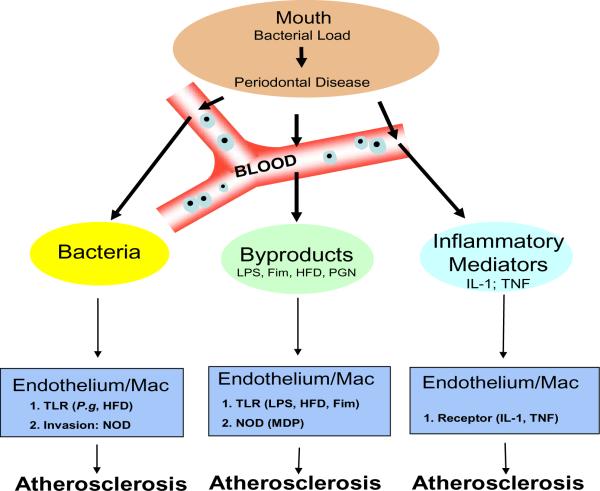
Fig. 2.
Relationship of P.gingivalis Infection and Atherosclerosis
As the bacterial load of P.gingivalis in the oral cavity increases periodontal disease becomes more severe. However, damage is not just limited to the oral cavity since local vasculature enables an entry point for bacteria, bacterial by-products, or inflammatory mediators (e.g cytokines interleukin-1 or tumor necrosis factor-α). Bacteremias, common in periodontal disease due to dental work e.g. cleaning, flossing or surgery, effect both endothelium and macrophages by inducing homotolarance along the Toll-like receptor (TLR) pathway. However, since P.gingivalis is an invasive bacterium, mediated by its fimbriae (Fim) protein, it has the ability to activate the cytosolic nucleotide oligomerization domains (NODs) through recognition of muramyl dipeptide (MDP), a fragment of peptidoglycan (PGN). In addition, various bacterial by-products, e.g. Lipopolysaccharide (LPS), can also activate both the endothelium and macrophages. Further, from the oral cavity a state of local inflammation exists and immune cells are constantly releasing inflammatory mediators into the circulation, these mediators, interleukin-1 or tumor necrosis factor-α, can activate both the endothelium and macrophages. Finally, activated endothelium and macrophages have been shown to exacerbate Atherosclerosis when coupled with a high fat diet (HFD).