Abstract
Intramedullary spinal cord metastases are very rare. Patients with breast cancer as the primary source of intramedullary spinal cord metastases tend to do better than other types of cancer. We report the very unusual case of a woman with breast cancer who had two separate episodes of intramedullary spinal cord metastasis.
Keywords: Intramedullary, Cervical, Thoracolumbar, Metastases, Breast cancer, Surgical treatment
INTRODUCTION
Intramedullary spinal cord metastases (ISCM) are rare presentation of cancer. The frequency of ISCM is reported to be 0.9-2.1% in all symptomatic metastatic tumors and only 4% to 9% of all spinal cord tumors.3-5,16,18) In 1,066 patients with disseminated cancer, Chason et al. prospectively examined the entire neuraxis at necropsy. Two-hundred cases were found to have intraparenchymal central nervous system (CNS) metastases (18.3%), and in 171 of 200 cases, multiple sites of CNS involvement were documented. ISCM were delineated in 10 of 200 patients with CNS metastasis; overall, intramedullary metastases were recognized in less than 1% of their carefully studied patients with cancer2). Grem et al.8) reviewed the records from 1980 through 1984 at the University of Wiscontin and then reported the 55 cases of ISCM. Lung cancer was 27%, and breast cancer occurred next in frequency, 14.5%. As a result, breast is one of most common primary sources4). We report the very unusual case of a single patient with two separate episodes of intramedullary spinal cord metastasis in breast cancer with a review of the pertinent literature.
CASE REPORT
A 45-year-old woman had insidious onset of numbness and paresthesia of the entire left hemibody below the C7 dermatome. On physical examination, she had a spastic left hemiparesis and was diffusely hyperreflexic. Sensory examination showed absent pain and temperature senses in the left hemibody below the C7 dermatome, with preserved sense of discriminatory touch. Magnetic resonance (MR) imaging of whole spine was performed, which clearly revealed a solid round mass occupying almost the entire spinal cord at C6 with maximum diameter of 2.5 cm (Fig. 1). The lesion was homogeneously hyperintense in T1-weighted images and was enhanced homogeneously with intravenous contrast. Her past medical history was significant for a right breast mass diagnosed as infiltrating ductal carcinoma 6 years earlier (Fig. 3A, B). At the time of initial presentation there was no evidence of metastasis to brain, lung, liver, or bones by computer tomography (CT) scan and whole body bone scan (WBBS). The patient had radical mastectomy. The initial medical therapy consisted of a tamoxifen and oral 5-fluoruracil (FU) regimen with a good response. Re-staging work-up revealed recurrence on the chest wall one year after initial diagnosis. The patient had done radiation therapy and six cycles of chemotherapy with CMF (cyclophosphamide, methotrexate, and 5-fluorouracil) regimen. The patient had been doing well for 6 years after the treatment without recurrence and metastasis. Surgical resection was performed for ISCM considering the possibility of metastatic lesion. Cervical ISCM was revealed as metastatic breast carcinoma on the pathologic report (Fig. 3C, D). Adjuvant chemotherapy consisted of a tamoxifen and oral 5-FU regimen without radiotherapy for cervical ISCM. The patient also had metastatic brain lesions at the time of diagnosis. Gamma knife surgery was performed for metastatic brain lesions because the patient's condition was relatively well. The patient had been well without recurrence and metastasis in other organs for 2 year.
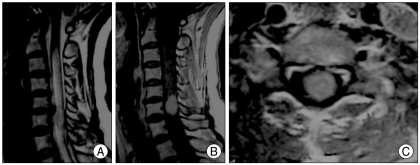
Fig. 1.
Cervical MR images show a solid round mass occupying almost the entire spinal cord at C6 with homogeneous contrast enhancement. A and B show intradural-extramedullary (IDEM) mass at C6 on T2WI & T1WI with contrast, respectively. C shows IDEM mass at C6 axial cut.
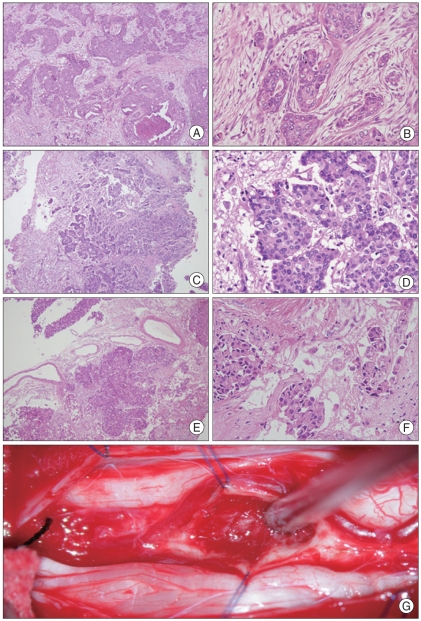
Fig. 3.
The primary tumor was infiltrating ductal carcinoma of breast. The lower power view (A : 40×) shows infiltrating carcinoma with ductal carcinoma in situ. High power view (B :×200) shows infiltrating carcinoma with focal tubular patterns. The histological features of the cervical ISCM and conus medullaris ISCM second metastasis to the spinal cord are identical to the primary tumor. C (×40) and D (×200) : Cervical ISCM. E (×40) and F (×200) : Conus medullaris ISCM. G shows intraoperative finding of conus medullaris ISCM.
Pain on both legs was developed 2 years after the surgery for cervical ISCM. This symptom was associated with a lancinating pain in both anterior and lateral aspects of thigh, both leg weakness, and loss of bowel and bladder control. MRI of whole spine revealed a solid intramedullary mass at T12-L1 level with a maximum diameter of 3 cm (Fig. 2). The other metastatic lesions such as brain and cervical ISCM were locally well controlled. We performed surgical resection for thoracolumbar ISCM again. (Fig. 3E, F) The patient had no neurological improvement after the surgery for thoracolumbar ISCM and the performance status of the patient deteriorated gradually and she died 2 months later. We couldn't treat the patient any further because of her poor general condition.
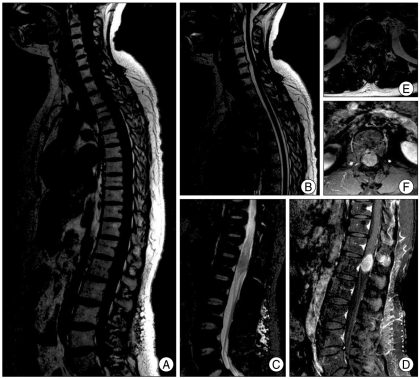
Fig. 2.
MRI of whole spine revealing a solid intramedullary mass at T12-L1 level 2 years after the surgery for cervical ISCM. A and B show no recurrence and residual mass in cervical area. A, C, D, E, and F show a solid intramedullary mass at T12-L1 level with homogeneous contrast enhancement.
DISCUSSION
Invasive ductal carcinoma (IDC) is the most common type of the breast cancer, which has been reported to constitute approximately 70-85% of all invasive breast carcinoma15). Usually, IDC can metastasize to the lungs, liver, bones, and central nervous system (CNS), especially brain17). The metastasis of IDC to the CNS is generally a late feature of metastatic disease, and is thought to be hematogenous in origin17). Among them, about 90% cause brain metastases, and only 8% spread to the leptomeninges12). Once the tumor cells reach the leptomeninges, they are thought to spread to the spinal cord via the CSF17).
ISCM is an unusual presentation of cancer. The most common organ of primary cause of metastatic spine tumor is lung, followed by breast8). Breast cancer is a common primary cause of metastatic spine tumor4). ISCM are very unusual presentation of breast cancer. The incidence of intramedullary tumors in various studies of metastases affecting the spinal cord ranges from 0.1% to 6% incidence of central nervous system metastases, usually multifocal4,13,14). Metastatic tumors are mostly localized in the brain followed by the cerebellum, dura mater, brain stem, and intramedullary spinal cord12). In a later review of ISCM by Edelson et al.6) the incidence if ISCM was found to be 3.4%. It is usually associated with widespread central nervous system (CNS) and systemic disease, although it can be the presenting manifestation of a previously undiagnosed neoplasm3).
Connolly, et al.3) presented the frequent sites of ISCM15). Metastases affect the cervical (24%), thoracic (22%), and lumbar (28%) spinal cords equally, and involve multiple levels in 19% of cases. Grem et al.14) reviewed the records from 1980 through 1984 at the University of Wiscontin and then reported the 55 cases of ISCM, and presented that thoracic level was most commonly affected (42%), followed by cervical (31%), lumbar (15%), and cervico thoracic (6%) and thoracolumbar (6%).
Patients usually present with back pain and signs and symptoms of spinal cord compression, such as hemiparesis or hemisensory impairments. Most patients present with myelopathy as the first manifestation. Symptoms progress rapidly and often lead to complete paraplegia. Although wide spectrum of symptoms and signs could be in difficulty for proper diagnosis, ISCMs should be considered in breast cancer patients with these clinical features. MRI may be the main diagnostic tool for intramedullary lesions as it is very sensitive, although non-specific, in distinguishing between ISCM and primary cord tumors.
Most patients with ISCM show rapid progression of clinical course and have an extremely poor prognosis. Optimal treatment in patients with ISCM remains controversial. The treatment modalities for ISCM include radiation therapy, chemotherapy, and surgical resection. The first of all, treatment for ISCM has been irradiation6). Radiation therapy could be an effective treatment for ISCM and the outcome has depended on the stage and severity of neurologic deterioration14). It may save spinal cord function or reverse temporary dysfunction in the early clinical course. The second treatment modality for ISCM is the microsurgical treatment. Microsurgical treatment with maximal removal of the lesion, with the goal of preserving existing function, is considered the treatment of choice, as it may improve survival and quality of life7,9). Kalayci et al.10) reported that early surgical resection resulted in the improvement of neurological deficit and in the quality of life of the patient. Surgery is followed by post-operative radiation therapy, especially when post-operative MRI demonstrates incomplete removal of the lesion. In this case, the patient showed two separate episodes of ISCM. This patient had slow progression after the surgery for first episode of ISCM. We performed the surgery because the patient's general condition was relatively good. Fortunately, the patient had been well for 2 years without any neurological deficit after the first surgery for ISCM.
Regarding the treatment option as in our case, we couldn't find similar cases in the literature due to low incidence of such cases. However, the incidence of metastases is increasing in these days due to the increase of the survival rate of malignant patients, thus the optimal treatment guidelines for treating these patients should be sought carefully. The treatment modality should be decided based on patient's condition and performance status at the time of diagnosis, such as timing of presentation in relation to initial breast cancer, degree of neurological deficits, life expectancy, and other medical conditions.
CONCLUSION
In this case, the patient had two separate episodes of ISCM. It is extremely rare. ISCMs become more common and the incidence is getting increased with advancement of imaging modality and more prolonged survival of metastatic breast cancer patients. Although optimal treatment in patients with ISCM remains controversial, microsurgical treatment with maximal removal of the lesion, with the goal of preserving existing function, is considered the treatment of choice regarding patient's condition at the time of diagnosis, as it may improve survival and quality of life.
References
- 1.Borst MJ, Ingold JA. Metastatic patterns of invasive lobular versus invasive ductal carcinoma of the breast. Surgery. 1993;114:637–641. discussion 641-642. [PubMed] [Google Scholar]
- 2.Chason JL, Walker FB, Landers JW. Metastatic carcinoma in the central nervous system and dorsal root ganglia. A prospective autopsy study. Cancer. 1963;16:781–787. doi: 10.1002/1097-0142(196306)16:6<781::aid-cncr2820160614>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 3.Connolly ES, Jr, Winfree CJ, McCormick PC, Cruz M, Stein BM. Intramedullary spinal cord metastasis: report of three cases and review of the literature. Surg Neurol. 1996;46:329–337. doi: 10.1016/s0090-3019(96)00162-0. discussion 337-338. [DOI] [PubMed] [Google Scholar]
- 4.Costigan DA, Winkelman MD. Intramedullary spinal cord metastasis. A clinicopathological study of 13 cases. J Neurosurg. 1985;62:227–233. doi: 10.3171/jns.1985.62.2.0227. [DOI] [PubMed] [Google Scholar]
- 5.Donovan DJ, Freeman JH. Solitary intramedullary spinal cord tumor presenting as the initial manifestation of metastatic renal cell carcinoma : case report. Spine (Phila Pa 1976) 2006;31:E460–E463. doi: 10.1097/01.brs.0000222022.67502.4e. [DOI] [PubMed] [Google Scholar]
- 6.Edelson RN, Deck MD, Posner JB. Intramedullary spinal cord metastases. Clinical and radiographic findings in nine cases. Neurology. 1972;22:1222–1231. doi: 10.1212/wnl.22.12.1222. [DOI] [PubMed] [Google Scholar]
- 7.Findlay JM, Bernstein M, Vanderlinden RG, Resch L. Microsurgical resection of solitary intramedullary spinal cord metastases. Neurosurgery. 1987;21:911–915. doi: 10.1227/00006123-198712000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Grem JL, Burgess J, Trump DL. Clinical features and natural history of intramedullary spinal cord metastasis. Cancer. 1985;56:2305–2314. doi: 10.1002/1097-0142(19851101)56:9<2305::aid-cncr2820560928>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 9.Hejazi N, Hassler W. Microsurgical treatment of intramedullary spinal cord tumors. Neurol Med Chir (Tokyo) 1998;38:266–271. doi: 10.2176/nmc.38.266. discussion 271-273. [DOI] [PubMed] [Google Scholar]
- 10.Kalayci M, Cağavi F, Gül S, Yenidünya S, Açikgöz B. Intramedullary spinal cord metastases : diagnosis and treatment - an illustrated review. Acta Neurochir (Wien) 2004;146:1347–1354. doi: 10.1007/s00701-004-0386-1. discussion 1354. [DOI] [PubMed] [Google Scholar]
- 11.Kesari S, Batchelor TT. Leptomeningeal metastases. Neurol Clin. 2003;21:25–66. doi: 10.1016/s0733-8619(02)00032-4. [DOI] [PubMed] [Google Scholar]
- 12.Kosmas C, Koumpou M, Nikolaou M, Katselis J, Soukouli G, Markoutsaki N, et al. Intramedullary spinal cord metastases in breast cancer : report of four cases and review of the literature. J Neurooncol. 2005;71:67–72. doi: 10.1007/s11060-004-9177-z. [DOI] [PubMed] [Google Scholar]
- 13.Lee SS, Kim MK, Sym SJ, Kim SW, Kim WK, Kim SB, et al. Intramedullary spinal cord metastases : a single-institution experience. J Neurooncol. 2007;84:85–89. doi: 10.1007/s11060-007-9345-z. [DOI] [PubMed] [Google Scholar]
- 14.Schiff D, O'Neill BP. Intramedullary spinal cord metastases : clinical features and treatment outcome. Neurology. 1996;47:906–912. doi: 10.1212/wnl.47.4.906. [DOI] [PubMed] [Google Scholar]
- 15.Toikkanen S, Pylkkanen L, Joensuu H. Invasive carcinoma of the breast has better short- and long-term survival than invasive ductal carcinoma. Br J Cancer. 1997;76:1234–1240. doi: 10.1038/bjc.1997.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watanabe M, Nomura T, Toh E, Sato M, Mochida J. Intramedullary spinal cord metastasis : a clinical and imaging study of seven patients. J Spinal Disord Tech. 2006;19:43–47. doi: 10.1097/01.bsd.0000188661.08342.2a. [DOI] [PubMed] [Google Scholar]
- 17.Weil RJ, Palmieri DC, Bronder JL, Stark AM, Steeg PS. Breast cancer metastasis to the central nervous system. Am J Pathol. 2005;167:913–920. doi: 10.1016/S0002-9440(10)61180-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang JW, Lee JI. Intramedullary spinal cord metastasis : case report. J Korean Neurosurg Soc. 2003;33:422–424. [Google Scholar]