Abstract
Purpose
The purpose of the study was to understand US dentists’ attitudes, knowledge, and practices regarding dental care for pregnant women and to determine the impact of recent papers on oral health and pregnancy and guidelines disseminated widely.
Methods
In 2006–2007, the investigators conducted a mailed survey of all 1,604 general dentists in Oregon; 55.2% responded). Structural equation modeling was used to estimate associations between dentists’ attitudes toward providing care to pregnant women, dentists’ knowledge about the safety of dental procedures, and dentists’ current practice patterns.
Results
Dentist’s perceived barriers have the strongest direct effect on current practice and might be the most important factor deterring dentists from providing care to pregnant patients. Five attitudes (perceived barriers) were associated with providing less dental services: time, economic, skills, dental staff resistance, and peer pressure. The final model shows a good fit with a chi-square of 38.286 (p = .12, n=772, df = 52) and a Bentler-Bonett Normed Fit index of .98, CFI = .993. The Root Mean Square Error of Approximation is .02.
Conclusions
Findings suggest attitudes are significant determinants of accurate knowledge and current practice. Multi-dimensional approaches are needed to increase access to dental care and protect the oral health of women during pregnancy. Despite current clinical recommendations to deliver all necessary care to pregnant patients during 1st, 2nd, and 3rd trimesters, dentists’ knowledge of the appropriateness of procedures continues to lag the state of the art in dental science.
Introduction and Background
Poor maternal oral health can increase the risk of complications of pregnancy including preterm delivery or low birth weight, gestational diabetes, preeclampsia, small for gestational age infants, and stillbirth (Vergnes & Sixou, 2007). Moreover, fetal exposure to oral pathogens may increase risk of subsequent neonatal intensive care admission (Jared et al., 2009). However, the periods before and after pregnancies are also important (D’Angelo et al., 2007). Health care goals during the interconception period are to improve the knowledge, attitudes, and behaviors of women regarding their preconception health, ensure all women of childbearing age receive preconception care services, reduce risks to future pregnancies indicated by adverse events experienced in prior pregnancies, and reduce disparities in adverse pregnancy outcomes (D’Angelo et al., 2007).
The recognition of the importance of oral health for the health of the women and future children has led professional associations and governmental agencies to issue practice recommendations, policy briefs, and fact sheets to raise public and professional awareness of the oral health needs of pregnant women and improve oral health care provided during pregnancy and early childhood (American Dental Association, 2000; Centers for Disease Control and Prevention, 2001; American Academy of Pediatric Dentistry, 2008). In 2006, an expert panel was convened by the New York State Health Department to create practice guidelines for prenatal, oral health, and child health professionals regarding oral health care during pregnancy and early childhood. Publication of the Practice Guidelines (New York Department of Health, 2006), in August 2006, was supported by grants from the Federal Maternal and Child Health Bureau, the Centers for Disease Control, and the Health Resources Administration. Professional organizations and government have undertaken efforts to disseminate and reinforce these recommendations and dentists throughout the country should have learned and adopted the recommendations. It is not known if the guidelines have had the intended effect.
Dental Utilization Is Low For All Women
The utilization of dental care during pregnancy is reported to be low (Le et al., 2009; Lydon-Rochelle et al., 2004). Data from an ongoing population-based survey conducted by the CDC (the Pregnancy Risk Assessment Monitoring System: PRAMS) indicate the proportion of women who receive dental services during pregnancy varies among the U.S. states, and ranges from 23 to 43% (Gaffield et al., 2001; Jeffcoat et al., 2001; Magskau & Arrindell, 1996). In one study, among women who reported having oral health problems, only one-half said they sought dental care (Ressler-Maerlender, Krishna, & Robison, 2005). Some women said that poor oral health status during pregnancy is normal, and some believed dental treatment was harmful to their unborn child.
Insurance Coverage for Dental Services is Not Sufficient to Reduce Barriers to Care
Access to dental care is severely limited for low-income pregnant women (even those with Medicaid insurance) and limited at all times for other women with limited social, political, and cultural resources. Pregnancy represents a time of increased risk of dental pathology and need for good care. According to a population-based study conducted in North Dakota, young women, particularly teenage mothers, women in poverty, and women with Medicaid coverage were at increased risk of not having a dental visit during pregnancy (Magskau & Arrindell, 1996). A longitudinal study of the oral health of diverse groups of patients in Florida found that African Americans, rural residents, individuals with less than a high school education, and those with limited financial resources had significantly higher occurrences of oral disadvantage (Chavers, Gilbert, & Shelton, 2002)
A study of the utilization patterns of women in Oregon eligible for Medicaid coverage for dental services during pregnancy and the child bearing years found few women received services (Lee et al., 2010). It is likely that utilization rates were affected by changes in the state’s eligibility requirements. The rate of dental care among pregnant women dropped from 17–21% in 2000–2002 to 10% in 2005; among women with young children rates declined from 27– 29% in 2000–2002 to 11–14% in 2005 (Milgrom, Lee, Huebner, & Conrad, 2010). This trend is alarming given the CDC’s recommendation that every state provide dental services to all women during pregnancy and the interconception period. Currently only 33 of 50 states and the District of Columbia provide dental benefits to pregnant women enrolled in Medicaid. Fewer states provide dental coverage during the interconception period and those that do severely restrict what is allowed (American Dental Association, 2009).
The Problem Is Multi-Dimensional
For low-income women eligible for Medicaid, pregnancy and post-partum can be the only periods when they have access to dental care. It is essential that low-income women and women with oral health problems prior or during pregnancy seek dental care. Dental care is safe during pregnancy; the optimal period for care is during the second trimester and emergency services can be provided at any time. Barriers to receipt of dental services during pregnancy include lack of knowledge or misinformation about the safety and importance of dental care for the health of the mother and the fetus. Limited oral health literacy is not unique to women with lower levels of education. Many women are not aware that severe periodontal infection can endanger the unborn child. Many will not seek restorative or preventive care because they believe dental procedures can harm the fetus (Gaffield, et al., 2001; Gilbert, et al., 1999) and many new mothers are unaware of the transmissible nature of dental caries.
Dental care providers also create barriers to care. A survey of general dentists in Oregon conducted by Huebner and colleagues (Huebner et al., 2009) found 71%of dentists reported low compensation by insurance plans was a barrier to providing counseling to pregnant patients; 11% said they were “too busy” to add counseling about oral health care for pregnant patients to their practices. A study of obstetrician gynecologists found 77% reported their pregnant women were “declined” treatment by dentists (Morgan, et al., 2009). Another survey, of both dental and medical providers, found most rated prenatal dental screening as important, but many thought x-rays, periodontal surgery, amalgam fillings, and pain medication were dangerous to pregnant women (Strafford, Shellhaas, & Hade, 2008). This same survey found that obstetricians were more comfortable than the dentists with recommended dental procedures and needed medication for pregnant women, but were less likely to recommend dental care to their patients.
The purpose of this paper is to describe the scope of dental care provided to pregnant women. Specifically, we sought to learn how closely the knowledge and practices of general dentists reflected the recent Practice Guidelines (New York Department of Health, 2006). We utilized a structural equation model to test the effects of dentists’ knowledge and attitudes about dental care for pregnant patients on self-reported clinical practices.
Methods
Participants
The sampling frame included all general dentists in the State of Oregon in 2005. Contact information was taken from the Masterfile of the American Dental Association, which includes all licensed dentists: 1,604 general practitioners were listed for 2005; 729 (55.2%) participated in the survey. The study was conducted in 2006–2007.
Source of Data and Survey Procedure
The study method was a mailed survey of dentist’s attitudes, practices, and knowledge regarding provision of dental care to pregnant women. We employed the Tailored Design Method (Dillman, 2000) because it achieves high response rates to surveys of health professionals. Each dentist was sent 4 mailings. The first contained an introductory letter explaining the importance and purposes of the study. The second mailing included a cover letter, the questionnaire, and described the option to complete the survey via the Internet. The third and fourth mailings were postcard reminders along with a replacement copy of questionnaire.
The Institutional Review Boards of the University of Washington and Washington State University (WSU) approved the study and the elements of informed consent were included in the cover letter. The survey was conducted by the Economic and Social Sciences Research Center at WSU. Responses were confidential.
Survey Instrument
The survey included 54 multi-level questions about dentists’ attitudes, knowledge regarding the appropriateness of performing routine procedures, and prescription of pharmaceuticals to pregnant women. Respondents were asked their attitudes regarding dental insurance benefits, efficacy of counseling and treating pregnant patients, possible barriers and pressures on the dentist and dental professionals, and their knowledge of the appropriate time period to perform dental procedures or prescribe drugs for pregnant patients. Survey items were written with Likert-scales response formats ranging from 1 to 4 or 5 and anchored with “strongly agree” to “strongly disagree,” or “often” to “never.” Some questions were reversed to avoid response bias. Questions that asked for specific numbers, e.g., the number of hours worked, or patients seen per week, were presented as open-ended questions.
Measures and Scale Development
Number of Pregnant Patients Seen per Week
Each dentist was asked to estimate the number of pregnant patients seen per week in his/her primary practice in a “typical month.”
Dentists’ Attitudes
Perceived barriers (Table 1) were assessed by 12 questions in which dentists were asked to rate the extent to which they agreed or disagreed (1 = strongly agree, 5 = strongly disagree) that the statement was true for them. Using the responses to the 12 items, we performed exploratory factor analysis with varimax rotation to maximize the variance of the loadings within factors and to allow for ease of interpretation. Five factors with eigenvalues greater than 1 were extracted. Item responses were then summed to create 5 scales representing: time costs, economic costs, skill (training) costs, staff resistance, and peer pressure from physicians to provide care to pregnant women. An example of an item representing time costs is “My practice is too busy to add counseling about oral care for pregnant women.” An example of an item representing economic costs is “Insurance plans compensate me adequately for time spent on counseling pregnant patients..” An example of a skill (training) cost item is “Physicians are better able than dentists to counsel pregnant patients about oral health.” An example of an item from the staff resistance scale is “My staff is resistant to me treating pregnant patients.” An example of an item from the peer pressure scale is “Physicians in the community will be critical of me if I provide comprehensive oral health care to pregnant patients.” Cronbach alphas for the scales ranged from .75 to .82.
Table 1.
Descriptive Statistics of Indices of Dentists’ Attitudes (Perceived Barriers) Regarding Provision of Dental Care to Pregnant Patients
| Perceived Barriers | Mean | S.D. | Maximum | Minimum | N |
|---|---|---|---|---|---|
| Time Cost | 8.22 | 1.67 | 2 | 10 | 772 |
| Economic Cost | 8.42 | 2.30 | 3 | 10 | 772 |
| Skill Cost | 5.51 | 1.92 | 3 | 12 | 772 |
| Staff Resistance | 4.38 | 1.92 | 2 | 10 | 772 |
| Peer Pressure | 4.21 | 1.70 | 2 | 10 | 772 |
Incorrect Knowledge of Routine Dental Procedures
Dentists’ knowledge of routine dental procedures was assessed by asking them to review a list of 10 routine procedures and indicate if they believed it was appropriate to provide each to a pregnant patient in the 1st, 2nd, or 3rd trimester of pregnancy, provide it in an emergency, or never provide it. We used the recommendations set forth in the Practice Guidelines (New York Department of Health, 2006) as the correct responses; the Guidelines state all 10 dental procedures can be performed any time during pregnancy to ensure patients receive all necessary dental care. Each routine procedure to which a dentist answered “no” to 1st, 2nd, 3rd trimester was coded as an incorrect response (a score = 1); a correct response received a score of 0. Responses indicating the dentist would not perform the procedures in the event of an emergency were coded similarly (1 = incorrect, 0 = correct). Table 2 shows the distribution of the responses. Exploratory factor analysis, with varimax rotation, was performed on the responses to these items. Two factors with eigenvalues greater than 1 were extracted. Individual’s responses to the items were summed to create 2 scales: incorrect knowledge of providing routine dental procedures and incorrect knowledge regarding performing procedures in a dental emergency (Cronbach alphas = .89 and .95 respectively).
Table 2.
Frequency Distribution of Variables for Indices of Incorrect Knowledge of Routine Procedures, and Emergency Procedures
| Incorrect Knowledge of Routine Procedures | 1st Trimester | 2nd Trimester | 3rd Trimester | Emergency |
|---|---|---|---|---|
| Scaling and Root Planing | 440(57%) | 165(22%) | 354(46%) | 534(69.2%) |
| Single Periapical X-Ray | 596(77.2%) | 426(55.2%) | 440(57%) | 180(23.3%) |
| Full Mouth Survey | 675(87.4%) | 586(75.9%) | 603(78.1%) | 605(78.4%) |
| Injection of Local Anesthetic | 490(63.5%) | 194(25.1%) | 308(39.9%) | 299(38.7%) |
| Single Tooth Extraction | 602(78%) | 373(48.3%) | 469(60.8%) | 166(21.5%) |
| Root Canal Therapy | 584(75.6%) | 329(42.6%) | 441(57.1%) | 196(25.4%) |
| Composite Restoration | 510(66.1%) | 196(25.4%) | 332(43%) | 394(51%) |
| Fixed Bridge | 619(80.2%) | 394(51%) | 513(66.5%) | 543(70.3%) |
| Site Specific Antibiotic | 688(89.1%) | 557(72.2%) | 599(77.6%) | 548(71%) |
| Nitrous Oxide & Oxygen Sedation | 765(99.1%) | 741(96%) | 741(96%) | 684(88.6%) |
Current Practice
Current practices were assessed by asking how often the dentist performed each of 5 dental procedures or used any of 3 medications in treating pregnant women (Table 3). The survey question read: “How often do you perform each of the following procedures on pregnant patients CURRENTLY?” Each response that was consistent with the Practice Guideline was given a score of 1; inconsistent responses were judged to be incorrect and received a score of 0. We performed exploratory factor analysis, with varimax rotation, on the responses to these items. Four factors with eigenvalues greater than 1 were extracted and the results were used to construct four scales: invasive procedures, periodontal procedures, x-rays, and medications (including local anesthetic, site specific antibiotics, and nitrous oxide-oxygen sedation) with Cronbach alphas ranging from .75 to .86.
Table 3.
Frequency of item variables for indices of current practice of invasive procedures, periodontal procedures, x rays, and drug prescriptions, based on dentists’ responses to survey question “How often do you perform each of the following procedures on pregnant women currently?”
| Current Practice Procedures and Drug Prescriptions | |||||
|---|---|---|---|---|---|
| Variables | |||||
| Index of Current Practices of Invasive Procedures | Often | Sometimes | Rarely | Never | Total |
| Single Tooth Extraction | 75(13.3%) | 243(43.1%) | 179(31.7%) | 67(11.95%) | 564(100%) |
| Root Canal Therapy | 91(16.1%) | 244(43.3%) | 183(32.4%) | 46(8.2%) | 564(100%) |
| Composite Restoration | 32(5.7%) | 130(23%) | 277(49.1%) | 125(22.2%) | 564(100%) |
| Index of Current Practices of Periodontal Procedures | Often | Sometimes | Rarely | Never | Total |
| Scaling and Root Planning | 55(9.8%) | 176(31.2%) | 181(32.1%) | 152(27%) | 564(100%) |
| Index of Current Practices of X-Rays | |||||
| Full mouth survey | 357(63.3%) | 94(16.7%) | 59(10.5%) | 54(9.6%) | 564(100%) |
| Index of Current Practices of Drug prescriptions | Often | Sometimes | Rarely | Never | Total |
| Injection of Local Anesthetic | 12(2.1%) | 138(24.5%) | 280(49.6%) | 134(23.8%) | 564(100%) |
| Site Specific Antibiotic | 395(70%) | 113(20%) | 51(9%) | 5(0.9%) | 564(100%) |
| Nitrous Oxide & Oxygen Sedation | 520(92.2%) | 31(5.5%) | 10(1.8%) | 3(0.5%) | 564(100%) |
Data Analysis
Analyses were conducted using SPSS, Version 17, SPSS Inc.; R, Cran.r-project.org; and EQS, Version 6.0, Multivariate Software Inc. We utilized exploratory factor analysis to determine the number of factors and the loadings of variables for each factor. We performed confirmatory factor analysis to assess the hypothesized relationships between the observed indicators and the latent theoretical constructs, and structural equation analysis to confirm the relationships hypothesized in the theoretical model.
Missing cases in our data were estimated with R using regression prediction with non–missing case level information (Bollen, 1989). To control for a downward bias in the estimated standard error, we used bootstrapping techniques to generate standard error estimates.
The structural equation model is expressed as follow:
where η represents the vector of latent endogenous random variables (incorrect knowledge), ξ represents the latent exogenous variables (number of pregnant patients, dentists’ perceived barriers), β is the matrix showing the influence of the latent endogenous variables on each other, and Γ is the coefficient matrix for the effects of ξ on η. ζ is the disturbance vector that is assumed to have an expected value of 0 [E(ζ = 0)]and which is uncorrelated with ξ.
Following the modeling, we conducted confirmatory factor analysis, using EQS 6.0 to test the model. An a priori measurement model specified the underlying relationships across the latent constructs and their observed indicators (Gerbing & Anderson, 1993). Four latent constructs were postulated: dentists’ perceived barriers, pregnant patients seen per week, incorrect knowledge, and current practices. The specification includes the number of latent constructs, the number of indicators for each construct, and whether measurement errors were allowed to correlate. Confirmatory factor analysis was used to test the fit of the observed indicators and the hypothesized latent constructs. In the construction of all latent variables, we used confirmatory factor analysis from the onset because the latent constructs made clear if the observed indicators reflect the underlying latent constructs well. Next, we utilized traditional methods of structural model estimation and evaluation via chi square tests of the null hypotheses that the observed latent and the expected matrices are identical. According to this approach, the theoretical model is accepted if the test fails to reject the null hypothesis (McDonald & Ho, 2002). In addition, we used goodness-of-fit indices to assess the fit of the model to the data: the Bentler Bonett Index or Normed Fit Index (NFI), the Comparative Fit Index (CFI), and root mean square error of approximation (RMSEA) combined with χ2 statistic. A model is considered a good fit with a NFI of .90 or greater, a CFI of .90 or greater, and the RMSEA of less than .05.
Results
Descriptive Findings
The dentists reported seeing between 2 and 3 pregnant patients per week, on average (M = 2.55, SD = 1.09); the median was 4 pregnant patients per week. Table 1 presents the mean and standard deviation of each constructed scale of perceived barriers regarding provision of care. Higher scores on the barriers indicate stronger perceived resistance in terms of counseling, compensation, pressure from office staff, and pressure from peers in medicine. The highest level of perceived barriers toward provision of care to pregnant women was for economic cost: 72.9% of dentists indicated that compensation by insurance companies was inadequate for time spent counseling pregnant patients.
Answers to questions about the appropriateness of performing routine services on pregnant patients during each trimester and in dental emergencies (e.g. toothaches) were compared with recommendations of the CDC and New York State Guidelines that encourage dentists to provide dental and periodontal treatment during pregnancy, including needed radiographs. Our results showed that dentists in Oregon have a high level of incorrect knowledge about routine and emergency procedures (Table 2). For restorative services, less than one-third of the dentists (66%, 25.4%, and 43% respectively) indicated they would not perform composite restorations (tooth colored fillings) during the 1st, 2nd, or 3rd trimesters. Approximately 51% indicated they would not perform composite restorations during a dental emergency. For scaling and root planing (non surgical periodontal treatment for unhealthy gums), 57%, 22%, and 46% indicated they would not provide this service during the 3 trimesters of pregnancy, and 69.2% would not provide this service during an emergency (such as a periodontal or gum abscess involving suppuration, intraoral swelling and fever). Overall, the mean of the indices of incorrect knowledge for routine services during the pregnancy was 44.2 (SD = 6.1, range = 30–54) where higher scores indicate greater incorrect knowledge. For emergencies, the mean was 17.3 (SD = 2.7, range = 11–22), where higher scores again indicate more incorrect knowledge. More than half of the dentists indicated they were reluctant to perform routine services sometime during the pregnancy and three-quarters of them were reluctant to perform services to relieve pain or swelling associated with a dental emergency.
We asked dentists how often they currently performed these procedures for pregnant women (Table 3). For the index of invasive procedures, 56.4% of dentists indicated they sometimes/often performed single tooth extraction on pregnant patients; 28.7% sometimes/often provided composite fillings. For the index of periodontal procedures, 41% sometimes/often performed scaling and root planing (non surgical periodontal services) for pregnant women. Only 26.6% of dentists indicated they often or sometimes provided injectable local anesthetics (pain control for dental procedures). Overall, the mean score for each scale was: invasive procedure (mean = 4.60, SD = .079, possible range = 0–9); periodontal procedures (mean = 1.8, SD = .035, possible range = 0–3); radiographs or x-rays (mean = .67, SD = .037, possible range = 0–3), and local anesthetics, site-specific antibiotics, and nitrous oxide (mean = 2.45, SD = .048, possible range = 0–9).
Our results suggest that although half of the dentists hold incorrect knowledge, the majority say they currently provide invasive and periodontal treatments, and administer or prescribe drugs to their pregnant patients. Current practice is a function of the number of pregnant patients currently being seen. Only 5.7% estimated they saw no pregnant patients in a typical month: 50% said they see 1–2 pregnant patients per month.
Findings of the Model Testing
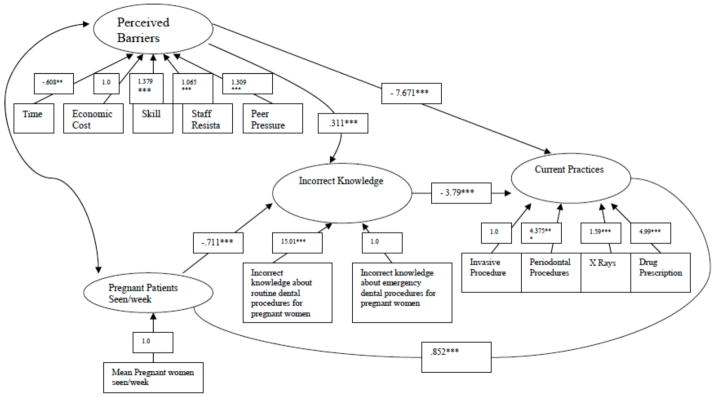
We tested the structural equation model presented in Figure 1. The structural equation model included the following 2 exogenous variables: (1) number of pregnant patients, (2) dentists’ perceived barriers, and 2 endogenous variables: incorrect knowledge and current practices. The final model had an acceptable χ2 =38.29 (df = 119, p = .11). The Bentler-Bonett fit index (NFI) was .984, the Comparative fit index (CFI) was .993, and the Root Mean Square Error of Approximation (RMSEA) was .02. In a further analysis we tested the same model with a random draw of the data, and the fit of the model was similarly acceptable with a χ2 = 45.71 (df = 120, p = .07).
Figure 1.
Relationship between dentists’ attitudes (perceived barriers), average number of pregnant patients seen per week, incorrect knowledge about routine and emergency procedures, and current practices on pregnant patients. All lamba, gama, and beta coefficients in this diagram are in unstandardized format.
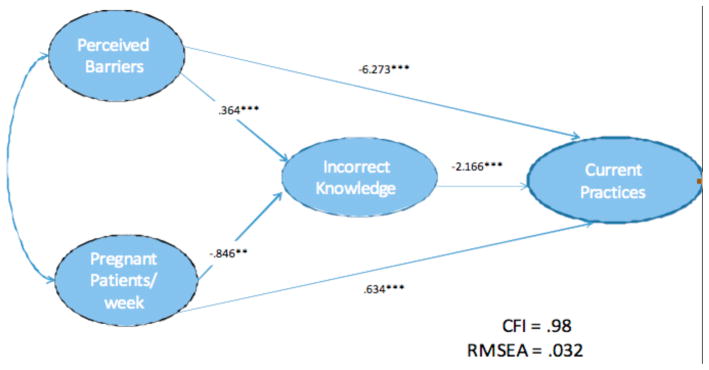
The model was tested to assess how well the observed indictors measured the latent concepts of the proposed conceptual model. The fit was acceptable (χ2 = 70.32, df = 127, p = .08). The Bentler-Bonett fit index (NFI) was .953; the Comparative fit index (CFI) was .978, and the Root Mean Square Error of Approximation (RMSEA) was .032. We included age of the dentist and dentist’s gender as control variables in earlier models; their effects were not significant so they were not included in the final model.
The standardized (β) and the unstandardized regression weights from the structural equation model are shown in Table 5. The dentist’s perceived barriers scale was negatively related to current practices (β = −.6.273, t > 1.96), and to a lesser extent indirectly related to current practices through incorrect knowledge (β = 1.18, t > 1.96). Dentists’ perceived barriers had the strongest direct effect on current practices suggesting they might be the most important factor deterring dentists from providing care to pregnant patients. Dentists’ incorrect knowledge had the second most pronounced effect on current practices (β = −3.79, t > 1.96). Dentists with incorrect knowledge about the appropriateness of routine services and emergency procedures for pregnant patients were less likely to practice currently on pregnant patients. Dentists’ perceived barriers were positively and directly related to incorrect knowledge, (β = .311, t > 1.96), which suggests dentists who perceived high levels of barriers are more likely to have incorrect knowledge of the appropriateness of routine an emergency procedures during pregnancy. The number of pregnant patients reported seen per week was positively related to reported practices that reflect the state of the art in clinical knowledge (β = .852, t > 1.96), and negatively related to incorrect practices (β = −.711, t > 1.96).
Conclusions and Discussion
Our paper investigates how far dental professionals have come in adopting perinatal care practices that follow recommendations of the NY State Department of Health’s expert panel and the CDC. Attitudes are important and barriers clearly remain. Dentists indicated that high levels of perceived time and economic costs, and dissatisfaction with compensation by insurers, were significant barriers to provision of care for pregnant patients. Results from our analysis confirm that dentists’ attitudes have significant negative impacts on current practice.
The result of our analysis should be interpreted in light of several alternative theoretical models. While the model proposed in this paper examined dentists’ perceived barriers and number of pregnant patients as exogenous variables, it is possible that alternative models exist among the exogenous and endogenous variables in the proposed conceptual framework. For example, dentists with incorrect knowledge may perceive more barriers, and thus avoid caring for pregnant patients. Alternatively, dentists who care for a large number of pregnant patients and have low levels of incorrect knowledge might still perceive substantial barriers to caring for this patient population. We tested both of these alternative models, and the results in the final model were more consistent with our hypotheses.
The delivery of perinatal health for the 62 million pregnant women in the US requires a multi-strategy, action-oriented initiative that includes all healthcare professionals, dental and obstetrics professionals and takes advantage of every encounter with women to provide preconception counseling and services to alleviate possible health risks. Previous efforts to disseminate new clinical guidelines through natural diffusion have been slowed by the fragmentation of the current healthcare system. Until critical barriers including insufficient compensation from private or public insurance, compromised access to healthcare, and limited awareness among women in childbearing ages are alleviated, impediments to improving the health of women and children will continue. Women’s health significantly influences the future of children’s health. Only when women’s health issues are given a higher priority by public policy leaders, health care providers, and public and private insurers will there be substantial improvement in the oral and general health of the next generation.
The US is failing to achieve goals set in Healthy People 2010 for oral health. Interventions to address the goals will not be successful if they are not based on a thorough understanding of the complexity of problems. This study draws on previous work in health care to encourage providers to change practices or adopt new ones (Grol & Grimshaw, 2003; Grol & Wensing, 2004). Research in both dentistry and medicine indicates that multi-level interventions, which explicitly address the complex factors that govern care, are more effective than simple ones. In the Access to Baby and Child Dentistry (ABCD) program in Washington State, (Grembowski & Milgrom, 2000), the intervention included key leaders in the local dental community who endorsed dentists’ participation, involvement of paraprofessional staff members, changing dental professionals’ attitudes about Medicaid procedures and about Medicaid clients, reduction of barriers to participate (e.g. reducing problems with billing Medicaid; reducing no shows by low-income clients; higher fees for appropriate procedures); and courses for dentists to increase their knowledge of child management and care procedures. In the ABCD model, workers in local health departments served as parent advocates and counselors and provided case management. This multi-layered approach and community-specific approach increased access to care and dental visits dramatically (Grembowski & Milgrom, 2000). It also changed the focus of care for young children from an episodic and symptom-oriented approach to one of disease prevention. . As a result of initial success, the program has grown (Kobayashi, et al., 2005).
The results of the present study suggest that something similar to the ABCD program is needed to overcome the limitations in the current system so pregnant women and women in the perinatal and interconception periods receive better dental care. However, the knowledge needed to build such an intervention is incomplete. For instance, different types of interventions may be needed to fit the different office contexts (e.g. private versus not for profit offices) and patient populations (e.g. Medicaid/racial/ethnic mix with cultural differences). An example of how such information can be used to tailor an intervention successfully is a pilot program that increased dental care utilization of women in Klamath County, Oregon (Milgrom, et al., 2008). In this program, a county community health coalition identified oral health as a priority and worked with managed care organizations in dentistry and medicine to prioritize care for pregnant women and their young children. A dental hygienist counselor/case manager was hired to work with pregnant women, and the dental offices, to assure the women had timely access to dental care. The women were identified through the Women, Infant and Child (WIC) program in the local health department. The local dental hygiene training program served as an entry point for care. Physicians also made referrals for dental care. As a result, the proportion of pregnant women in the county who saw a dentist during pregnancy increased from 8.8 (before the program period) to nearly 56 percent. A challenge for practice and policy is to encourage field experiments to identify promising practices and then support their “scale up” to improve population health.
Figure 2.
Relationship between dentists’ attitudes (perceived barriers), average number of pregnant patients seen per week, incorrect knowledge about routine and emergency procedures, and current practices on pregnant patients. All lamba, gama, and beta coefficients in this diagram are in standardized format.
Table 4.
Standardized and Unstandardized Regression Coefficients for the Final Model
| Standardized Coefficients | Unstandardized Coefficients | SE | CR | |
|---|---|---|---|---|
| Barriers ➝ Incorrect Knowledge | .364*** | .311 | .018 | 17.28 |
| Barriers ➝ Current Practices | − 6. 273*** | − 7.671 | .47 | 14.19 |
| Pregnant Patients ➝ Incorrect Knowledge | − .846** | −.711 | .12 | 5.83 |
| Pregnant Patients ➝ Current Practices | .634*** | .852 | .098 | 8.69 |
| Incorrect Knowledge ➝ Current Practices | −2.166*** | − 3.79 | .58 | 6.53 |
Note: CR = Critical Ratio;
p < .05;
p < .01;
p < .001.
Critical Ratio is the estimate divided by its standard error. Our estimations are based on random sample variables with standard normal distributions, estimates with critical ratios more than 1.96 are significant at the .05 level.
Acknowledgments
This research was supported by Grant No. R40MC03622 from the Maternal and Child Health Bureau, HRSA, and Grant No. No. U54DE019346 from the National Institute of Dental and Craniofacial Research, NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Rosanna Shuk-Yin Lee, Email: rsyl@u.washington.edu.
Peter Milgrom, Email: dfrc@u.washington.edu.
Colleen E. Huebner, Email: colleenh@u.washington.edu.
Douglas A. Conrad, Email: dconrad@u.washington.edu.
References
- American Academy of Pediatric Dentistry. [Accessed July 11, 2008];Clinical guideline: oral health care for the pregnant adolescent. 2008 Available from http://www.aapd.org/media/policies.asp.
- American Dental Association. ADA Position Statement on Early Childhood Caries, 2000. 2000 Retrieved July 11, 2008 from http://www.ada.org/prof/resources/positions/statements/caries.asp.
- American Dental Association. [Accessed September 11, 2009];State innovations to improve access to oral health: A compendium update[Internet] 2009 Available from: www.ada.org/prof/advocacy/medicaid/sectionD.asp.
- Bollen KA. Structural Equations with Latent Variables. New York, NY: John Wiley & Sons; 1989. [Google Scholar]
- Centers for Disease Control and Prevention. Recommendations for using fluoride to prevent and control dental caries in the United States. Morbidity and Mortality Weekly Report Recommendations and Reports. 2001;17(50 RR-14):1–42. [PubMed] [Google Scholar]
- Chavers LS, Gilbert GH, Shelton BJ. Racial and socioeconomic disparities in oral Disadvantage, a measure of oral health-related quality of life: 24-month incidence. Journal of Public Health Dentistry. 2002;62(3):140–147. doi: 10.1111/j.1752-7325.2002.tb03435.x. [DOI] [PubMed] [Google Scholar]
- D’Angelo D, Williams L, Morrow B, Cox S, Harris N, Harrison L, Posner SF, Hood JR, Zapata L. Preconception and interconception health status of women who recently gave birth to a live-born infant–Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 26 reporting areas 2004. Morbidity and Mortality Weekly Report Surveillance Summary. 2007;56(10):1–35. [PubMed] [Google Scholar]
- Dillman DA. Mail and internet surveys: The tailored design method. New York, NY: John Wiley Co; 2000. [Google Scholar]
- Gaffield ML, Colley-Gilbert BJ, Malvitz DM, Romaguera R. Oral health during pregnancy: An analysis of information collected by the pregnancy risk assessment monitoring system. Journal of the American Dental Association. 2001;132:1009–1016. doi: 10.14219/jada.archive.2001.0306. [DOI] [PubMed] [Google Scholar]
- Gerbing D, Anderson J. Monte Carlo evaluations of goodness of fit indices for structural equation models. In: Bollen K, Long J, editors. Testing structural equation models. London: UK: 1993. [Google Scholar]
- Gilbert B, Shulman HB, Fischer LA, Rogers MM. The Pregnancy Risk Assessment Monitoring System: methods and 1996 response rates from 11 States. Maternal and Child Health Journal. 1999;3:199–209. doi: 10.1023/a:1022325421844. [DOI] [PubMed] [Google Scholar]
- Grembowski D, Milgrom PM. Increasing access to dental care among Medicaid preschoool children: the access to baby and child dentistry (ABCD) Program. Public Health Reports. 2000;115(5):448–459. doi: 10.1093/phr/115.5.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet. 2003;362(9391):1225–1230. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- Grol R, Wensing M. What drives change? Barriers to and incentives for achieving evidence-based practice. Medical Journal of Australia. 2004;180(6 Suppl):S57–S60. doi: 10.5694/j.1326-5377.2004.tb05948.x. [DOI] [PubMed] [Google Scholar]
- Huebner CE, Milgrom P, Conrad D, Lee RSY. Providing dental care to pregnant patients: a survey of Oregon general dentists. Journal of the American Dental Association. 2009;140(2):211–222. doi: 10.14219/jada.archive.2009.0135. [DOI] [PubMed] [Google Scholar]
- Jared H, Boggess KA, Moss K, Boss C, Auten R, Beck J, Offenbacher S. Fetal expsoure to oral pathogens and subsequent risk for neonatal intensive care admission. Journal of Periodontology. 2009;80:873. doi: 10.1902/jop.2009.080642. [DOI] [PubMed] [Google Scholar]
- Jeffcoat MK, Geurs NC, Reddy MS, Cliver SP, Goldenerg RL, Hauth JC. Periodontal infection and preterm birth: results of a prospective study. Journal of the American Dental Association. 2001;132:875–880. doi: 10.14219/jada.archive.2001.0299. [DOI] [PubMed] [Google Scholar]
- Kobayashi M, Chi D, Coldwell SE, Domoto P, Milgrom P. The effectiveness and estimated costs of the access to baby and child dentistry program in Washington State. Journal of the American Dental Association. 2005;136(9):1257–63. doi: 10.14219/jada.archive.2005.0341. [DOI] [PubMed] [Google Scholar]
- Le M, Riedy C, Weinstein P, Milgrom P. Barriers to utilization of dental services during pregnancy: a qualitative analysis. Journal of Dentistry for Children (Chic) 2009;76(1):46–52. [PMC free article] [PubMed] [Google Scholar]
- Lydon-Rochelle MT, Krakowiak P, Hujoel PP, Peters RM. Dental care use and self-reported dental problems in relation to pregnancy. American Journal of Public Health. 2004;94(5):765–765. doi: 10.2105/ajph.94.5.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangskau KA, Arrindell B. Pregnancy and oral health: utilization of the oral health care system by pregnant women in North Dakota. Northwest Dentistry. 1996;75:23–28. [PubMed] [Google Scholar]
- McDonald RP, Ho MHR. Principles and practice in reporting structural equation analyses. Psychological Methods. 2002;7:64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- Milgrom P, Lee RSY, Huebner CE, Conrad DA. Medicaid reforms in Oregon and suboptimal utilization of dental care by women of childbearing age. Journal of the American Dental Association. 2010 doi: 10.14219/jada.archive.2010.0259. Paper accepted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milgrom P, Ludwig S, Shirtcliff RM, Smolen D, Sutherland M, Weinstein P. Providing a dental home for pregnant women: A community access program to address dental care access. Journal of Public Health Dentistry. 2008 Summer;68(3):170–173. doi: 10.1111/j.1752-7325.2007.00049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan MA, Crall J, Goldenberg RL, Schulkin J. Oral health during pregnancy. Journal of Maternal Fetal and Neonatal Medicine. 2009 June;1:1–7. doi: 10.3109/14767050902926954. [DOI] [PubMed] [Google Scholar]
- New York State Department of Health. Oral health care during pregnancy and early childhood: Practice Guidelines [Internet] New York: New York State Department of Health; 2006. Aug, [Accessed September 11, 2009]. Available from http://www.health.state.ny.us/publications/0824.pdf. [Google Scholar]
- Ressler-Maerlender J, Krishna R, Robison V. Oral health during pregnancy: current research. Journal of Womens Health. 2005;14(10):880–882. doi: 10.1089/jwh.2005.14.880. [DOI] [PubMed] [Google Scholar]
- Strafford KE, Shellhaas C, Hade EM. Provider and patient perceptions about dental care during pregnancy. Journal of Maternal and Fetal Neonatal Medicine. 2008;21(1):63–71. doi: 10.1080/14767050701796681. [DOI] [PubMed] [Google Scholar]
- Vergnes JN, Sixou M. Preterm low birth weight and maternal periodontal status: a meta-analysis. American Journal of Obstetrics and Gynecology. 2007;196:135.e1–7. doi: 10.1016/j.ajog.2006.09.028. [DOI] [PubMed] [Google Scholar]