of other services, including those both wealth and health related. Some amenities, like telephone service, facilitate communication, whereas others, like paved roads, facilitate transportation. Both of these factors may be important for transferring health information to older adults, moving both formal and informal care into the community, and allowing older adults to be in contact with family members. The latter may have psychological benefits and result in more efficient informal assistance.
Given that the amenities measure was a composite of seven individual items, separate analyses not presented here predicted survival given existence versus nonexistence of each amenity, adjusting for age, gender, and residence. Telegraph service, electricity, telephone service, and paved roads are most important, in that order. Post office, movie theaters, and newspapers are least important. There are several possible explanations for this. One is that amenities that are most important facilitate communication and transportation, which are important for the provision and efficient transfer of formal and informal care. A second is that amenities that are most important are more basic and distinguish the poorest and most remote communities. A movie theater or newspapers may arrive in a community only after more basic infrastructure such as telephone service and paved roads, and the earlier types of development are more crucial for health. This suggests a threshold above which communities become more equal. Still, the summed score created from the seven items proves to be the best indicator.
It is surprising that number of medical facilities had virtually no influence. Unlike a measure better related to actual community wealth, number of facilities may not translate well into quality of service or capacity of care. Small facilities may be poorly maintained and equipped and may be staffed with less qualified personnel. At the same time, fewer larger facilities may provide better medical treatment, be technologically more advanced, and be able to handle a larger collection of health problems. Thus, the positive influence of a greater number of facilities might be negated by the superior capability of larger facilities. Questions regarding the impact of number of doctors, nurses, and specialists; quality of available care; number of available beds; quality of facilities; and other similar variables for which we did not have appropriate measures remain.
We should note several issues regarding covariates. First, due to inclusion criteria, like consistent measurement over time, the study employed a limited number of covariates. Still, even with a small number of covariates we were able to account for about at least one third of the urban advantage. Second, there were some fairly high correlations among covariates, such as between having more than a primary education and being a cadre (r = .30), having a skilled occupation and being a cadre (r = .36), and wealth index score and having insurance (r = .30). This “shared variance” might be one factor accounting for rather weak significance among some covariates in a full model. Third, there were some curious results. Having an “other” occupation in comparison to a skilled or white collar occupation functioned to increase risk of mortality. It is difficult to interpret this result because “other” comprised mostly those who had never worked or those not stating an occupation. Also, although a health insurance influence came through when other individual level covariates were not controlled, its insignificance in a full model circumvented common sense.
Also, we are cautious about the accuracy of mortality reporting in China. Prior research has suggested that census and vital registration data in China underestimate number of deaths (Banister & Hill, 2004; Yang et al., 2005). A footnote in the DY declared that death rates were inflated to calculate life expectancies because it was assumed that there was underreporting in vital registration. Still, because death rates in the CHNS mirror, to a degree, those in the CC and DY, we can speculate that whatever inaccuracies exist in the CHNS parallel those in other sources. Moreover, underreporting is thought to be greater in rural areas. If this is true, the results shown here represent an underestimation of the urban advantage in mortality.
In sum, the policy implications of our findings appear to be clear: Investment in rural infrastructure, especially in electricity, telephone and telegraph services, and paved roads, appears to have a beneficial role in reducing health inequalities, and this may be particularly so for the poorest and most remote communities. Investing in rural economy in general to improve wage structure also appears to help reduce urban/rural inequalities in health. Although we were not able to study in detail how cadre status exactly benefits the health of older adults, we speculate it to be at least partly through increased health care access. Thus, our results highlight the significance of improving individual-level access to various resources, thereby reducing inequality in access. Future research should address the mechanisms through which being a cadre is associated with health and mortality among older adults in China. Future studies should also examine the impact of additional community factors on urban/rural differences in health, including more detailed information about the availability of health care services, such as quality of service and capacity of care. It is also essential to monitor changes in levels of urban/rural inequality in health as China undergoes further rapid socioeconomic development.
Acknowledgments
The preparation of this article was supported in part by Grant R03 AG025729 from the National Institutes of Health (National Institute on Aging). We thank three anonymous reviewers for their helpful suggestions on an earlier version of the article. Lead author Zachary Zimmer conceived the study; organized and managed the study team; and led all aspects of the preparation of the article, including planning and implementing statistical methods, data analysis and modeling, interpreting results, writing the initial version of the article, and making revisions based on reviewer and editor comments. Second author Toshiko Kaneda was involved in all aspects of the study including conception, data analysis, writing, and editing. Third author Laura Spess took primary responsibility for management of data and methods, including data manipulation, use of statistical software, and planning and implementation of statistical models.
References
- Andrews GR. Demographic and health issues in rural aging: A global perspective. Journal of Rural Health. 2001;17:323–327. doi: 10.1111/j.1748-0361.2001.tb00281.x. [DOI] [PubMed] [Google Scholar]
- Antonovsky A. Social class, life expectancy and overall mortality. Milbank Memorial Fund Quarterly. 1967;45:31–73. [PubMed] [Google Scholar]
- Banister J, Hill K. Mortality in China 1964–2000. Population Studies. 2004;58:55–75. doi: 10.1080/0032472032000183753. [DOI] [PubMed] [Google Scholar]
- Beach M. China's rural health care gradually worsens. Lancet. 2001;358:567. doi: 10.1016/s0140-6736(01)05754-3. [DOI] [PubMed] [Google Scholar]
- Bell AC, Ge K, Popkin BM. Weight gain and its predictors in Chinese adults. International Journal of Obesity. 2001;25:1079–1086. doi: 10.1038/sj.ijo.0801651. [DOI] [PubMed] [Google Scholar]
- Beydoun MA, Popkin BM. The impact of socio-economic factors on functional status decline among community-dwelling older adults in China. Social Science & Medicine. 2005;60:2045–2057. doi: 10.1016/j.socscimed.2004.08.063. [DOI] [PubMed] [Google Scholar]
- Box-Steffensmeier JM, Jones BS. Event history modeling. Cambridge University Press; New York: 2004. [Google Scholar]
- Bradley JB, Stephens T, Harpham T, Cairncross S. A review of environmental health impacts in developing country cities. World Bank; Washington, DC: 1992. [Google Scholar]
- Chen XM, Hu TW, Lin Z. The rise and decline of the cooperative medical system in rural China. International Journal of Health Services. 1993;23:731–742. doi: 10.2190/F8PB-HGJH-FHA8-6KH9. [DOI] [PubMed] [Google Scholar]
- China Data Center China data online. 2006 Retrieved April 26, 2006, from http://chinadataonline.org.
- Clifford WB, Brannon YS. Rural–urban differences in mortality. Rural Sociology. 1985;50:210–224. [Google Scholar]
- Eastwood R, Lipton M. Rural urban dimensions of inequality change (United Nations University World Institute for Development Economic Research Working Paper No. 200) WIDER Publications; Helsinki, Finland: 2000. [Google Scholar]
- England RS. Aging China: The demographic challenge to China's economic prospects. Praeger; Westport, CT: 2005. [Google Scholar]
- Entwisle B, Chen F. Work patterns following a birth in urban and rural China: A longitudinal study. European Journal of Population. 2002;18:99–119. [Google Scholar]
- Fang RK. The geographical inequalities of mortality in China. Social Science & Medicine. 1993;36:1319–1323. doi: 10.1016/0277-9536(93)90222-p. [DOI] [PubMed] [Google Scholar]
- Filmer D, Pritchett L. Estimating wealth effects without expenditure data—or tears: An application to educational enrollments in states of India. Demography. 2001;38:115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- Goldstein H. Multilevel statistical models. 3rd ed. Oxford University Press; London: 2003. [Google Scholar]
- Harpham T, Tanner M, editors. Urban health in developing countries: Progress and prospects. St. Martin's Press; New York: 1995. [Google Scholar]
- Hayward MD, Pienta AM, Mclaughlin DK. Inequality in men's mortality: The socioeconomic status gradient and geographic context. Journal of Health and Social Behavior. 1997;38:313–330. [PubMed] [Google Scholar]
- Hougaard P. Frailty models for survival data. Lifetime Data Analysis. 1995;1:255–273. doi: 10.1007/BF00985760. [DOI] [PubMed] [Google Scholar]
- House JS, Lepkowski JM, Williams DR, Mero RP, Lantz PM, Robert SA, et al. Excess mortality among urban residents: How much, for whom, and why? American Journal of Public Health. 2000;90:1898–1904. doi: 10.2105/ajph.90.12.1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn J. China's leader urges shift in development to rural areas. New York Times. 2004 March 5;:6. [Google Scholar]
- Kearns G. The urban penalty and the population history of England. In: Brandstrom A, Tedebrand L, editors. Society, health and population during the demographic transition. Almquist & Wiskell International; Stockholm: 1988. pp. 213–236. [Google Scholar]
- Kinsella K. Urban and rural dimensions of global population aging: An overview. Journal of Rural Health. 2001;17:314–322. doi: 10.1111/j.1748-0361.2001.tb00280.x. [DOI] [PubMed] [Google Scholar]
- Kinsella K, Phillips DR. Global aging: The challenge of success. Population Bulletin. 2005;60:1–40. [Google Scholar]
- Kirkby RJR. The definition of urban population in the People's Republic of China. In: Kirby RJR, editor. Urbanization in China: Town and country in a developing economy, 1949–2000 AD. Columbia University Press; New York: 1985. pp. 54–102. [Google Scholar]
- Kitagawa EM, Hauser PM. Differential mortality in the United States: A study of socioeconomic epidemiology. Harvard University Press; Cambridge, MA: 1973. [Google Scholar]
- Landers J. Mortality and metropolis: The case of London 1675–1825. Population Studies. 1987;41:59–76. doi: 10.1080/0032472031000142536. [DOI] [PubMed] [Google Scholar]
- Langmore J. Rural aging: A global challenge. Journal of Rural Health. 2001;17:305–306. doi: 10.1111/j.1748-0361.2001.tb00276.x. [DOI] [PubMed] [Google Scholar]
- Lee HY. From revolutionary cadres to party technocrats in socialist China. University of California Press; Berkeley: 1991. [Google Scholar]
- Li S, Sun F. Mortality analysis of China's 2000 population census data: A preliminary examination. China Review. 2003;3:31–48. [Google Scholar]
- Li Y. The structure and evolution of Chinese social stratification. University Press of America; Lanham, MD: 2005. [Google Scholar]
- Lili M. Analysis of social and economic factors affecting mortality in China. Chinese Journal of Population Science. 1993;5:119–132. [PubMed] [Google Scholar]
- Mackenbach JP, Kunst AE, Cavelaars JM, Groenhof F, Geurts JJM, The EU Working Group on Socioeconomic Inequalities in Health Socioeconomic inequalities in morbidity and mortality in western Europe. Lancet. 1997;349:1655–1659. doi: 10.1016/s0140-6736(96)07226-1. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Shipley M, Rose G. Inequalities in death: Specific explanations of a general pattern? Lancet. 1984;321:1003–1006. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- Mayhew L. Health and welfare services expenditure in an aging world (Interim Rep. No. IR-99-035) International Institute for Applied Systems Analysis; Laxenburg, Austria: 1999. [Google Scholar]
- Meng Q, Liu X, Shi J. Comparing the services and quality of private and public clinics in rural China. Health and Policy Planning. 2000;15:349–356. doi: 10.1093/heapol/15.4.349. [DOI] [PubMed] [Google Scholar]
- National Research Council . Cities transformed: Demographic change and its implications in the developing world. National Academies Press; Washington, DC: 2003. [Google Scholar]
- Nee V. The emergence of a market society: Changing mechanisms of stratification in China. American Journal of Sociology. 1996;101:908–949. [Google Scholar]
- Pickles A, Crouchley R. A comparison of frailty models for multivariate survival data. Statistics in Medicine. 1995;14:1447–1461. doi: 10.1002/sim.4780141305. [DOI] [PubMed] [Google Scholar]
- Preston SH, Taubman P. Socioeconomic differences in adult mortality and health status. In: Martin LG, Preston SH, editors. Demography of aging. National Academy Press; Washington, DC: 1994. pp. 279–318. [PubMed] [Google Scholar]
- Rutstein S, Johnson K. The DHS wealth index. ORC Macro; Calverton, MD: 2004. [Google Scholar]
- Shi L. Access to care in post-economic reform rural China: Results from a 1994 cross-sectional survey. Journal of Public Health Policy. 1996;17:347–361. [PubMed] [Google Scholar]
- Smith MH, Anderson RT, Bradham DD, Longino CF. Urban and rural differences in mortality among Americans 55 years and older: Analysis of the national longitudinal mortality study. Journal of Rural Health. 1995;11:274–285. doi: 10.1111/j.1748-0361.1995.tb00425.x. [DOI] [PubMed] [Google Scholar]
- Stephens C. Healthy cities or unhealthy islands? The health and social implications of urban inequality. Environment and Urbanization. 1996;8:9–30. [Google Scholar]
- United Nations . Demographic yearbook 2000. Author; New York: 2002a. [Google Scholar]
- United Nations . World population ageing 1950–2050. Author; New York: 2002b. [Google Scholar]
- Wang Y, Bentley ME, Zhai F, Popkin BM. Tracking of dietary intake patterns of Chinese from childhood to adolescence over a six-year follow-up period. Journal of Nutrition. 2002;132:430–438. doi: 10.1093/jn/132.3.430. [DOI] [PubMed] [Google Scholar]
- Woods R. Urban–rural mortality differentials: An unresolved debate. Population and Development Review. 2003;29:29–46. [Google Scholar]
- Yang G, Hu J, Rao KQ, Ma J, Rao C, Lopez AD. Mortality registration and surveillance in China: History, current situation and challenges. Population Health Metrics. 2005;3:1–9. doi: 10.1186/1478-7954-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Y. An analysis of changing trends in China's urban and rural households. Chinese Journal of Population Science. 1990;2:187–199. [PubMed] [Google Scholar]
- Zeng Y, George LK. Extremely rapid ageing and the living arrangements of the elderly: The case of China. Population Bulletin of the United Nations. 2001;42/43:255–287. [Google Scholar]
- Zhai S, McGarvey ST. Temporal changes and rural–urban differences in cardiovascular disease risk factors and mortality in China. Human Biology. 1992;64:807–819. [PubMed] [Google Scholar]