Abstract
Over the past few years, arthroscopy of the hip joint is becoming more common as a technique in both the diagnosis and treatment of hip pain. A frequent cause of hip and groin pain is a tear of the acetabular labrum. Patients with labral tears complain of pain in the groin region and pain with clicking in the hip without a history of pain prior to the original onset. Once a patient presents with signs and symptoms of hip pain that are greater than four weeks in conjunction with indicative findings of a labral tear by way of MRI, he or she may be considered a good candidate for arthroscopy of the hip joint. Little evidence exists in the current literature on rehabilitative procedures performed after arthroscopy of the acetabular labrum. The purpose of this clinical commentary is to suggest a rehabilitation protocol after acetebular labral debridement or repair.
INTRODUCTION
Arthroscopy of the hip joint has become a common technique used over the past few years in both the diagnosis and treatment of hip pain.1–7 One of the more frequent diagnoses of hip and groin pain is a tear of the acetabular labrum. The most common etiology in patients with mechanical hip symptoms is the existence of a labral tear8, 9 and can be related to intra-articular snapping hip syndrome up to 80% of the time.7 In 59 patients undergoing hip arthroscopy, 59% had a tear of the acetabular labrum.8 Likewise, a significant correlation exists between the tear and complaints of clicking and giving-way. In an athletic population, among eighteen patients presenting with a complaint of pain in the groin region, four (22%) were found to have a tear in the acetabular labrum.10 All of the patients with a tear reported pain with clicking in the hip, but did not have a history of pain prior to the original onset. In addition, of 45 professional athletes who presented with femoroacetabular impingement, all had a tear in the labrum.4 The presence of hip labral tears is also high in the general population. Of 100 patients (39±13 years of age) who presented with mechanical symptoms of pain, clicking, and locking in the hip, 66% were found to have labral tears.9
The mechanism of injury (MOI) for an acetabular labral tear often involves repetitive twisting, cutting, and pivoting movements in addition to repetitive flexion at the hip.11 However, the history of the mechanism associated with injury is not always apparent to the patient. Instead, patients will present with insidious complaints of groin pain and mechanical symptoms of clicking, locking, and giving way.9–12 Additional causes of acetabular labral tears may include femoral acetabular impingement, capsular laxity/joint hypermobility, hip dysplasia, and joint degeneration.1 The mechanism of femoral acetabular impingement occurs when the anterior superior portion of the labrum is pinched or squeezed by the edge of the acetabulum and the anterior neck of the femur.1,6 This type of mechanism is described as either cam or pincer.13 In cam, an abnormal femoral head is wedged against the acetabulum in motions such as forced or excessive flexion. On the other hand, pincer femoral acetabular impingement is the result of an irregular projection of the acetabular rim that contacts the head of the femur during movement.13
Upon examination, the clinical characteristics of a tear in the acetabular labrum can vary. In 66 patients with a labral tear (confirmed arthroscopically) who were retrospectively examined, 61% had an insidious onset of symptoms while, 86% reported the symptoms as moderate to severe. Similarly, the most common location was in the groin, with either sharp or dull pain which was activity-related and included painful mechanical locking.11
DIAGNOSIS
Because pain in the hip can arise from a variety of different sources, identification of a labral tear can be challenging and is often misdiagnosed. Using plain radiography is not always sufficient for identifying a labral tear. However, structural abnormalities of the hip such as a retroverted acetabulum or coxa valga have been found in a high percentage (87%) of those patients with labral tears.14 As these abnormalities are more closely scrutinized, earlier detection of a tear may be possible.
Acetabular labral tears are most reliably diagnosed arthroscopically. However, with the development of musculoskeletal imaging, correctly diagnosing a tear has become more manageable. Magnetic resonance imaging (MRI)15 and arthrography (MRA) are regularly used to evaluate and diagnose hip labral pathology.9,16,17 The MRI has been shown to accurately assess the presence of both hip labral and articular cartilage damage.15 Using MRI, labral pathologies were identified correctly in 94% and 95% of the cases respectively by two radiologists. Likewise, a high agreement exists between MRI and arthroscopy in the identification of chondral pathology. MRA can provide an extension of MRI by allowing an in vivo image of the hip joint that can often be difficult to see secondary to the depth of the articulation.9 In fact, a significant correlation between the grade of cartilage loss with the grade of labral tear has been shown, causing the authors to suggest an MRA may be indicated if the presence of bone marrow edema is discovered with a routine MRI.
SURGICAL INTERVENTION
Once a patient presents with signs and symptoms of hip pain that are greater than four weeks in conjunction with indicative findings of a labral tear by way of MRI or MRA, he or she may be considered a good candidate for arthroscopy of the hip joint.14 Arthroscopic techniques for treating hip labral pathologies are becoming more routine in both adults,1, 7, 29, 30 adolescents, and children.20 In the case of an acetabular labral lesion, surgical intervention may involve debridement or repair. Be aware, however, conditions such as acetabular dysplasia, femoral acetabular impingement, degenerative conditions of the joint, fractures, arthrofibrosis, or non-compliance with the rehabilitation program may preclude the surgical intervention.
Both debridement and repair of an acetabular labral lesion may be performed in either the supine or lateral position. In the supine position, a standard fracture table is used with an oversized perineal post to apply traction. The affected hip is placed into slight extension and adduction to allow approach to the joint. Care is taken to minimize pressure in the perineal area as well as to carefully monitor the amount and duration of traction to avoid neurologic complications. The procedure is performed under the guidance of fluoroscopy. After an adequate amount of distraction is obtained, a 14 or 16 gauge spinal needle is inserted into the joint to break the vacuum seal and allow further distraction. Three portals are generally used, the anterolateral (which is established first), the anterior, and the distal lateral accessory or paratrochanteric portal.
After complete evaluation of the joint, including the articular cartilage surfaces of the acetabulum and femoral head, ligament fraying or tearing, and assessment of the posterior recess, any labral abnormality may then be addressed. Most labral tears occur in the anterior superior quadrant of the acetabulum. Acute, longitudinal, and peripheral tears are most amenable to repair. For repair of a detached labrum, the edges of the tear are delineated and suture anchors are placed on the top of the acetabular rim in the area of detachment.1 Conversely, if the tear in the labrum has a secure outer rim and is still attached to the acetabulum, a suture in the midsubstance of the tear can be used to secure the tissue. Radial splits, significantly macerated or degenerative labral tissue, or labral tissue that appears unviable should be debrided. Not uncommonly, chondral lesions may be noted adjacent to labral pathology that may require either debridement, common microfracture, or other cartilage resurfacing techniques.4,21
The natural history of untreated labral tears is unknown. Recently, authors9,21,22 have attempted to correlate the presence of labral tears with the development of degenerative osteoarthritis of the hip joint. Although this correlation remains unclear, some observations suggest labral lesions may be a contributory factor to the evolution and progression of osteoarthritis.21 Although debridement may be successful from the standpoint of pain relief, the surgery could potentially lead to joint load alteration and the progression of articular cartilage changes.23 In addition, alterations to the structure of the labrum, or disruption in the acetabular labral junction, may lead to the loss of the pressurized fluid film layer within the joint and uneven force distribution across the articular cartilage surfaces of the acetabulum and femoral head.24
REHABILITATION
Little evidence exists in the current literature to support rehabilitative procedures performed after arthroscopy of the acetabular labrum. Likewise, because new surgical procedures are constantly evolving, it is the responsibility of the physical therapist to stay up to date with the most current techniques as well as to establish and maintain good communication with the orthopaedic surgeon.
Surgical techniques and outcomes have been reported in the literature with little or no attention to post-operative rehabilitation.25–27 Currently, the best evidence for post-operative rehabilitation is based upon surgeon and physical therapist experience. With a labral repair, the location and size of the tear should be noted.28 Most of these tears are located in the anterior or anterosuperior portion of the labrum;9,29 movements that stress this area should be avoided. However, communication with the surgeon about the location of the tear and surgical technique used is vital to the treating physical therapist.
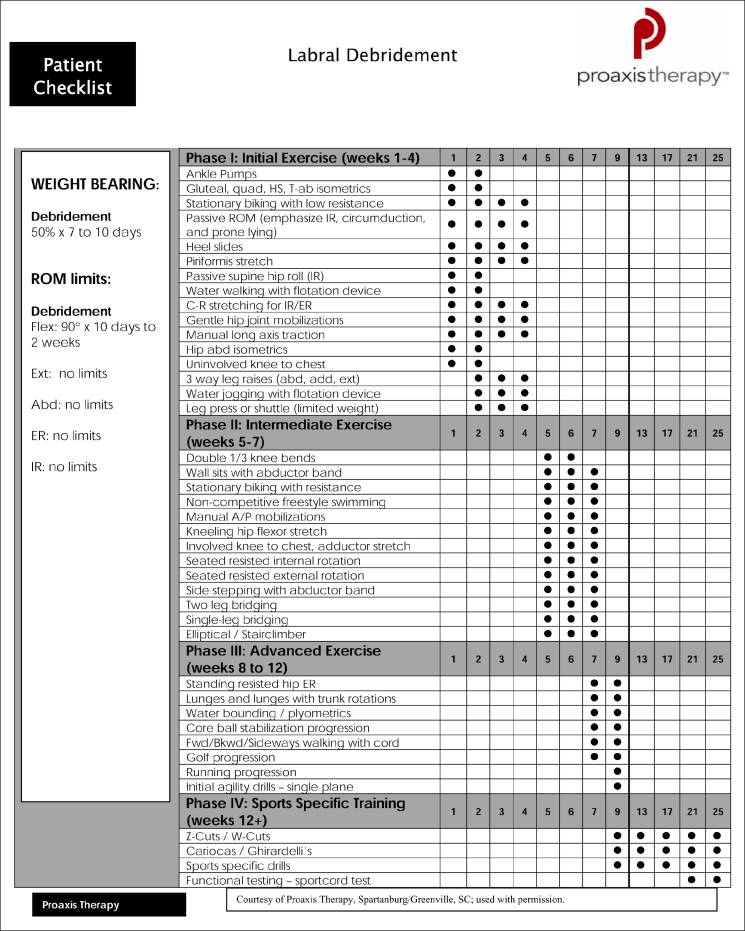
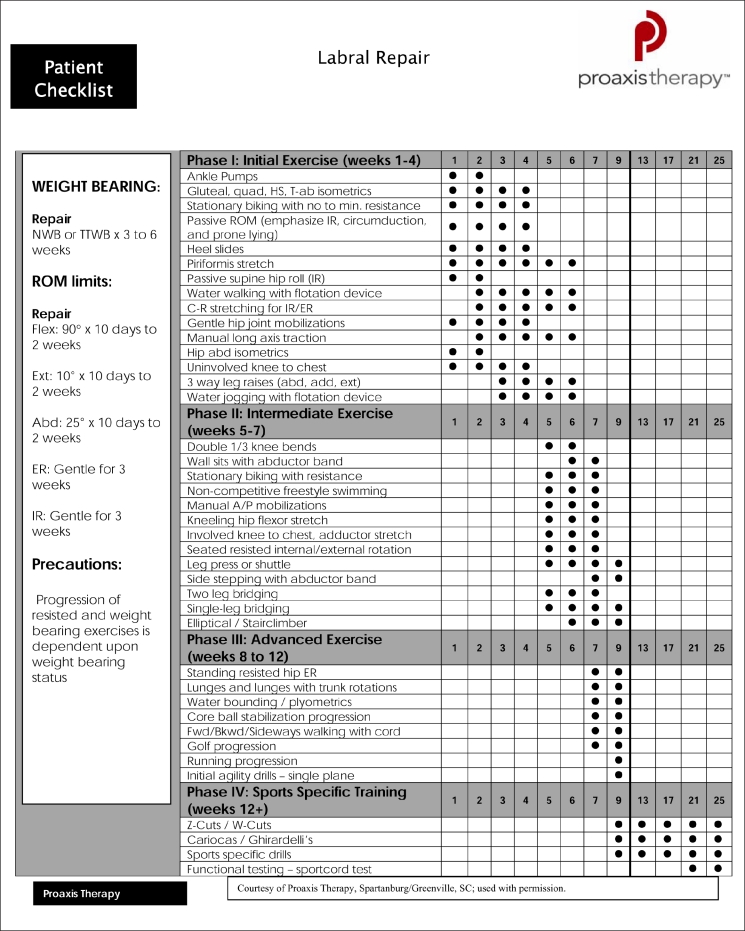
Rehabilitation protocols following acetabular labral debridement (Table 1) or repair (Table 2) can be divided into four phases. The progression with both procedures is similar with the exception of differences which are noted within the protocol. Exercise, and particularly strengthening, progression in a repair of the labrum may be delayed by a few weeks depending upon tissue healing. The timelines for each phase are based on clinical findings and presentations of active, healthy individuals. If clinical presentation meets objective criteria an athlete may move through the phases at a faster rate, always keeping basic tissue healing physiology in mind.
Table 1:
Table 2:
Phase I - Initial Exercises. Weeks 1 to 4.
The primary goals immediately following acetabular labral debridement or repair are to minimize pain and inflammation, protect the surgically repaired tissue, and initiate early motion exercises. Patients are typically 50% weight-bearing for 7 to 10 days progressing to weight-bearing as tolerated. For a labral repair, the weight-bearing restrictions include toe-touch weight bearing for 3 weeks, but may last up to 6 weeks depending upon the progression of healing and pain level of the patient. If the surgery involved additional procedures to the hip such as a microfracture, the weight-bearing restrictions can increase to 6 weeks. However, for purposes of this paper, labral debridement and repair will be the main focus.
It is important to maintain a symmetrical gait pattern to prevent concomitant stress throughout the lower extremity and spine. If this gait pattern is not established, a muscular imbalance of tight hip flexors and erector spinae with inhibition of the gluteals and abdominals (lower crossed syndrome) could develop.30 The potential ramifications include increased weight-bearing through the acetabulum with labral tissue stresses secondary to hip flexor tightness.31 Consequently, continued crutch use may be a necessary prophylactic. Similarly, the patient should be instructed to control the hip in all three planes of motion. Decreased core and hip strength have been implicated in alterations of lower extremity alignment during functional activities.32–34 Also, hip abductor strength has been shown to be a predictor of frontal plane motion in the knee while weak hip extensors can lead to quadriceps overuse and increased compression and shear force at the knee.32 A correlation between weakness in the hip and core and lower extremity injuries has been established.35 Thus, when these studies32,34–36 are considered together, the suggestion is that rehabilitation of the hip should include a component of hip and core strengthening in each phase.
Aquatic therapy is an excellent resource, if available, once surgical incisions are well-healed. Ambulation in the water allows for improvements in gait by allowing appropriate loads to the joint while minimizing unnecessary stresses to the healing tissue.19,28 Light jogging in the water using a flotation device may begin as early as 2-3 weeks if pain is not an issue. Range of motion (ROM) precautions may vary, but typically include limiting flexion beyond 90° for 10 days to avoid undue compression of the anterior labrum. If treating a labral repair, in addition to the 90° of flexion, the patient is limited to 25° of abduction and 10° of extension for 10 days to 2 weeks. An emphasis should be placed on manual therapy for pain reduction and improvements in joint mobility and proprioception.31 Considerations include gentle hip joint mobilizations, contract-relax stretching for internal and external rotation, long axis distraction, and assessment of lumbo-sacral mobility. Particular attention should be paid to the posterlateral soft tissue structures and the lumbo-sacral spine (as each can contribute to pain) and unnecessary hypomobility which will limit progress in future phases.
Modalities for pain control such as immediate post-operative transcutaneous electrical nerve stimulation (TENS) units {preferably applied in recovery room (based on clinical experiences of the authors)}, cryotherapy, and appropriate pain management through medication are important as well. Cautious and gentle stretching of hip muscle groups including piriformis, psoas, quadriceps, and hamstring muscles should begin with hip passive range of motion exercises, respecting the patient's pain threshold. The risk of tissue damage must be considered,37 and the patient should provide verbal feedback following mobilization and ROM exercises. Prone lying for 1 to 2 hours per day and passive ROM exercises emphasizing internal rotation are beneficial to prevent adhesions.19 Stationary bike begins with no resistance and gradually progresses in resistance over the first 4 weeks with a seat height that limits hip flexion to less than 90°.
Strengthening in Phase I initially consists of isometric contractions for the hip adductors, abductors, extensors, and transverse abdominals, but progresses to straight leg raises for abduction, adduction, and extension. To prevent irritation of the psoas muscle,19 hip flexion straight leg raise is not performed early on. Seated hip flexion using a short lever arm might be an alternative. For labral debridement, closed-chain activities of low-level leg press or shuttle can also begin with limited resistance. This type of exercise allows weight-bearing through the lower extremity joints with the application of appropriate stresses to the tissue.38
Criteria to progress from Phase I to Phase II require ROM of greater than or equal to 75% of the uninvolved side28 and the ability to demonstrate a sidelying straight leg raise (Figure 1) using the gluteus medius muscle. This straight let raise should be performed without compensation from the tensor fascia lata and quadratus lumborum.
Figure 1:
Sidelying straight leg raise.
Phase II - Intermediate Exercises. Weeks 5-7.
The primary focus of the second phase is to continue progressing ROM and soft tissue flexibility while beginning to transition the emphasis to strengthening. Manual therapy should continue with mobilization becoming more aggressive, as appropriate. If capsular laxity was thought to be a contributing factor to developing labral pathology, normal mobility (but not hypermobility) should be achieved. Flexibility exercises involving the piriformis, adductor group, and psoas/rectus femoris should continue. The kneeling hip flexor stretch (Figure 2) can be particularly beneficial for psoas and rectus femoris once tolerated in this phase of rehabilitation. Passive ROM exercises should become more aggressive, as needed, for internal and external rotation.
Figure 2:
Kneeling hip flexor stretch.
Strengthening of the hip and core musculature progresses ensuring the patient can dissociate pelvic movements and avoid muscular compensations. The strength goal is to build an endurance base prior to progressing to more advanced exercises. Patients can begin to add gradual resistance to the bike and use the elliptical machine, as tolerated, for cardiovascular endurance. Other examples of Phase II exercises include seated resisted internal (Figure 3) and external rotation, 1/3 knee bends progressing to wall sits with an abductor band for resistance (Figure 4), sidestepping with an abductor band for resistance, and core strengthening such as bridging on two legs progressing to single-leg bridging (Figure 5). Patients can return to non-competitive free-style swimming at week 5, as symptoms allow. Criteria to progress to Phase III are a normal gait pattern with no Trendelenburg sign. In addition, the patient should have symmetrical and passive ROM measurements with minimal complaints of pain.
Figure 3:

Resisted internal rotation - sitting.
Figure 4:

Wall squats with abductor band for resistance.
Figure 5:
Single leg bridging.
Phase III - Advanced Exercises. Weeks 8-12.
The primary objectives for Phase III are for the patient to have symmetrical ROM and begin integrated functional strengthening. Manual therapy should be performed as needed. Flexibility and passive ROM interventions should become slightly more aggressive if limitations persist. If full ROM or flexibility has not been attained at week 10, terminal stretches should be initiated, and moderate pain with stretching becomes acceptable.
Strengthening exercises should now incorporate multi-planar movements involving multiple muscles groups. Single leg activities challenging proprioception and strengthening of the hip muscles in a functional position should be performed. Examples of Phase III exercises include standing resisted hip external rotation (Figure 6), walking lunges, lunges with trunk rotation, plyometric bounding in the water, resisted sportcord walking forward/backward/sideways, and a progressive exercise ball program for advanced core strengthening. Core strengthening is an essential component to successful rehabilitation of athletes with hip pathology. As the progression to running and agility drills nears in the latter stages of the phase, athletes should be repetitively instructed on the importance of shock absorption and eccentric control during functional training.
Figure 6:

Resisted hip external rotation - standing.
Criteria to progress to Phase IV are symmetrical ROM and symmetrical flexibility of the psoas and piriformis. No noted Trendelenburg sign should exist with these higher level functional strengthening activities.
Phase IV - Return to Sports. Weeks 12+.
The primary objective of this phase is a safe and effective return to competition or previous activity level. Manual therapy, flexibility, and ROM exercises can be continued as deemed appropriate by the treating physical therapist. Careful attention and frequent re-assessment of these areas should take place to prevent loss of mobility and flexibility as the activity level increases. Once patients can demonstrate good muscular endurance, good eccentric control, and the ability to generate power, running may be progressed. Straight-ahead activities can be gradually progressed to lateral agilities. The completion of a return-to-play assessment using a sportcord test (developed by Steadman Hawkins Clinic and Howard Head Sports Medicine) prior to granted clearance for athletic competition. The athlete must perform a series of dynamic functional activities with resistance from a sportcord such as single-leg squats for 3 minutes, lateral bounding for 80 seconds, and forward/backward jogging for 2 minutes each. He or she is graded on the ability to demonstrate good neuromuscular control of the lower extremity during multi-planar movements that simulate athletic activities.
Post-operative protocols following acetabular labral debridement and repair will continue to develop as these procedures become more common. Current protocols are based on basic science and clinical experience, while future studies should include objective outcome measures to determine the most appropriate post-operative progression.
REFERENCES
- 1.Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: Surgical technique and review of the literature. Arthroscopy. 2005;21:1496–1504 [DOI] [PubMed] [Google Scholar]
- 2.McCarthy J, Noble P, Aluisio FV, et al. Anatomy, pathologic features, and treatment of acetabular labral tears. Clin Orthop Relat Res. 2003;406:38–47 [DOI] [PubMed] [Google Scholar]
- 3.Murphy KP, Ross AE, Javernick MA, Lehman RA., Jr Repair of the adult acetabular labrum. Arthroscopy. 2006;22:561–563 [DOI] [PubMed] [Google Scholar]
- 4.Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: Associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15:908–914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Philippon MJ, Arnoczky SP, Torrie A. Arthroscopic repair of the acetabular labrum: A histologic assessment of healing in an ovine model. Arthroscopy. 2007;23:376–380 [DOI] [PubMed] [Google Scholar]
- 6.Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25:299–308 [DOI] [PubMed] [Google Scholar]
- 7.Yamamoto Y, Hamada Y, Ide T, Usui I. Arthroscopic surgery to treat intra-articular type snapping hip. Arthroscopy. 2005;21:1120–1125 [DOI] [PubMed] [Google Scholar]
- 8.McCarthy JC, Busconi B. The role of hip arthroscopy in the diagnosis and treatment of hip disease. Can J Surg. 1995;38Suppl 1:S13–17 [PubMed] [Google Scholar]
- 9.Neumann G, Mendicuti AD, Zou KH, et al. Prevalence of labral tears and cartilage loss in patients with mechanical symptoms of the hip: Evaluation using MR arthrography. Osteoarthritis Cartilage. 2007;15:909–917 [DOI] [PubMed] [Google Scholar]
- 10.Narvani AA, Tsiridis E, Kendall S, et al. A preliminary report on prevalence of acetabular labrum tears in sports patients with groin pain. Knee Surg Sports Traumatol Arthrosc. 2003;11:403–408 [DOI] [PubMed] [Google Scholar]
- 11.Burnett RS, Della Rocca GJ, Prather H, et al. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88:1448–1457 [DOI] [PubMed] [Google Scholar]
- 12.Guevara CJ, Pietrobon R, Carothers JT, et al. Comprehensive morphologic evaluation of the hip in patients with symptomatic labral tear. Clin Orthop Relat Res. 2006;453:277–285 [DOI] [PubMed] [Google Scholar]
- 13.Lavigne M, Parvizi J, Beck M, et al. Anterior femoroacetabular impingement: Part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004:61–66 [PubMed] [Google Scholar]
- 14.Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426:145–150 [DOI] [PubMed] [Google Scholar]
- 15.Mintz DN, Hooper T, Connell D, et al. Magnetic resonance imaging of the hip: Detection of labral and chondral abnormalities using noncontrast imaging. Arthroscopy. 2005;21:385–393 [DOI] [PubMed] [Google Scholar]
- 16.Blankenbaker DG, De Smet AA, Keene JS, Fine JP. Classification and localization of acetabular labral tears. Skeletal Radiol. May2007;36:391–397 [DOI] [PubMed] [Google Scholar]
- 17.Petersilge CA, Haque MA, Petersilge WJ, et al. Acetabular labral tears: Evaluation with MR arthrography. Radiology. 1996;200:231–235 [DOI] [PubMed] [Google Scholar]
- 18.Atlihan D, Jones DC, Guanche CA. Arthroscopic treatment of a symptomatic hip plica. Clin Orthop Relat Res. 2003:174–177 [DOI] [PubMed] [Google Scholar]
- 19.Enseki KR, Martin RL, Draovitch P, et al. The hip joint: Arthroscopic procedures and postoperative rehabilitation. J Orthop Sports Phys Ther. 2006;36:516–525 [DOI] [PubMed] [Google Scholar]
- 20.Kocher MS, Kim YJ, Millis MB, et al. Hip arthroscopy in children and adolescents. J Pediatr Orthop. 2005;25:680–686 [DOI] [PubMed] [Google Scholar]
- 21.McCarthy JC, Noble PC, Schuck MR, et al. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25–37 [DOI] [PubMed] [Google Scholar]
- 22.Girard J, Springer K, Bocquet D, et al. Influence of labral tears on the outcome of acetabular augmentation procedures in adult dysplastic hips. Prospective assessment with a minimum follow-up of 12 years. Acta Orthop Belg. 2007;73:38–43 [PubMed] [Google Scholar]
- 23.Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171–178 [DOI] [PubMed] [Google Scholar]
- 24.Ferguson SJ, Bryant JT, Ganz R, Ito K. The acetabular labrum seal: A poroelastic finite element model. Clin Biomech. 2000;15:463–468 [DOI] [PubMed] [Google Scholar]
- 25.Diulus CA, Krebs VE, Hanna G, Barsoum WK. Hip arthroscopy technique and indications. J Arthroplasty. 2006;21(4 Suppl 1):68–73 [DOI] [PubMed] [Google Scholar]
- 26.Farjo L, Glick J. Hip arthroscopy for acetabular labral tears. Arthroscopy. 1999;15:132–137 [DOI] [PubMed] [Google Scholar]
- 27.Robertson W, Kadrmas W, Kely B. Arthroscopic management of labral tears in the hip: A systematic review. Clin Orthop Relat Res. 2006;455:88–92 [DOI] [PubMed] [Google Scholar]
- 28.Stalzer S, Wahoff M, Scanlan M. Rehabilitation following hip arthroscopy. Clin Sports Med. 2006;25:337–357 [DOI] [PubMed] [Google Scholar]
- 29.Peelle MW, Della Rocca GJ, Maloney WJ, et al. Acetabular and femoral radiographic abnormalities associated with labral tears. Clin Orthop Relat Res. 2005;441:327–333 [DOI] [PubMed] [Google Scholar]
- 30.Janda V. Evaluation of Muscular Imbalance: Rehabilitation of the Spine. Baltimore: Lippincott Williams & Wilkins; 1996:97–112 [Google Scholar]
- 31.Schmerl M, Pollard H, Hoskins W. Labral injuries of the hip: A review of diagnosis and management. J Manipulative Physiol Ther. 2005;28:632. [DOI] [PubMed] [Google Scholar]
- 32.Claiborne TL, Armstrong CW, Gandhi V, Pincivero DM. Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech. 2006;22:41–50 [DOI] [PubMed] [Google Scholar]
- 33.Mascal CL, Landel R, Powers C. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: Two case reports. J Orthop Sports Phys Ther. 2003;33:647–660 [DOI] [PubMed] [Google Scholar]
- 34.Willson JD, Ireland ML, Davis I. Core strength and lower extremity alignment during single leg squats. Med Sci Sports Exerc. 2006;38:945–952 [DOI] [PubMed] [Google Scholar]
- 35.Leetun DT, Ireland ML, Willson JD, et al. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36:926–934 [DOI] [PubMed] [Google Scholar]
- 36.Willson JD, Dougherty CP, Ireland ML, Davis IM. Core stability and its relationship to lower extremity function and injury. J Am Acad Orthop Surg. 2005;13:316–325 [DOI] [PubMed] [Google Scholar]
- 37.Cantu R. Soft tissue healing considerations after surgery. In: Maxey LM, ed. Rehabilitation for the Postsurgical Orthopedic Patient. St. Louis, MO: Mosby; 2001 [Google Scholar]
- 38.Snyder-Mackler L. Scientific rationale and physiological basis for the use of closed kinetic chain exercise in the lower extremity. J Sport Rehab. 1996;5:2–12 [Google Scholar]