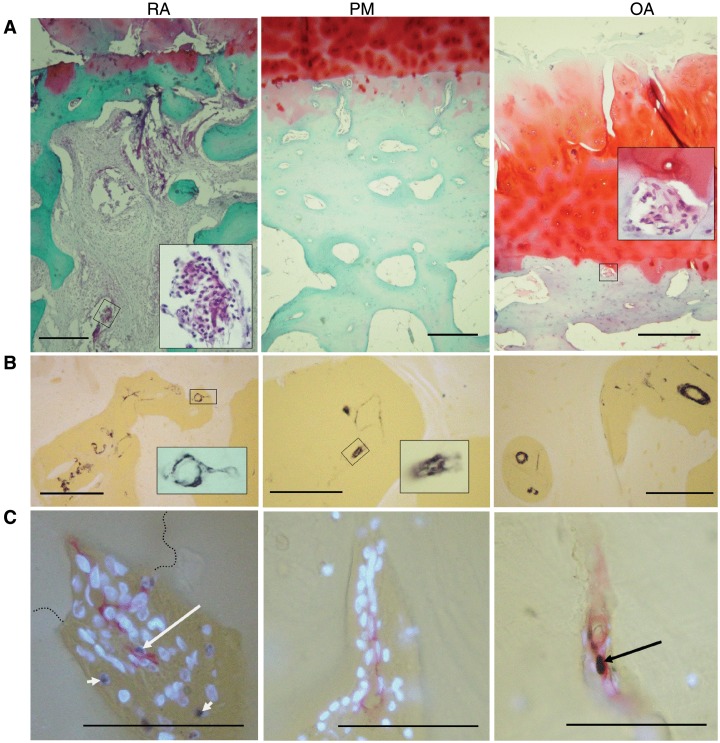
Fig. 1.
Morphology and vascularity at the osteochondral junction in RA, PM controls and OA. (A) General morphology at the osteochondral junction. RA: fibrovascular granulation tissue filling bone marrow spaces and invading the articular cartilage from below. There is proteoglycan loss and thinning of the articular cartilage and subchondral bone plate. Inset: blood vessel and inflammatory cells within the subchondral bone space. PM: normal cartilage, thick subchondral bone containing vascular channels and bone marrow spaces filled with fatty tissue. OA: fibrovascular tissue within a channel touching the tidemark (inset) as well as fibrillation, fissuring and proteoglycan depletion in cartilage at the articular surface. (B) Smooth muscle α-actin-positive cells (black) in subchondral bone spaces and associated vascular channels. Insets: positive blood vessels within a vascular channel (RA) and subchondral space (OA). (C) Vascular channels stained for CD34-positive ECs (red), PCNA-positive nuclei (black) and non-proliferating nuclei [4′-6′-diamidino-2-phenylindole (DAPI): fluorescent blue]. Proliferating ECs (long arrows) are demonstrated in a vascular channel that crosses the tidemark (broken line) in RA, and within the subchondral bone plate in OA. Proliferating non-ECs are also present (RA: short arrows). PM: vascular channel within the subchondral bone plate containing no proliferative ECs. Tissue morphology is revealed in (A) by Safranin O stain (red: proteoglycan; green: bone), with haematoxylin counterstain or (B and C) using combined transmitted and fluorescent light (blue/white: cartilage, bone and DAPI-reactive nuclei; yellow: background). Scale bars = 100 microns.