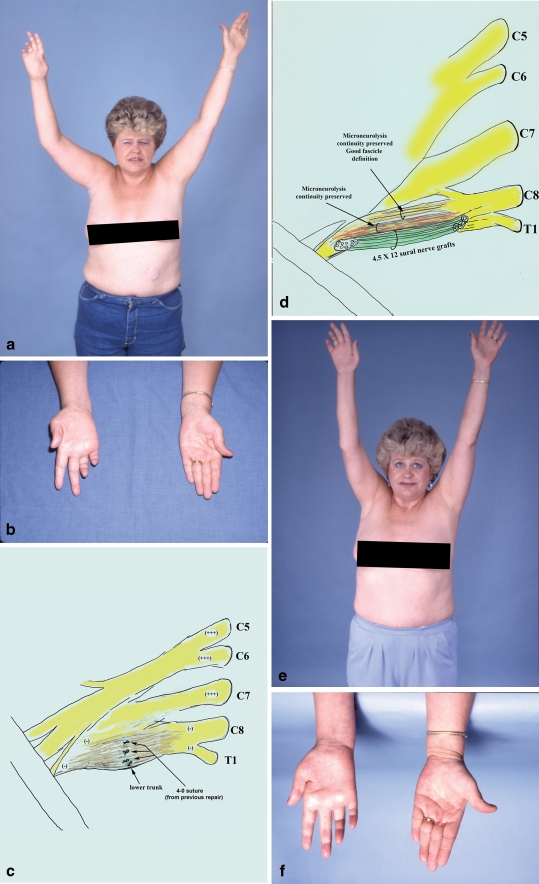
Figure 4.
A 41-year-old female sustained iatrogenic injury to the right brachial plexus during transaxillary first rib resection, elsewhere (patient no. 9 in Table 7). Although there was an attempt to repair the injured lower trunk intraoperatively with 4-0 sutures, there were no signs of nerve regeneration. She developed reflex sympathetic dystrophy which required sympathectomy resulting in mild improvement. This patient was referred to our center and presented 14 months after the initial surgery, with severe burning pain in the ulnar side of the hand and the medial surface of the upper third of the arm, as well as near complete ulnar nerve palsy (a, b). Exploration of the right supraclavicular plexus revealed a large neuroma in the lower trunk. Suture remnants were observed among the scar tissue (c). The lower trunk of the brachial plexus was reconstructed with a combination of partial nerve grafting and extensive microneurolysis (d). Fascicles with perineurial integrity were preserved while those that were replaced by scar were resected, and the gap repaired with 12 sural nerve grafts, each 4.5 cm in length. This patient also had crushing of the intercostobrachial nerves during the transaxillary first rib resection. This lesion required microneurolysis, resection of the neuroma, and nerve repair. At the last office visit (18 months after surgery), she was pain-free over the ulnar nerve distribution, and also over her medial arm, and quite happy with the result (e). However, minimal motor improvement in ulnar innervated targets was observed; she was graded as a fair result (f).