Abstract
There is a large body of scientific evidence that has been confirmed in randomized controlled trials indicating a cardioprotective effect for omega-3 fatty acids from fish. For alpha-linolenic acid (ALA), which is the omega-3 fatty acid from plants, the relation to cardiovascular health is less clear. We reviewed the recent literature on dietary ALA intake, ALA tissue concentrations, and cardiovascular health in humans. Short-term trials (6–12 weeks) in generally healthy participants mostly showed no or inconsistent effects of ALA intake (1.2–3.6 g/d) on blood lipids, low-density lipoprotein oxidation, lipoprotein(a), and apolipoproteins A-I and B. Studies of ALA in relation to inflammatory markers and glucose metabolism yielded conflicting results. With regard to clinical cardiovascular outcomes, there is observational evidence for a protective effect against nonfatal myocardial infarction. However, no protective associations were observed between ALA status and risk of heart failure, atrial fibrillation, and sudden death. Findings from long-term trials of ALA supplementation are awaited to answer the question whether food-based or higher doses of ALA could be important for cardiovascular health in cardiac patients and the general population.
Keywords: Alpha-linolenic acid, Cardiovascular diseases, Coronary heart disease, Cardiovascular risk factors
Introduction
Omega-3 (n-3) fatty acids can be divided into alpha-linolenic acid (ALA; C18:3n-3) from plant origin, and eicosapentaenoic acid (EPA; C20:5n-3) and docosahexaenoic acid (DHA; C22:6n-3) from seafood. Because the human body lacks the enzymatic capacity to synthesize ALA, it is essential to obtain it from the diet.
The estimated average ALA intake in the United States and most European countries is 1.3 to 1.7 g/d [1–3]. The Institute of Medicine (IOM) of the National Academies established Dietary Reference Intakes for macronutrients in 2002 [4]. For ALA, the Adequate Intake (AI) was set at 1.6 g/d for men and 1.1 g/d for women [4]. The IOM noted that intakes of n-3 fatty acids above the AI may confer additional health benefits, especially with respect to cardiovascular health. Many advisory boards consider ALA intakes greater than 1.5 g/d important for human health [1]. To achieve an adequate ALA intake, food sources such as flaxseed and flaxseed oil, walnuts and walnut oil, and canola and soybean oil are recommended.
For EPA and DHA from fish, there is a vast amount of epidemiologic evidence indicating a cardioprotective effect. This evidence has been confirmed in randomized controlled trials [5–8]. For ALA, the relation with cardiovascular health is less clear. Several large, prospective cohort studies in the United States have shown inverse associations of ALA intake with risk of cardiovascular diseases, but other epidemiologic studies have been inconclusive [9–11]. A meta-analysis of observational studies showed that increased intake of ALA might reduce coronary heart disease (CHD) mortality by 21%, although this was not statistically significant [11]. In the Lyon Diet Heart Study, a randomized controlled trial in coronary patients, consumption of a Mediterranean-type diet that included an additional daily intake of roughly 1 g of ALA significantly decreased the risk of cardiac death and nonfatal myocardial infarction (MI) by more than 60% [12]. This study, however, was not specifically designed to assess the effect of ALA supplementation, and many dietary factors differed between the experimental and control group. Since then, no randomized controlled trials of ALA and cardiovascular events have been published. This article summarizes the current literature (published after 2008) on dietary ALA intake, ALA tissue levels, and cardiovascular health in humans.
Effect of ALA Supplementation on Cardiovascular Risk Factors
Several trials have recently been published on the effect of ALA supplementation on blood lipids, inflammatory markers, and other indicators of cardiovascular health (Table 1) [13, 14•, 15–17, 18••]. Trials were mostly of relatively short duration (6–12 weeks) and ALA doses ranged from 1.2 to 3.6 g/d. There was one long-term trial (52 weeks) in which a high ALA dose of 8.8 g/d was given [18••]. Increased ALA intake was achieved by means of flaxseed oil [13, 15], ALA-enriched margarine [14•], or other ALA-enriched foods [16, 17, 18••].
Table 1.
Overview of randomized controlled trials of increased alpha-linolenic acid intake and cardiovascular risk factors published between January 2008 and June 2010
| Study/year | Population | Design | Outcome for ALA |
|---|---|---|---|
| Kaul et al. [13]/2008 | 88 healthy non-smoking Canadian men and premenopausal women, aged 33 y | 12-week, double-blind, parallel randomized controlled trial; sunflower oil (placebo), flaxseed oil (∼1 g/d ALA), hempseed oil (0.3 g/d ALA), or fish oil (0.6 g/d EPA+DHA) | Plasma ALA levels increased (P < 0.05) after 6 wk; no differences in total cholesterol, LDL-C, HDL-C, TG, LDL oxidation, platelet aggregation, or inflammation markers (CRP, TNF-α) |
| Egert et al. [14•]/2009 | 79 healthy non-smoking German men and premenopausal women, aged 19–45 y | 6-week, double-blind, parallel randomized controlled trial; ALA (3.4 g/d), EPA (2.2 g/d), or DHA (2.3 g/d) via enriched margarines | LDL-ALA levels increased (P < 0.05); fasting serum TG decreased (P < 0.05); no differences in total cholesterol, LDL-C, or HDL-C |
| Barceló-Coblijn et al. [15]/2008 | 62 American men >40 y of age | 12-week, parallel randomized controlled trial; different doses of flax oil, fish oil, and sunflower oil in capsules; ALA doses were 1.2 g/d, 2.4 g/d, and 3.6 g/d | 2.4 and 3.6 g/d of ALA significantly increased erythrocyte ALA and EPA levels; no differences in inflammation markers (CRP, TNF-α, sVCAM-1), total cholesterol, TG, or HDL-C |
| Sioen et al. [16]/2009 | 59 healthy Belgian male prisoners | 12-week single-blind study; diet with 3.2 g/d extra ALA | No effect on waist circumference, weight, BMI, systolic blood pressure; diastolic blood pressure decreased and HDL-C increased in non-smokers |
| Bloedon et al. [17]/2008 | 62 men and post-menopausal women from Philadelphia, aged 44–75 y, with hypercholesterolemia | 10-week, blind, parallel randomized controlled trial with low-fat diet with extra flaxseed or with wheat bran (control); ALA dose of 3.4 g/d | Serum ALA levels increased; LDL-C was decreased after 5 wk but not after 10 wk; lipoprotein(a) was decreased and insulin sensitivity (HOMA index) improved; no effect on inflammation (IL-6, hs-CRP) or oxidative stress (ox-LDL, urinary isoprostane); HDL-C was reduced |
| Dodin et al. [18••]/2008 | 199 Canadian menopausal women, aged 49–65 y | 52-week, blind parallel trial; 40 g/d flaxseed or wheat germ; ALA dose of 8.8 g/d | Serum ALA levels increased; modest effects on apolipoproteins A-I and B; no effects on LDL electrophoretic characteristics or markers of hemostasis and inflammation |
ALA alpha-linolenic acid; BMI body mass index; DHA docosahexaenoic acid; EPA eicosapentaenoic acid; HDL-C high-density lipoprotein cholesterol; HOMA homeostasis model assessment; hs-CRP high-sensitivity C-reactive protein; IL-6 interleukin-6; LDL-C low-density lipoprotein cholesterol; sVCAM-1 soluble vascular cell adhesion molecule-1; TG triglycerides; TNF tumor necrosis factor
Kaul et al. [13] studied the effects of low-dose supplementation (2 g/d, by means of capsules) of flaxseed oil, fish oil, and hempseed oil in 86 healthy Canadian men and women about 34 years of age in a 12-week, randomized, double-blind, placebo-controlled trial. Flaxseed oil (ALA dose ∼1 g/d) increased plasma ALA by 30% to 40%, had a small nonsignificant effect on plasma EPA (7%–8%), and no effect on plasma DHA. None of the treatments affected serum total, low-density lipoprotein (LDL), or high-density lipoprotein (HDL) cholesterol, triglycerides, LDL oxidation, platelet aggregation, or inflammatory markers [13]. In another randomized trial in 62 healthy men approximately 40 years of age in the United States, participants were randomized to flax oil (ALA doses of 1.2, 2.4, or 3.6 g/d), fish oil (0.6 or 1.2 g/d), or sunflower oil for 12 weeks [15]. Increasing doses of flax oil caused elevation of the ALA content in erythrocyte membranes by 40% to 80%, and also of EPA (20%–35%), but not of DHA. None of the treatments altered plasma inflammatory markers (C-reactive protein [CRP], tumor necrosis factor [TNF]-α, soluble vascular cell adhesion molecule-1 [sVCAM-1]), plasma total or HDL cholesterol, or triglycerides [15].
Bloedon et al. [17] enrolled 62 American men and post-menopausal women aged 44 to 75 years with hypercholesterolemia. All participants were on a low-fat, low-cholesterol diet and subsequently randomized to flax-based or wheat-based products for 10 weeks. ALA intake in the flaxseed group was 3.4 g/d higher than in the control group. Flax-based products improved insulin sensitivity and reduced plasma LDL cholesterol by 7% to 13% and lipoprotein(a) by 14% compared with wheat-based products. In men, there was also a decrease in HDL cholesterol. Treatment had no effect on markers of inflammation (interleukin-6, high-sensitivity CRP) or oxidative stress (oxidized LDL, urinary isoprostanes) [17]. The extent to which the observed effects of the flax-based diet were due to its ALA content or other components of flax seeds is not clear.
In a single-blind, 12-week field study among 59 healthy male prisoners (mean age of 42 years) in Belgium, daily ALA intake was increased from 2.8 to 4.9 g/d by means of ALA-enriched foods without changing the linoleic acid content of the diet [16]. All individuals were first on a regular diet, which was followed by an ALA-rich diet, and no randomization was applied. EPA and DHA, but not ALA, were assessed in platelet phospholipids, which showed no significant changes during ALA intervention. Body weight, waist circumference, and systolic blood pressure did not change, and there were no effects of ALA on plasma total and LDL cholesterol, triglycerides, apolipoproteins A-I and B, glucose, and CRP. Diastolic blood pressure, however, significantly decreased by 3 mm Hg [16].
Egert et al. [14•] studied the effects of increased intake of ALA, EPA, and DHA in a 6-week parallel trial in 74 German normolipidemic men and women aged 19 to 43 years. Participants were randomly assigned to trial margarines that provided additional ALA (3.4 g/d), EPA (2.2 g/d), or DHA (2.3 g/d). No placebo group was included. In the ALA group, the ALA content of LDL particles increased by 178% and the EPA content increased by 36%, whereas DHA remained unchanged. Serum total and LDL cholesterol were not affected by the different treatments. Fasting serum triglycerides significantly decreased with EPA (−0.14 mmol/L), DHA (−0.30 mmol/L), and ALA (−0.17 mmol/L). DHA intake significantly increased serum HDL cholesterol, whereas no changes were found with ALA or EPA intake [14•].
Finally, Dodin et al. [18••] evaluated the effect of flaxseed on markers of cardiovascular disease risk in 169 healthy menopausal Canadian women who were randomly assigned to 40 g/d of flaxseed-based products or wheat-based products for 12 months. In the active-treatment group, ALA intake was increased by 8.8 g/d. Flaxseed products increased plasma ALA by 85% and plasma EPA by 51% after 12 months of intake, which differed significantly from wheat-based intervention (12% and 29%, respectively). Changes in plasma DHA were similar in both groups. The 12-month intervention with flaxseed had significant effects on body weight (−0.8 kg) and serum total cholesterol (−0.20 mmol/L) and a small adverse effect on HDL cholesterol (−0.08 mmol/L). LDL cholesterol was reduced by 0.13 mmol/L (P = 0.09). Apolipoproteins A-I and B increased in both groups, but less during flaxseed-based than wheat-based intervention. Treatment had no effect on plasma lipoprotein(a), fibrinogen, CRP, insulin, glucose, or LDL peak particle size. The effect of ALA on plasma triglycerides was not reported [18••].
Observational Studies on ALA Intake and Cardiovascular Risk
Zatónski et al. [2] examined trends in CHD mortality in 11 Eastern European countries and linked these figures to national data on vegetable oil consumption after 1990. They showed the strongest decline in CHD mortality in countries where rapeseed oil (9% ALA) rather than sunflower oil (0% ALA) was used. Although these data are suggestive for a beneficial effect of ALA, no definite conclusions can be drawn because the countries also differed in many other aspects that could impact cardiovascular health. Cross-country comparisons based on aggregate data cannot be adjusted for potential confounders, (eg, socioeconomic status, lifestyle and other dietary components) and should be considered for hypothesis generation only.
In Costa Rica, soybean oil has been substituted for palm oil since the 1980s, which has led to an increase in ALA intake. Campos et al. [19••] performed a case–control study in 3638 Costa Rican individuals to examine the association between ALA and nonfatal MI (Fig. 1). Participants were matched for age, sex, and area of residence. ALA intake was assessed by a 135-item food frequency questionnaire and ranged from 1.1 to 2.4 g/d (mean, 1.6 g/d) in this population. Dietary ALA was inversely associated with nonfatal MI, with odds ratios indicating a 39% reduced risk for approximately a 0.6-g/d difference in intake. The relationship between ALA and MI was nonlinear and mainly confined to the lowest levels of intake. Dietary ALA intake in this study correlated well with ALA in adipose tissue, plasma, and erythrocytes, but poorly with biomarkers of EPA and DHA, suggesting a direct cardioprotective effect of ALA rather than via conversion to long-chain n-3 fatty acids [19••].
Fig. 1.
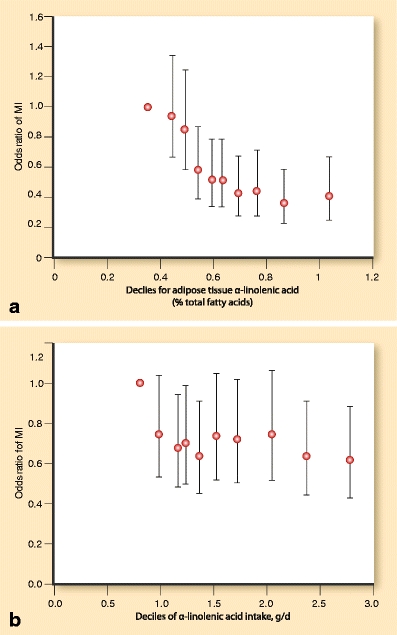
Odds ratios and 95% confidence intervals for nonfatal myocardial infarction (MI) by deciles of alpha-linolenic acid in adipose tissue (a) or intake (b) in a case–control study of 3638 men and women in Costa Rica. Data were adjusted for smoking status, physical activity, household income, history of diabetes mellitus, history of hypertension, waist-to-hip ratio, saturated fat intake, and linoleic and trans fatty acids in adipose tissue. (From Campos et al. [19••]; with permission)
An anti-inflammatory action of ALA has been proposed as an explanation for the inverse association with cardiovascular diseases found in the case–control study in Costa Rica [19••], although negative findings on ALA and inflammatory markers have been reported by others [9]. Dai et al. [20•] examined habitual ALA intake and plasma concentrations of inflammatory markers, including IL-6 and sIL-6R, in 353 middle-aged men in the United States who were recruited from a twin registry. ALA intake, assessed by the Willett questionnaire, ranged from 0.2 to 2 g/d, and was significantly inversely related to plasma sIL-6R independent of shared genetic factors and a wide range of potential confounders. A twin with a 1-g higher ALA intake (equivalent to one tablespoon of canola oil) had 11% lower sIL-6R concentrations than his twin with a low intake. Despite the robust association with sIL-6R, no significant associations were found with plasma IL-6, TNF-α, or high-sensitivity CRP [20•]. In a study of 511 Japanese employees of municipal offices, ALA intake was assessed by a diet history questionnaire that had been validated against 16-day weighed food records (Pearson correlation for ALA, r = 0.3) [21]. ALA comprised 0.8% to 1.0% energy (>2 g/d) and was inversely related to serum CRP. Data were adjusted for age, body mass index (BMI), lifestyle factors, and physical activity, but not for dietary factors associated with ALA, and should therefore be interpreted with caution.
Smith et al. [22•] assessed dietary ALA intake by the Willett questionnaire in 260 post-MI patients and linked these data to 24-hour electrocardiogram recordings that were analyzed for ventricular premature beats. ALA intake (expressed per 1,000 kcal/d) was associated with a significant reduction in ventricular premature beats after adjustment for age, sex, cardiovascular medication, and co-morbidities. However, lifestyle (eg, smoking) and dietary factors were not controlled for and the study had a cross-sectional design, which has inherent methodologic weaknesses.
Biomarker Studies of ALA and Cardiovascular Risk
Previous analyses in the National Heart, Lung, and Blood Institute NHLBI Family Heart Study suggested that ALA may protect against atherosclerosis [23, 24]. Recently, Sala-Vila et al. [25] investigated whether serum phosphatidylcholine content of ALA and other fatty acids was related to carotid atherosclerosis in a cross-sectional study of 451 asymptomatic Spanish individuals (mean age of 45 years) with primary dyslipidemia. Over half of the participants were treated with lipid-lowering drugs. The habitual Mediterranean diet in this population provided a mean ALA intake of 0.8 g/d, mainly from olive oil and walnuts, which correlated well with serum ALA (r = 0.44). EPA and DHA intake from fish was 1.05 g/d on average. The association of serum fatty acids with intima-media thickness (IMT) of the carotid arteries was assessed, adjusting for age, sex, BMI, smoking, antihypertensive drugs, statins, and other serum fatty acids. Significant inverse associations were found between serum ALA and internal carotid artery IMT, and between serum DHA and common carotid artery IMT. Serum EPA was not associated with IMT [25]. In a small cross-sectional study of 50 Asian men and women (mean age of 58 years) who suffered a first nonfatal MI, the mean common carotid IMT was inversely associated with ALA content of erythrocytes (P = 0.09) and ALA intake (P = 0.02) [26]. Data, however, were only adjusted for age, sex, and total energy (for dietary ALA). EPA and DHA were not consistently related to IMT. The average intake of ALA was 0.6 g/d, which was similar to that of EPA and DHA intake.
Ebbesson et al. [27] examined whether ALA content of erythrocytes was related to heart rate as a risk indicator for ventricular arrhythmias. They performed a cross-sectional study in 707 Alaskan Eskimos (mean age of 50 years) who had a habitual intake of marine n-3 fatty acids of 2.9 g/d. After adjustment for gender, height, BMI, blood pressure, smoking, and heart rate–lowering medications, no association was observed with ALA (P = 0.98). EPA and DHA, on the other hand, were significantly inversely associated with heart rate.
The delta(6)-desaturase enzyme is the rate-limiting step in the conversion of ALA into EPA and DHA, and genetic variation in the delta(6)-desaturase gene (FADS2) may therefore affect the associations of ALA with cardiovascular health. Truong et al. [28], in a cross-sectional study, examined the association of ALA in adipose tissue with metabolic syndrome, and possible effect modification by FADS2. In a cohort of 1,815 men and women from Costa Rica, the prevalence of metabolic syndrome (656 cases) was 19% lower in the upper compared with the lower quintile of adipose tissue ALA. There was no association between ALA and metabolic syndrome among homozygous carriers of the FADS2 deletion allele, suggesting that conversion of ALA into EPA may play a role [28]. It should be noted, however, that the FADS2 polymorphism did not influence the inverse association of ALA with nonfatal MI in a previous case–control study from Costa Rica [29].
Biomarker Studies of ALA and Cardiovascular Endpoints
ALA status has been inversely associated with cardiovascular disease events, although data are less consistent than for EPA and DHA [7–10]. An overview of ALA biomarker studies is provided in Table 2. In the aforementioned case–control study by Campos et al. [19••], ALA was measured in adipose tissue as a biomarker of intake, which correlated well with dietary ALA. ALA was strongly inversely associated with nonfatal MI, with a 57% reduced risk when comparing the 7th decile with the lowest decile. The relationship between ALA and MI was nonlinear and mainly confined to levels below the median (Fig. 1). Mozaffarian et al. [30] suggested that ALA may particularly reduce CHD risk when intake of marine n-3 fatty acids is low. In the study by Campos et al. [19••], however, concurrent fish intake (range, 3–32 g/d) or EPA and DHA intake (range, 130–520 mg/d) did not modify the associations of ALA with MI.
Table 2.
Overview of biomarker studies of alpha-linolenic acid and cardiovascular events published between January 2008 and June 2010
| Study/year | Population | Design | Outcome |
|---|---|---|---|
| Campos et al. [19••]/2008 | Costa Rica: 1,891 cases with first nonfatal MI and 1,891 population-based controls; matching for age, sex, and area of residence | Case–control study: association of ALA intake from FFQ and ALA in adipose tissue with risk of first nonfatal MI | OR (95% CI) for first nonfatal MI was 0.41 (0.25–0.67) for top vs lowest decile of ALA in adipose tissue, and 0.61 (0.42–0.88) for high vs low ALA intake; associations only present at lower ALA levels |
| Yamagishi et al. [31]/2008 | USA, Minneapolis: 3,575 white men and women from ARIC study, ages 45–64 y | Prospective cohort study: association of plasma ALA with incident heart failure; 14.3 y of follow-up | 195 participants (5.5%) developed heart failure; ALA status (top vs bottom quintile) was not associated with incident heart failure; age- and sex-adjusted HR was 0.99 (0.63–1.53) for cholesteryl ester fraction and 0.97 (0.61–1.54) for phospholipid fraction |
| Warensjö et al. [32]/2008 | Sweden: 2,009 men from ULSAM study, aged 50 y | Prospective cohort study: association of ALA in serum cholesteryl esters with CVD mortality; 30.7 y of follow-up | Multivariable-adjusted HR was 1.10 (1.00–1.21) per 1-SD increase in serum ALA |
| Park et al. [33]/2009 | South Korea: 40 cases of ischemic stroke, 40 cases of hemorrhagic stroke and 40 healthy controls; matching for age and sex | Case–control study: association of ALA in erythrocytes with risk of ischemic and hemorrhagic stroke | Erythrocyte ALA concentrations (area%) in hemorrhagic stroke patients (0.71 ± 0.21) and ischemic stroke patients (0.24 ± 0.03) were not significantly different from controls (0.44 ± 0.05) after adjustment for family history of stroke; inverse association of ALA with ischemic stroke after adjustment for age and systolic blood pressure (P = 0.045). |
| Virtanen et al. [34••]/2009 | Finland: 2,174 men from Kuopio Ischemic Heart Disease Risk Factor Study, ages 42–60 y | Prospective cohort study: association of serum ALA with incident atrial fibrillation; 17.7 y of follow-up | 240 men (11.0%) developed atrial fibrillation; multivariable-adjusted HR for serum ALA (compared to Q1) was Q2: 1.26 (95% CI, 0.84–1.89), Q3: 0.74 (0.46–1.20), and Q4: 1.14 (0.72–1.79; P for trend = 0.98). |
| Lemaitre et al. [35••]/2009 | USA, Seattle: 265 out-of-hospital sudden cardiac arrest patients and 415 community members; matching for age, sex, and calendar year | Case–control study: association of ALA in erythrocytes with risk of sudden cardiac death; blood collection immediately after the event (patients) or during interview (control) | Multivariable-adjusted OR over quartiles of ALA in erythrocytes (compared to Q1): Q2 was 1.7 (1.0–3.0), Q3 was 1.9 (1.1–3.3), Q4 was 2.5 (95% CI, 1.3–4.8); association independent of erythrocyte levels of EPA and DHA, linoleic acid, and trans fatty acids |
ALA alpha-linolenic acid; ARIC Atherosclerosis Risk in Communities; CVD cardiovascular diseases; DHA docosahexaenoic acid; EPA eicosapentaenoic acid; FFQ food frequency questionnaire; HR hazard ratio; MI myocardial infarction; OR odds ratio; Q quartile; SD standard deviation; ULSAM Uppsala Longitudinal Study of Adult Men
Yamagishi et al. [31] examined the prospective association of plasma fatty acids with risk of heart failure. The data used were from 3,575 white men and women in the United States (mean age of 54 years) who participated in the Atherosclerosis Risk in Communities (ARIC) study. During 14 years of follow-up, 195 cases of heart failure developed. Concentrations of n-3 fatty acids were assessed in plasma cholesteryl esters and in phospholipids. Plasma ALA was not associated with risk of heart failure (hazard ratios of 0.99 and 0.97 for upper versus lower quintiles of cholesteryl ester and phospholipid fractions, respectively; P = 0.8). Plasma EPA also showed no association. Plasma DHA was inversely associated with incident heart failure, but only in women. Data were extensively adjusted for major confounders, including age, sex, BMI, lifestyle factors, and cardiovascular risk factors, but not for potential dietary confounders [31].
Warensjö et al. [32] conducted a prospective cohort study of ALA in serum cholesteryl esters and cardiovascular mortality in more than 2,000 Swedish men (mean age of 50 years). The study had 30 years of follow-up and comprised over 60,000 person-years. A 10% higher risk of fatal cardiovascular events was found per standard deviation increase in serum ALA, which was borderline statistically significant. Data were adjusted for serum cholesterol, BMI, smoking, physical activity, and presence of hypertension.
Erythrocyte concentrations of n-3 fatty acids were studied in relation to hemorrhagic and ischemic stroke in a case–control study of 120 Asian men and women (mean age of 57 years) [33]. The average total n-3 fatty acid intake in this population was 1.1 g/d, about half of which was ALA. Erythrocyte ALA concentrations (area%) were 0.71 ± 0.21 in hemorrhagic stroke patients and 0.24 ± 0.03 in ischemic stroke patients, which did not differ significantly from controls (0.44 ± 0.05) after adjustment for family history of stroke. In a logistic regression model, both ALA, EPA and DHA were significantly inversely related to ischemic stroke. EPA and DHA were also inversely related to hemorrhagic stroke, but this was not the case for ALA. Data, however, were only adjusted for age and systolic blood pressure, so residual confounding may have been present.
The risk of atrial fibrillation in relation to serum n-3 fatty acids was examined in a prospective cohort study of 2,174 Finnish men (mean age of 53 years) [34••]. During 18 years of follow-up, 240 events of atrial fibrillation occurred. Serum ALA was not associated with incidence of atrial fibrillation. Hazard ratios in consecutive quartiles of ALA were 1.26 (95% CI, 0.84–1.89), 0.74 (95% CI, 0.46–1.20), and 1.14 (95% CI, 0.72–1.79) compared with the lowest quartile (P for trend = 0.98). Serum EPA did not show an association but DHA was inversely related to atrial fibrillation (hazard ratio of 0.62 for upper vs lower quartile; P for trend = 0.02) [34••].
Finally, Lemaitre et al. [35••] investigated in a case–control study whether ALA levels in erythrocytes were associated with risk of sudden cardiac death. Blood was collected from 265 out-of-hospital sudden cardiac arrest patients in Seattle, WA immediately after the event and from 415 randomly selected community members (mean age of 58 years). In contrast to what was expected, higher ALA levels were associated with a higher risk of sudden cardiac arrest. After adjustment for age, sex, smoking, diabetes, hypertension, education, physical activity, weight, height, and total fat intake, the risk increased over the quartiles with an odds ratio of 2.5 (95% CI, 1.3–4.8) for the highest compared with the lowest quartile. The association was independent of other fatty acids in erythrocyte membranes, including EPA and DHA [35••].
Conclusions
The trials reviewed here consistently showed an increase in blood ALA levels after ALA supplementation, starting at low doses (<2 g/d). ALA supplementation also increased blood levels of EPA, but not of DHA, indicating conversion of ALA to EPA through elongation and desaturation. Short-term trials (6–12 weeks) in generally healthy individuals mostly showed no or inconsistent effects of ALA intake (1.2–3.6 g/d) on blood lipids, LDL oxidation, lipoprotein(a), and apolipoproteins A-I and B. Previous studies suggested an anti-inflammatory action of ALA [5, 7, 8], but recent trials showed little effect of ALA on CRP or other inflammatory markers. There was, however, an interesting inverse association of ALA with sIL-6R in the twin study by Dai et al. [20•], which warrants further investigation. The few studies that addressed ALA intake in relation to glucose metabolism or blood pressure yielded inconsistent results [16, 17, 18••]. There is, however, some observational evidence that a high ALA status may be related to a lower risk of metabolic syndrome [28]. Long-term treatment with high ALA doses had a beneficial effect on body weight and blood LDL cholesterol [18••], which warrants confirmation in future trials.
Previous evidence favored recommendations for modest dietary consumption of ALA (2–3 g/d) for the primary and secondary prevention of CHD [7]. The recently published case–control study by Campos et al. [19••] showing strong inverse associations of ALA status and intake with nonfatal MI is in line with this recommendation. Recent data provide some support that ALA could protect against atherosclerosis [25, 26], but it should be noted that this evidence comes from relatively small cross-sectional studies and that conclusions on causality cannot be drawn. Concerning the hypothesis of an anti-arrhythmic effect of n-3 fatty acids, there was some evidence for protection against ventricular premature beats [22•], but no evidence for a relation with heart rate [27] or incidence of atrial fibrillation [34••]. Moreover, data from two recent well-conducted epidemiologic studies suggested that high tissue ALA is related to an increased rather than decreased risk of fatal cardiovascular events [32] and sudden death [35••]. Harris et al. [36] performed a meta-analysis of previous studies on tissue fatty acid composition and risk of CHD published until 2006. They showed that ALA in adipose tissue or phospholipids was inversely associated with CHD, although the association was not statistically significant for fatal events [36]. Of 16 studies reviewed, about half were supportive for a beneficial role of ALA, whereas other studies were negative or supportive for an adverse effect [36].
In conclusion, there is a need for long-term trials investigating the effect of ALA supplementation on cardiovascular risk factors and clinical end points. Data are awaited from the Alpha Omega Trial, in which 4,837 post-MI patients (mean age of 69 years) were randomized to 2 g/d of ALA and/or 400 mg/d of EPA and DHA and followed for fatal and nonfatal cardiovascular disease events for 40 months [37]. The findings of this study may answer the question of whether a food-based dose of ALA affects cardiovascular health in high-risk individuals and, if so, whether this is comparable to the effect of marine n-3 fatty acids.
Acknowledgments
Disclosure
Dr. Geleijnse’s institution received an unrestricted grants from the Dutch Product Board for Margarine Fats and Oils and from the Alpro Foundation for an epidemiologic study of fatty acid intake and cardiovascular diseases in the Dutch population. It also received an unrestricted grant from Unilever to conduct the Alpha Omega Trial (http://www.alphaomegatrial.com). No other potential conflicts of interest relevant to this article were reported.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Gebauer SK, Psota TL, Harris WS, Kris-Etherton PM. n-3 fatty acid dietary recommendations and food sources to achieve essentiality and cardiovascular benefits. Am J Clin Nutr. 2006;83(Suppl 6):1526S–1535S. doi: 10.1093/ajcn/83.6.1526S. [DOI] [PubMed] [Google Scholar]
- 2.Zatónski W, Campos H, Willett W. Rapid declines in coronary heart disease mortality in Eastern Europe are associated with increased consumption of oils rich in alpha-linolenic acid. Eur J Epidemiol. 2008;23:3–10. doi: 10.1007/s10654-007-9195-1. [DOI] [PubMed] [Google Scholar]
- 3.Hulshof KF, van Erp-Baart MA, Anttolainen M, et al. Intake of fatty acids in western Europe with emphasis on trans fatty acids: the TRANSFAIR Study. Eur J Clin Nutr. 1999;53:143–157. doi: 10.1038/sj.ejcn.1600692. [DOI] [PubMed] [Google Scholar]
- 4.IOM: Dietary reference intakes: energy, carbohydrates, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, DC: National Academies Press; 2002. [DOI] [PubMed]
- 5.Hansen SN, Harris WS. New evidence for the cardiovascular benefits of long chain omega-3 fatty acids. Curr Atheroscler Rep. 2007;9:434–440. doi: 10.1007/s11883-007-0058-8. [DOI] [PubMed] [Google Scholar]
- 6.Harris WS, Kris-Etherton PM, Harris KA. Intakes of long-chain omega-3 fatty acid associated with reduced risk for death from coronary heart disease in healthy adults. Curr Atheroscler Rep. 2008;10:503–509. doi: 10.1007/s11883-008-0078-z. [DOI] [PubMed] [Google Scholar]
- 7.Mozaffarian D. Does alpha-linolenic acid intake reduce the risk of coronary heart disease? A review of the evidence. Altern Ther Health Med. 2005;11:24–30. [PubMed] [Google Scholar]
- 8.Harris WS, Miller M, Tighe AP, et al. Omega-3 fatty acids and coronary heart disease risk: clinical and mechanistic perspectives. Atherosclerosis. 2008;197:12–24. doi: 10.1016/j.atherosclerosis.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 9.Harris WS. Cardiovascular risk and alpha-linolenic acid: can Costa Rica clarify? Circulation. 2008;118:323–324. doi: 10.1161/CIRCULATIONAHA.108.791467. [DOI] [PubMed] [Google Scholar]
- 10.Wang C, Harris WS, Chung M, et al. n-3 Fatty acids from fish or fish-oil supplements, but not alpha-linolenic acid, benefit cardiovascular disease outcomes in primary- and secondary-prevention studies: a systematic review. Am J Clin Nutr. 2006;84:5–17. doi: 10.1093/ajcn/84.1.5. [DOI] [PubMed] [Google Scholar]
- 11.Brouwer IA, Katan MB, Zock PL. Dietary alpha-linolenic acid is associated with reduced risk of fatal coronary heart disease, but increased prostate cancer risk: a meta-analysis. J Nutr. 2004;134:919–922. doi: 10.1093/jn/134.4.919. [DOI] [PubMed] [Google Scholar]
- 12.De Lorgeril M, Renaud S, Mamelle N, et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343:1454–1459. doi: 10.1016/S0140-6736(94)92580-1. [DOI] [PubMed] [Google Scholar]
- 13.Kaul N, Kreml R, Austria JA, et al. A comparison of fish oil, flaxseed oil and hempseed oil supplementation on selected parameters of cardiovascular health in healthy volunteers. J Am Coll Nutr. 2008;27:51–58. doi: 10.1080/07315724.2008.10719674. [DOI] [PubMed] [Google Scholar]
- 14.Egert S, Kannenberg F, Somoza V, et al. Dietary alpha-linolenic acid, EPA, and DHA have differential effects on LDL fatty acid composition but similar effects on serum lipid profiles in normolipidemic humans. J Nutr. 2009;139:861–868. doi: 10.3945/jn.108.103861. [DOI] [PubMed] [Google Scholar]
- 15.Barceló-Coblijn G, Murphy EJ, Othman R, et al. Flaxseed oil and fish-oil capsule consumption alters human red blood cell n-3 fatty acid composition: a multiple-dosing trial comparing 2 sources of n-3 fatty acid. Am J Clin Nutr. 2008;88:801–809. doi: 10.1093/ajcn/88.3.801. [DOI] [PubMed] [Google Scholar]
- 16.Sioen I, Hacquebard M, Hick G, et al. Effect of ALA-enriched food supply on cardiovascular risk factors in males. Lipids. 2009;44:603–611. doi: 10.1007/s11745-009-3307-5. [DOI] [PubMed] [Google Scholar]
- 17.Bloedon LT, Balikai S, Chittams J, et al. Flaxseed and cardiovascular risk factors: results from a double blind, randomized, controlled clinical trial. J Am Coll Nutr. 2008;27:65–74. doi: 10.1080/07315724.2008.10719676. [DOI] [PubMed] [Google Scholar]
- 18.Dodin S, Cunnane SC, Mâsse B, et al. Flaxseed on cardiovascular disease markers in healthy menopausal women: a randomized, double-blind, placebo-controlled trial. Nutrition. 2008;24:23–30. doi: 10.1016/j.nut.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Campos H, Baylin A, Willett WC. Alpha-linolenic acid and risk of nonfatal acute myocardial infarction. Circulation. 2008;118:339–345. doi: 10.1161/CIRCULATIONAHA.107.762419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dai J, Ziegler TR, Bostick RM, et al. High habitual dietary alpha-linolenic acid intake is associated with decreased plasma soluble interleukin-6 receptor concentrations in male twins. Am J Clin Nutr. 2010;92:177–185. doi: 10.3945/ajcn.2010.29305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poudel-Tandukar K, Nanri A, Matsushita Y, et al. Dietary intakes of alpha-linolenic and linoleic acids are inversely associated with serum C-reactive protein levels among Japanese men. Nutr Res. 2009;29:363–370. doi: 10.1016/j.nutres.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 22.Smith PJ, Blumenthal JA, Babyak MA, et al. Association between n-3 fatty acid consumption and ventricular ectopy after myocardial infarction. Am J Clin Nutr. 2009;89:1315–1320. doi: 10.3945/ajcn.2008.26829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Djoussé L, Arnett DK, Carr JJ, et al. Investigators of the NHLBI FHS: Dietary linolenic acid is inversely associated with calcified atherosclerotic plaque in the coronary arteries: the National Heart, Lung, and Blood Institute Family Heart Study. Circulation. 2005;111:2921–2926. doi: 10.1161/CIRCULATIONAHA.104.489534. [DOI] [PubMed] [Google Scholar]
- 24.Djoussé L, Folsom AR, Province MA, National Heart, Lung, and Blood Institute Family Heart Study et al. Dietary linolenic acid and carotid atherosclerosis: the National Heart, Lung, and Blood Institute Family Heart Study. Am J Clin Nutr. 2003;77:819–825. doi: 10.1093/ajcn/77.4.819. [DOI] [PubMed] [Google Scholar]
- 25.Sala-Vila A, Cofán M, Pérez-Heras A, et al. Fatty acids in serum phospholipids and carotid intima-media thickness in Spanish subjects with primary dyslipidemia. Am J Clin Nutr. 2010;92:186–193. doi: 10.3945/ajcn.2009.28807. [DOI] [PubMed] [Google Scholar]
- 26.Park Y, Lim J, Kwon Y, Lee J. Correlation of erythrocyte fatty acid composition and dietary intakes with markers of atherosclerosis in patients with myocardial infarction. Nutr Res. 2009;29:391–396. doi: 10.1016/j.nutres.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 27.Ebbesson SO, Devereux RB, Cole S, et al. Heart rate is associated with red blood cell fatty acid concentration: the Genetics of Coronary Artery Disease in Alaska Natives (GOCADAN) study. Am Heart J. 2010;159:1020–1025. doi: 10.1016/j.ahj.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Truong H, DiBello JR, Ruiz-Narvaez E, et al. Does genetic variation in the Delta6-desaturase promoter modify the association between alpha-linolenic acid and the prevalence of metabolic syndrome? Am J Clin Nutr. 2009;89:920–925. doi: 10.3945/ajcn.2008.27107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baylin A, Ruiz-Narvaez E, Kraft P, Campos H. alpha-Linolenic acid, Delta6-desaturase gene polymorphism, and the risk of nonfatal myocardial infarction. Am J Clin Nutr. 2007;85:554–560. doi: 10.1093/ajcn/85.2.554. [DOI] [PubMed] [Google Scholar]
- 30.Mozaffarian D, Ascherio A, Hu FB, et al. Interplay between different polyunsaturated fatty acids and risk of coronary heart disease in men. Circulation. 2005;111:157–164. doi: 10.1161/01.CIR.0000152099.87287.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yamagishi K, Nettleton JA, Folsom AR, ARIC Study Investigators Plasma fatty acid composition and incident heart failure in middle-aged adults: the Atherosclerosis Risk in Communities (ARIC) Study. Am Heart J. 2008;156:965–974. doi: 10.1016/j.ahj.2008.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Warensjö E, Sundström J, Vessby B, et al. Markers of dietary fat quality and fatty acid desaturation as predictors of total and cardiovascular mortality: a population-based prospective study. Am J Clin Nutr. 2008;88:203–209. doi: 10.1093/ajcn/88.1.203. [DOI] [PubMed] [Google Scholar]
- 33.Park Y, Park S, Yi H, et al. Low level of n-3 polyunsaturated fatty acids in erythrocytes is a risk factor for both acute ischemic and hemorrhagic stroke in Koreans. Nutr Res. 2009;29:825–830. doi: 10.1016/j.nutres.2009.10.018. [DOI] [PubMed] [Google Scholar]
- 34.Virtanen JK, Mursu J, Voutilainen S, Tuomainen TP. Serum long-chain n-3 polyunsaturated fatty acids and risk of hospital diagnosis of atrial fibrillation in men. Circulation. 2009;120:2315–2321. doi: 10.1161/CIRCULATIONAHA.109.852657. [DOI] [PubMed] [Google Scholar]
- 35.Lemaitre RN, King IB, Sotoodehnia N, et al. Red blood cell membrane alpha-linolenic acid and the risk of sudden cardiac arrest. Metabolism. 2009;58:534–540. doi: 10.1016/j.metabol.2008.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harris WS, Poston WC, Haddock CK. Tissue n-3 and n-6 fatty acids and risk for coronary heart disease events. Atherosclerosis. 2007;193:1–10. doi: 10.1016/j.atherosclerosis.2007.03.018. [DOI] [PubMed] [Google Scholar]
- 37.Geleijnse JM, Giltay EJ, Schouten EG, Alpha Omega Trial Group et al. Effect of low doses of n-3 fatty acids on cardiovascular diseases in 4,837 post-myocardial infarction patients: design and baseline characteristics of the Alpha Omega Trial. Am Heart J. 2010;159:539–546.e2. doi: 10.1016/j.ahj.2009.12.033. [DOI] [PubMed] [Google Scholar]


