Abstract
Background
It is not known if surgeons who place women of reproductive age on thyroid hormone replacement (levothyroxine, LT4) routinely inform them of the increased LT4 demands with future pregnancy. In addition, it is not clear whether reading the 2007 Endocrine Society's “Guidelines on the Management of Thyroid Dysfunction during Pregnancy and Postpartum” influences the role of the surgeon in patient education. The objective of this study was to identify the role of the surgeon in patient education at the time of initiation of LT4 therapy.
Methods
A two-sided one-page survey was distributed to the 260 surgeons attending the 2009 American Association of Endocrine Surgeons' meeting. Of those distributed, 109 (42%) surgeons returned the survey.
Results
Although only 26/109 (23%) read the 2007 Endocrine Society's “Guidelines on the Management of Thyroid Dysfunction during Pregnancy and Postpartum,” reading the guidelines was associated with a significantly greater likelihood of informing patients of higher LT4 requirements with pregnancy (p < 0.0001). Eighty-five percent of those who read the guidelines “often” or “always” informed patients of higher LT4 requirements with future pregnancy, whereas only 44% of those who did not read the guidelines provided the same level of education. After controlling for surgeon sex, academic versus private practice, years in practice, and number of surgeries performed in 2008, the only independent predictor of patient education was reading the guidelines (p = 0.006). On multivariable analysis, surgeon volume was associated with reading the guidelines (p = 0.006). The mean number of thyroid surgeries performed by those who read the guidelines versus those who did not was 164.46 ± 16.98 versus 115.01 ± 8.27 (p = 0.005).
Conclusion
Surgeons who read the Endocrine Society's “Guidelines on the Management of Thyroid Dysfunction during Pregnancy and Postpartum” were significantly more likely to inform patients of the need for higher LT4 doses with pregnancy. Thyroid surgery volume was associated with guideline awareness.
Introduction
There is a growing body of evidence that maternal hypothyroidism can have detrimental effects on pregnancy outcome, including increased risk of miscarriage, premature delivery, low birth weight, fetal death, C-section, preeclampsia, and decreased infant intelligence quotient (IQ) (1–6). Since the fetal thyroid is not active until close to 13 weeks of gestation, the role of adequate thyroid hormone levels may be most critical during the early weeks of gestation.
There are also data that pregnancy does impact thyroid function (7), and women on thyroid hormone replacement (levothyroxine, LT4) prepregnancy often need a 30%–50% increase in dose during pregnancy (8–11). Thyroid surgery is a common cause of hypothyroidism because 100% of total thyroidectomy patients and 13%–35% of patients undergoing lobectomy require thyroid hormone replacement postsurgery (12–16). In addition, hypothyroidism secondary to thyroid surgery is associated with a larger LT4 dose requirement during pregnancy than primary hypothyroidism (10). Because of the increasing evidence supporting the potential gravity of hypothyroidism during pregnancy, in 2007 the Endocrine Society created “Guidelines on the Management of Thyroid Dysfunction during Pregnancy and Postpartum” (17).
Although it may have been assumed that the issue of thyroid hormone replacement in pregnancy only pertains to obstetricians, a recent study has shown that most pregnant women are not under obstetric care until after the optimal window for LT4 dose increase occurs (18). For women on LT4, the LT4 dose often needs to be increased by 4–6-week gestation and may require a 30%–50% increase (1,8). However, our previous work has revealed that 76% of obstetric care providers initially see patients after the optimal window for dose adjustment (18). The rate of miscarriage is high before 6 weeks of gestation (19), and many obstetric care providers schedule the initial prenatal visit close to 10 weeks of gestation when fetal heart beat can be confirmed. Although this is a logical and appropriate time to schedule prenatal visits for most patients, this missed window for LT4 dose adjustment is one explanation for why 49% of women on LT4 have thyroid-stimulating hormone levels outside goal range during the first trimester (11). Given the risks of poorly treated hypothyroidism during pregnancy (1–6) and that many of these patients are not under obstetric care at the preferred time of initial dose increase (18), prepregnancy counseling on LT4 changes during pregnancy is important. Education before conception enables a patient to be her own advocate and have thyroid function addressed at the time of confirmed conception instead of at the initial antenatal visit.
It is not known which healthcare providers provide education on the increased LT4 requirement with pregnancy, but it can be assumed that if it is not provided at the time of drug initiation, then it may not occur. Surgeons place women of reproductive age on LT4 routinely postoperatively and it is not known whether they inform them of increased LT4 demands with future pregnancy. In addition, it is not clear whether the 2007 Endocrine Society's “Guidelines on the Management of Thyroid Dysfunction during Pregnancy and Postpartum” (17) influence the role of the surgeon in patient education at the time of LT4 initiation. With the goal of determining the impact of the guidelines on surgical practice, we surveyed the surgeon attendees at the 2009 annual meeting for the American Association of Endocrine Surgeons (AAES).
Materials and Methods
The current study used physician surveys to evaluate the ability of the Endocrine Society's “Guidelines on the Management of Thyroid Dysfunction during Pregnancy and Postpartum” to influence the surgeon's role in educating patients on changes in LT4 dose with pregnancy. The University of Wisconsin Health Sciences Institutional Review Board (IRB) approved this study for IRB exemption. The survey instrument consisted of a two-sided one-page survey that was hand distributed at the registration desk at the 2009 AAES’ meeting in Madison, WI (see Supplemental Data, available online at www.liebertonline.com/thy). The focus of the survey and the method of return was also one of the first announcements at the start of the AAES meeting. There were 330 meeting attendees, but after excluding spouses, students, vendors, nurses, and nonsurgical physicians, only 260 attendees were surgeons. Of the 260 eligible attendees, 109 (42%) completed the survey. Four out of 109 had never performed thyroid surgery on a female patient aged 12–50 years and thus appropriately stopped after the first question, whereas 2 of the 109 answered questions on the front page only. The remaining 103 answered all questions.
All statistical analysis was performed with SPSS 10.0. The distribution of continuous variables was compared using analysis of variance, and chi-square statistic was used for categorical variables. Multivariable logistic regression was used to model dichotomous outcomes. Means were reported as mean ± standard error of mean, and statistical significance was set to a probability value of p < 0.05.
Results
Of the 109 surgeons who completed the survey, 87 (80%) of the surgeons worked at an academic center and 16 (15%) were in private practice. The mean number of years in practice was 10.5 ± 1.01, and the mean number of thyroid surgeries in 2008 was 126 ± 7.69. Relative to the total eligible population, there was an underrepresentation of male surgeons and of residents/fellows that completed surveys. Of the 260 surgeons present at the meeting, 177 (68%) were men and 59 (23%) were residents or fellows. Of those that completed the survey, 67/109 (62%) were men versus 36/109 (33%) women. Only 17/109 (16%) of the completed surveys were filled out by residents or fellows (Table 1).
Table 1.
Surgeon Characteristics
| Number | |
|---|---|
| Sex | |
| Male | 67/109 (61.5%) |
| Female | 36/109 (33.0%) |
| Missing data | 6/109 (5.5%) |
| Type of practice | |
| Academic | 87/109 (79.8%) |
| Private practice | 16/109 (14.7%) |
| Missing data | 6/109 (5.5%) |
| Resident or fellow | 17/109 (15.6%) |
| Mean no. of years in practice | 10.5 ± 1.01 |
| Mean no. of thyroid surgeries 2008 | 126.3 ± 7.69 |
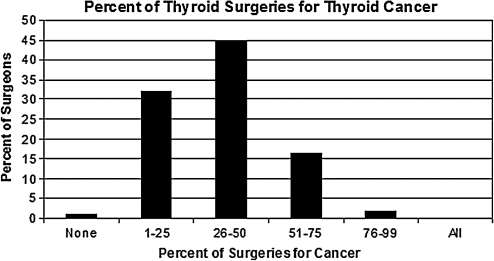
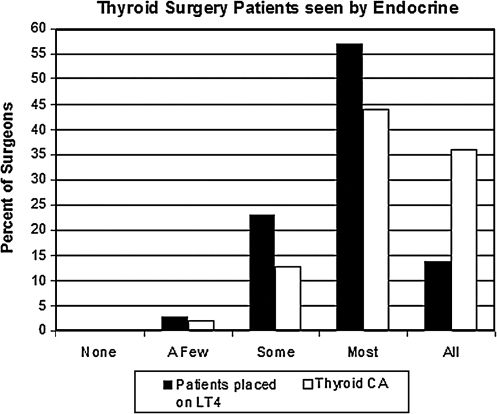
Of the thyroid surgeries performed in 2008, 85/109 (78%) surgeons reported that <50% were for thyroid cancer (Fig. 1). This indicates that >50% were for benign thyroid disease. For women placed on LT4 postoperatively, 77/109 (71%) of surgeons referred “most” or “all” patients to an endocrinologist; for women found to have thyroid cancer, 87/109 (80%) referred either “most” or “all” patients to an endocrinologist (Fig. 2).
FIG. 1.
Seventy-eight percent of endocrine surgeons reported that <50% of the thyroid surgeries performed in 2008 were for thyroid cancer.
FIG. 2.
The majority of surgeons report that “most” to “all” of their thyroid patients had either already seen an endocrinologist or were referred to an endocrinologist. LT4, levothyroxine.
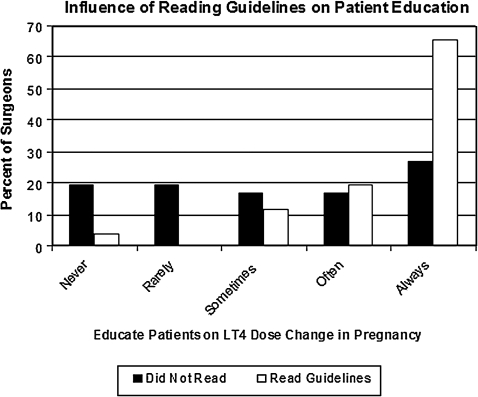
Of the participating surgeons, 26/109 (23%) read the 2007 Endocrine Society's “Guidelines on the Management of Thyroid Dysfunction during Pregnancy and Postpartum.” Reading the guidelines was associated with a significantly higher likelihood of patient education on LT4 dose changes with pregnancy (p < 0.0001). Surgeons were asked how often they inform female patients who are on thyroid hormone replacement, but not currently pregnant, that they may need a dose increase if they become pregnant. Twenty-two of the 26 surgeons (85%) who read the guidelines versus 34/77 (44%) of those who did not read the guidelines “often” or “always” informed female patients started on LT4 about increased LT4 requirements with pregnancy (Fig. 3).
FIG. 3.
Of the 109 surgeons surveyed, 26 (23%) reported reading the 2007 Endocrine Society's “Guidelines on the Management of Thyroid Dysfunction during Pregnancy and Postpartum.” Reading the guidelines was associated with a significantly higher likelihood of patient education on LT4 dose changes with pregnancy (p < 0.0001).
After controlling for surgeon sex, academic versus private practice, years in practice, and number of surgeries performed in 2008, the only independent predictor of patient education “often” or “always” was reading the guidelines (p = 0.006). On multivariable logistic regression evaluating surgeon sex, practice type, years in practice, and number of thyroid surgeries in 2008, only the total number of surgeries was predictive of reading the guidelines (Table 2) (p = 0.006). In fact, the mean number of thyroid surgeries performed by those who read the guidelines versus those who did not was 164.46 ± 16.98 compared to 115.01 ± 8.27 (Table 3) (p = 0.005).
Table 2.
Multivariable Logistic Regression
| p-Value | |
|---|---|
| Predictive of educating the patient often/always | |
| Read guidelines | 0.006a |
| Surgeon sex | 0.724 |
| Academic practice | 0.265 |
| No. of years in practice | 0.603 |
| No. of thyroid surgeries | 0.073 |
| Predictive of reading the guidelines | |
| Surgeon sex | 0.605 |
| Academic practice | 0.202 |
| No. of years in practice | 0.419 |
| No. of thyroid surgeries | 0.006a |
Significant based on p < 0.05.
Table 3.
Thyroid Surgery Volume Is Predictive of Reading the Guidelines
| Mean no. of surgeries | p-Value | |
|---|---|---|
| Read the guidelines | 164.46 ± 16.98 | 0.005 |
| Did not read | 115.01 ± 8.27 |
Discussion
All patients undergoing total thyroidectomy and up to 35% of patients undergoing lobectomy require treatment with lifelong LT4 (12–16). Women on LT4 as therapy for hypothyroidism typically need a 30%–50% increase in LT4 dose during pregnancy (8,17). Recent data have revealed that up to 49% of these women have a thyroid-stimulating hormone outside goal range during the first trimester (11). Since many women are not under obstetric care during the optimal time for initial LT4 dose adjustment, patient education preconception is vital.
In this study we surveyed the surgeon attendees at the annual AAES’ meeting in an attempt to determine exposure to and impact from the 2007 Endocrine Society's “Guidelines on the Management of Thyroid Dysfunction during Pregnancy and Postpartum.” Interestingly, 23% of endocrine surgeons reported reading the guidelines, and this is higher than the 11.5% of Wisconsin obstetricians and family physicians who read the guidelines (18). The reason for the higher rate of surgeon awareness is not clear but may be due to membership in organizations affiliated with endocrinologists, multidisciplinary clinics with endocrinologists, and, most importantly, access to the journal publishing the guidelines. Although these details were not addressed in the survey, previous studies have shown that comanagement in a multidisciplinary clinic is associated with surgical decisions that improve patient care (20).
Despite a relatively small percent of surgeons who read the guidelines, our study shows that reading the guidelines was the only independent predictor of patient education on thyroid hormone dose requirements with pregnancy. Eighty-five percent of those who read the guidelines versus 44% of those who did not read the guidelines “often” or “always” informed patients of higher LT4 requirements with future pregnancy. Provider sex, academic practice, and number of years in practice were not associated with increased patient education. When we evaluated factors predictive of reading the guidelines, surgeon volume was highly associated with guideline reading. It is well known that surgeon volume is associated with decreased morbidity and mortality (21,22). Even in the setting of thyroid surgery, a surgery with a low mortality rate, there is a confirmed relationship between surgical volume and decreased complications (23). However, as far as we know, there are no previous data showing that surgical volume is associated with increased guideline awareness and subsequent patient education.
These findings are important for several reasons. First, uncontrolled maternal hypothyroidism can result in adverse pregnancy outcome. This includes adverse effects on the mother such as preeclampsia and increased likelihood of C-section and adverse effects on the fetus such as premature delivery, low birth weight, fetal death, and decreased infant IQ (1–6). Although there is an assumption that the burden of awareness falls on the obstetrician, many patients are not under obstetric care at the optimal time for dose adjustment (18). Although surgeons would usually not be involved in dose adjustment, education at the time of initial LT4 prescription is vital and allows a patient to advocate for herself at the time of conception. In addition to informing patients of the risk of laryngeal nerve damage and permanent hypothyroidism with thyroid surgery, it may be beneficial if surgeons also inform patients of the 85% likelihood of increased LT4 demands with pregnancy (8,24). Second, as far as we know, the relationship between surgeon volume, guideline awareness, and patient education has never been illustrated. However, this is a logical association as surgical volume is likely a marker of subspecialization. Although the group of surgeons surveyed was already a subspecialized group of endocrine surgeons, even within this cohort some surgeons have more of an interest in thyroid surgery versus parathyroid or adrenal. It is probable that the surgeons with the highest thyroid surgery volume are also the ones with the most clinical interest and/or research interest in thyroid disorders. Thus, this subgroup reading the guidelines may be a self-selected population. However, volume alone was not predictive of patient education. Reading the guidelines was vital.
Although these findings are important, there are several limitations to this study. First, the majority of the surgeons surveyed have specialized in endocrine surgery; therefore, we may not be able to extrapolate these data to all general surgeons. Second, 109 (42%) of meeting attendees returned the survey and 103 (94%) completed the entire survey. Physician surveys have notoriously poor response rates with 35% not uncommon, and thus a response rate of 42% is reasonable. A previous survey study of the same cohort, AAES members, had a similar number of completed surveys, 109 (25), suggesting that there may be a set number of AAES members who participate in survey studies. Since the percent of residents and fellows completing the survey was less than the percent present at the meeting and a higher percent of female versus male surgeons completed the survey, there is a risk of nonresponse bias. Third, practice patterns were based on self-report and thus subject to respondent recall. Respondent recall can result in bias and self-inflation. For example, the mean number of thyroid surgeries performed in 2008 is much higher than the number performed by the highest volume surgeon in Maryland in 1998 (23). It is not clear if this is due to self-inflation or related to the rising demand for endocrine surgery (26). Although we do not have patient data to confirm surgery number, in other studies surgeon recall in regard to volume has correlated highly with the number of patients actually treated (20). It is not clear if self-report on patient education is also highly correlative. Finally, since most of the surgeons report that their patients were also seen by endocrinology, a lack of patient education from the surgeon does not necessarily mean that the patient did not receive the information from other sources. It is likely that the endocrinologists also educate the patients on LT4 dose changes with pregnancy. However, close to 25% of the surgeons do not consistently refer patients to endocrinology, and these patients would be particularly vulnerable without surgeon education.
In summary, this study has shown that surgeons who read the 2007 Endocrine Society's “Guidelines on the Management of Thyroid Dysfunction during Pregnancy and Postpartum” were significantly more likely to inform patients of the need for higher LT4 doses with future pregnancy. Within this highly specialized group of surgeons, surgical volume was the single predictor of guideline awareness.
This study emphasizes the role of clinical guidelines in influencing provider-initiated patient education. In the case of thyroid hormone replacement in pregnancy, when the patient may not be under obstetric care at optimal window for LT4 dose increase, there is a role for guideline dissemination to a broader population of healthcare providers.
Supplementary Material
Acknowledgments
The authors would like to thank the surgical attendees at the 2009 AAES’ Meeting who took the time to complete the survey. The University of Wisconsin Paul P. Carbone Comprehensive Cancer Center funded the data collection and supported the research of Megan Haymart through CA K12087718.
Disclosure Statement
The authors declare that there is no conflict of interest and nothing to disclose.
References
- 1.Stagnaro-Green A. Maternal thyroid disease and preterm delivery. J Clin Endocrinol Metab. 2009;94:21–25. doi: 10.1210/jc.2008-1288. [DOI] [PubMed] [Google Scholar]
- 2.Allan WC. Haddow JE. Palomaki GE. Williams JR. Mitchell ML. Hermos RJ. Faix JD. Klein RZ. Maternal thyroid deficiency and pregnancy complications: implications for population screening. J Med Screen. 2000;7:127–130. doi: 10.1136/jms.7.3.127. [DOI] [PubMed] [Google Scholar]
- 3.Antolic B. Gersak K. Verdenik I. Novak-Antolic Z. Adverse effects of thyroid dysfunction on pregnancy and pregnancy outcome: epidemiologic study in Slovenia. J Matern Fetal Neonatal Med. 2006;19:651–654. doi: 10.1080/14767050600850332. [DOI] [PubMed] [Google Scholar]
- 4.Benhadi N. Wiersinga WM. Reitsma JB. Vrijkotte TG. Bonsel GJ. Higher maternal TSH levels in pregnancy are associated with increased risk for miscarriage, fetal or neonatal death. Eur J Endocrinol. 2009;160:985–991. doi: 10.1530/EJE-08-0953. [DOI] [PubMed] [Google Scholar]
- 5.Idris I. Srinivasan R. Simm A. Page RC. Maternal hypothyroidism in early and late gestation: effects on neonatal and obstetric outcome. Clin Endocrinol (Oxf) 2005;63:560–565. doi: 10.1111/j.1365-2265.2005.02382.x. [DOI] [PubMed] [Google Scholar]
- 6.Haddow JE. Palomaki GE. Allan WC. Williams JR. Knight GJ. Gagnon J. O'Heir CE. Mitchell ML. Hermos RJ. Waisbren SE. Faix JD. Klein RZ. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med. 1999;341:549–555. doi: 10.1056/NEJM199908193410801. [DOI] [PubMed] [Google Scholar]
- 7.Glinoer D. de Nayer P. Bourdoux P. Lemone M. Robyn C. van Steirteghem A. Kinthaert J. Lejeune B. Regulation of maternal thyroid during pregnancy. J Clin Endocrinol Metab. 1990;71:276–287. doi: 10.1210/jcem-71-2-276. [DOI] [PubMed] [Google Scholar]
- 8.Alexander EK. Marqusee E. Lawrence J. Jarolim P. Fischer GA. Larsen PR. Timing and magnitude of increases in levothyroxine requirements during pregnancy in women with hypothyroidism. N Engl J Med. 2004;351:241–249. doi: 10.1056/NEJMoa040079. [DOI] [PubMed] [Google Scholar]
- 9.Mandel SJ. Larsen PR. Seely EW. Brent GA. Increased need for thyroxine during pregnancy in women with primary hypothyroidism. N Engl J Med. 1990;323:91–96. doi: 10.1056/NEJM199007123230204. [DOI] [PubMed] [Google Scholar]
- 10.Loh JA. Wartofsky L. Jonklaas J. Burman KD. The magnitude of increased levothyroxine requirements in hypothyroid pregnant women depends upon the etiology of the hypothyroidism. Thyroid. 2009;19:269–275. doi: 10.1089/thy.2008.0413. [DOI] [PubMed] [Google Scholar]
- 11.Hallengren B. Lantz M. Andreasson B. Grennert L. Pregnant women on thyroxine substitution are often dysregulated in early pregnancy. Thyroid. 2009;19:391–394. doi: 10.1089/thy.2008.0206. [DOI] [PubMed] [Google Scholar]
- 12.Piper HG. Bugis SP. Wilkins GE. Walker BA. Wiseman S. Baliski CR. Detecting, defining hypothyroidism after hemithyroidectomy. Am J Surg. 2005;189:587–591. doi: 10.1016/j.amjsurg.2005.01.038. discussion 591. [DOI] [PubMed] [Google Scholar]
- 13.Wormald R. Sheahan P. Rowley S. Rizkalla H. Toner M. Timon C. Hemithyroidectomy for benign thyroid disease: who needs follow-up for hypothyroidism? Clin Otolaryngol. 2008;33:587–591. doi: 10.1111/j.1749-4486.2008.01794.x. [DOI] [PubMed] [Google Scholar]
- 14.McHenry CR. Slusarczyk SJ. Hypothyroidisim following hemithyroidectomy: incidence, risk factors, and management. Surgery. 2000;128:994–998. doi: 10.1067/msy.2000.110242. [DOI] [PubMed] [Google Scholar]
- 15.De Carlucci D., Jr. Tavares MR. Obara MT. Martins LA. Hojaij FC. Cernea CR. Thyroid function after unilateral total lobectomy: risk factors for postoperative hypothyroidism. Arch Otolaryngol Head Neck Surg. 2008;134:1076–1079. doi: 10.1001/archotol.134.10.1076. [DOI] [PubMed] [Google Scholar]
- 16.Stoll SJ. Pitt SC. Liu J. Schaefer S. Sippel RS. Chen H. Thyroid hormone replacement after thyroid lobectomy. Surgery. 2009;146:554–558. doi: 10.1016/j.surg.2009.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abalovich M. Amino N. Barbour LA. Cobin RH. De Groot LJ. Glinoer D. Mandel SJ. Stagnaro-Green A. Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2007;92:S1–S47. doi: 10.1210/jc.2007-0141. [DOI] [PubMed] [Google Scholar]
- 18.Haymart M. The role of clinical guidelines in patient care: thyroid hormone replacement in women of reproductive age. Thyroid. 2009;20:301–307. doi: 10.1089/thy.2009.0321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boklage CE. Survival probability of human conceptions from fertilization to term. Int J Fertil. 1990;35:75. 79–80, 81–94. [PubMed] [Google Scholar]
- 20.Alderman AK. Hawley ST. Waljee J. Mujahid M. Morrow M. Katz SJ. Correlates of referral practices of general surgeons to plastic surgeons for mastectomy reconstruction. Cancer. 2007;109:1715–1720. doi: 10.1002/cncr.22598. [DOI] [PubMed] [Google Scholar]
- 21.Birkmeyer JD. Stukel TA. Siewers AE. Goodney PP. Wennberg DE. Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–2127. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 22.Dimick JB. Birkmeyer JD. Upchurch GR., Jr. Measuring surgical quality: what's the role of provider volume? World J Surg. 2005;29:1217–1221. doi: 10.1007/s00268-005-7989-4. [DOI] [PubMed] [Google Scholar]
- 23.Sosa JA. Bowman HM. Tielsch JM. Powe NR. Gordon TA. Udelsman R. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998;228:320–330. doi: 10.1097/00000658-199809000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verga U. Bergamaschi S. Cortelazzi D. Ronzoni S. Marconi AM. Beck-Peccoz P. Adjustment of L-T4 substitutive therapy in pregnant women with subclinical, overt or post-ablative hypothyroidism. Clin Endocrinol (Oxf) 2009;70:798–802. doi: 10.1111/j.1365-2265.2008.03398.x. [DOI] [PubMed] [Google Scholar]
- 25.Sosa JA. Powe NR. Levine MA. Bowman HM. Zeiger MA. Udelsman R. Profile of a clinical practice: thresholds for surgery and surgical outcomes for patients with primary hyperparathyroidism: a national survey of endocrine surgeons. J Clin Endocrinol Metab. 1998;83:2658–2665. doi: 10.1210/jcem.83.8.5006. [DOI] [PubMed] [Google Scholar]
- 26.Sosa JA. Wang TS. Yeo HL. Mehta PJ. Boudourakis L. Udelsman R. Roman SA. The maturation of a specialty: workforce projections for endocrine surgery. Surgery. 2007;142:876–883. doi: 10.1016/j.surg.2007.09.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.