Abstract
Stress-induced cardiomyopathy (SCMP) is diagnosed in 1-2% of patients presenting with symptoms suggestive of acute coronary syndrome. Because of sharing many common clinical features with SCMP, acute ST-segment elevation myocardial infarction (STEMI) can be misdiagnosed as SCMP. However, it can be associated with fatal outcome of the patient. Also, diagnosis of SCMP seems to be always challenging to clinicians, especially in the decision of taking coronary angiography which is still invasive and even risky. Here, we present a case with acute STEMI mimicking SCMP as a result of anatomical variation of coronary circulation. In this patient, prompt and early coronary angiography and stent implantation was very helpful.
Keywords: Stress-induced cardiomyopathy, Acute ST-segment elevation myocardial infarction, Coronary angiography
Introduction
Stress-induced cardiomyopathy (SCMP), also known as Tako-tsubo cardiomyopathy, was first described by Dote et al.1) in 1991. Initially, it is known as a clinical syndrome characterized by chest pain following emotional or physical stress, a typical ST-segment elevation on electrocardiography (ECG), mild increase in cardiac enzymes, and reversible left ventricular dysfunction with characteristic apical ballooning in patients without significant epicardial coronary artery stenosis.2),3) Recently, there are several variation of SCMP involving mid portion, basal portion or both portions of the left ventricle (basal ballooning syndrome).4)
Because SCMP shows similar clinical presentation with acute ST-segment elevation myocardial infarction (STEMI), SCMP can be misdiagnosed as an acute STEMI. However, it can be fatal if with misdiagnosis of acute STEMI as an SCMP. Here, we report a case with acute STEMI with typical echocardiographic feature of SCMP as a result of anatomical variation of the left anterior descending coronary artery (LAD). In this patient, early coronary angiography was very necessary.
Case
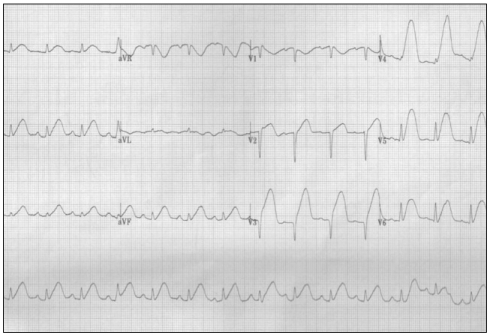
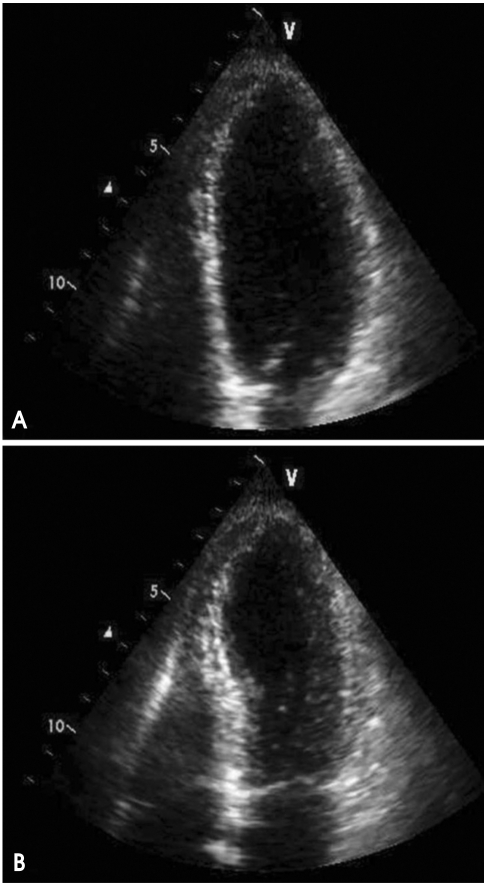
A 66-year-old woman visited our emergency department with new onset chest pain more than half an hour. Being worried that her grandson got wet as a result of sudden shower, she ran to the elementary school with an umbrella to pick him up as fast as possible. Suddenly, the patient felt chest pain after running and visited our hospital. In her past medical history, she has been on antihypertensive medication with a calcium channel blocker for 5 years. On her arrival, blood pressure was 108/56 mmHg, pulse rate and respiratory rate were 85 and 35 per minute, respectively. The initial ECG taken at the emergency department showed ST-segment elevation in all leads (Fig. 1) and the echocardiogram revealed akinesia of apical portion of the left ventricle with typical feature of apical ballooning (Fig. 2). After these two diagnostic studies, she was initially impressed of having SCMP. The cardiac enzyme levels were moderately elevated [creatinine kinase (CK) level of 677 U/L, CK-MB of 7.4 ng/mL, and troponin-I of 1.18 ng/mL] and these laboratory findings also supported the diagnosis of SCMP. Other chemistries were as follows; AST/ALT 19/15 IU/L, BUN/Cr 10.2/0.8 mg/dL, and N-terminal pro B-type natriuretic peptide 33.61 pg/mL.
Fig. 1.
The initial electrocardiogram shows ST-segment elevation in nearly all leads.
Fig. 2.
The echocardiography taken at admission reveals dilated left ventricular apex compatible with typical apical ballooning syndrome (A: end-diastole, and B: end-systole).
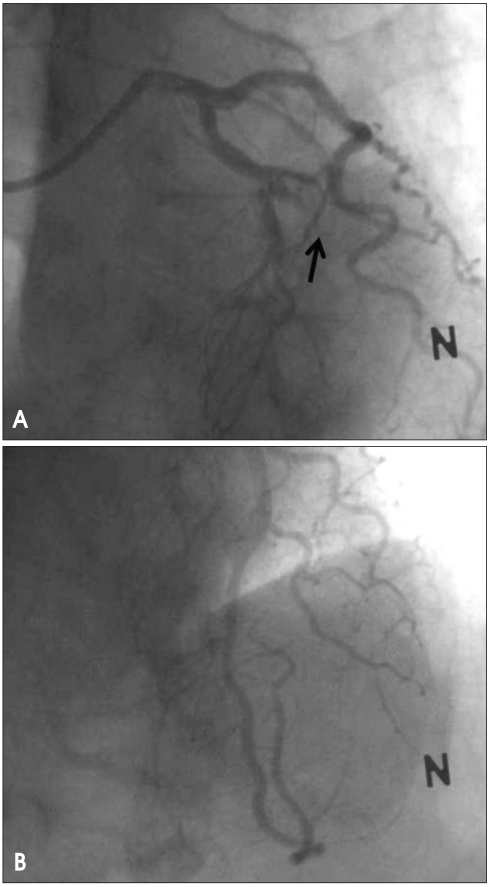
However, the patient complained of severe chest pain, which is unusual for patients with SCMP. And the intensity of her chest pain increased even after intravenous injection of morphine, the attending physician decided to check emergent coronary angiography. The left coronary angiogram showed totally occluded mid portion of the LAD (Fig. 3A). After successful reperfusion therapy of the occluded portion with a 3.0×28 mm sized Endeavor® stent (Medtronics Cardio Vascular, Santa Rosa, CA, USA), her LAD runs long way to the mid portion of posterior cardiac wall, and the septal and diagonal branches of the LAD supplied almost all apical portion of the heart (Fig. 3B). The patient was discharged without any complication 3 days after the primary angioplasty.
Fig. 3.
The initial left coronary angiogram demonstrates totally occluded mid portion of the left anterior descending coronary artery (arrow) (A). After successful reperfusion therapy, her left anterior descending coronary artery runs along the apex and supplies to the mid posterior aspect of the left ventricle (B).
Discussion
In this case report, we demonstrated misdiagnosed acute STEMI as SCMP due to unusual distribution of the LAD and the importance of prompt coronary angiography in the diagnosis and management of the patient.
SCMP is a reversible form of acute heart failure usually triggered by emotional or physical stresses.3) The usual form of SCMP shows a distinctive left ventricular apical ballooning pattern with normal epicardial coronary arteries.5) Usually patients with SCMP have a favorable outcome with appropriate medical managements.6) Recently, the guidelines for diagnosis of SCMP were published.7) In this guideline, SCMP is defined as an acute left ventricular apical ballooning, after myocardial infarction due to significant organic stenosis of coronal artery is excluded. Moreover, the incidence of SCMP in the acute coronary syndrome was 1-3%. So, the routine screening of presence of significant coronary artery disease is important in the diagnosis and management of the patients.
Despite the guidelines recommended taking coronary angiography to rule out significant epicardial coronary stenosis, the coronary angiography is not routinely performed in all patients with typical features of SCMP. Moreover, surmountable portion of SCMP patients have an incidental coronary artery disease because of advanced age. One study conducted in Japan showed that incidental coronary artery disease was found in about 10% of patients with SCMP.8) Another study showed nearly two thirds of the patients had coexisting atherosclerosis.9) Hence, some authors suggested that patients with coronary arterial disease in LAD, it should be carefully judged whether the disease causes left ventricular apical ballooning to avoid performing coronary revascularization unnecessarily.9),10)
In this patient, initial ECG was not compatible with acute STEMI and echocardiogram showed typical findings of SCMP. Moreover, because she had no previous clinical symptom suggesting coronary arterial disease, we initially diagnosed her of having SCMP without consideration of coronary angiography. However, we decided to have coronary angiography because her chest pain was unusual for SCMP patients and the intensity increased even after an analgesic treatment. The coronary angiography was very helpful in the early treatment of this patient. Also coronary angiography gave the answer of the echocardiographic feature that the distribution of her LAD was large enough to make apical ballooning and widespread ST-segment elevation without reciprocal change in the electrocardiographic exam.
In conclusion, even in a patient with typical presentation of SCMP like our case, the possibility of acute coronary syndrome should always be considered. And, if pain persists and when there is no contraindication, coronary angiography should be performed to rule out other acute coronary syndromes. Moreover, it would be better considering the possibility of the anatomical variation of the LAD can make similar features of apical ballooning.
References
- 1.Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. [Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases] J Cardiol. 1991;21:203–214. [PubMed] [Google Scholar]
- 2.Kurt IH. Coronary artery disease mimicking Tako-tsubo cardiomyopathy: a case report. Cases J. 2009;2:6374. doi: 10.4076/1757-1626-2-6374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park JH, Kang SJ, Song JK, Kim HK, Lim CM, Kang DH, Koh Y. Left ventricular apical ballooning due to severe physical stress in patients admitted to the medical ICU. Chest. 2005;128:296–302. doi: 10.1378/chest.128.1.296. [DOI] [PubMed] [Google Scholar]
- 4.Kim EM, Park JH, Park YS, Lee JH, Choi SW, Jeong JO, Seong IW. Catecholamines may play an important role in the pathogenesis of transient mid- and basal ventricular ballooning syndrome. J Korean Med Sci. 2008;23:898–902. doi: 10.3346/jkms.2008.23.5.898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharkey SW, Windenburg DC, Lesser JR, Maron MS, Hauser RG, Lesser JN, Haas TS, Hodges JS, Maron BJ. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol. 2010;55:333–341. doi: 10.1016/j.jacc.2009.08.057. [DOI] [PubMed] [Google Scholar]
- 6.Vidi V, Rajesh V, Singh PP, Mukherjee JT, Lago RM, Venesy DM, Waxman S, Pyne CT, Piemonte TC, Gossman DE, Nesto RW. Clinical characteristics of tako-tsubo cardiomyopathy. Am J Cardiol. 2009;104:578–582. doi: 10.1016/j.amjcard.2009.04.028. [DOI] [PubMed] [Google Scholar]
- 7.Kawai S, Kitabatake A, Tomoike H Takotsubo Cardiomyopathy Group. Guidelines for diagnosis of takotsubo (ampulla) cardiomyopathy. Circ J. 2007;71:990–992. doi: 10.1253/circj.71.990. [DOI] [PubMed] [Google Scholar]
- 8.Kurisu S, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Nakama Y, Maruhashi T, Kagawa E, Dai K, Matsushita J, Ikenaga H. Prevalence of incidental coronary artery disease in tako-tsubo cardiomyopathy. Coron Artery Dis. 2009;20:214–218. doi: 10.1097/MCA.0b013e3283299260. [DOI] [PubMed] [Google Scholar]
- 9.Winchester DE, Ragosta M, Taylor AM. Concurrence of angiographic coronary artery disease in patients with apical ballooning syndrome (takotsubo cardiomyopathy) Catheter Cardiovasc Interv. 2008;72:612–616. doi: 10.1002/ccd.21738. [DOI] [PubMed] [Google Scholar]
- 10.Jie BS, Her SH, Yoon HJ, Jeong HB, Park CH, Jeon JH, Kwak JW, Kim YC, Lee SJ, Jin SW. A case of ST-segment elevation myocardial infarction mimicking stress-induced cardiomyopathy. J Cardiovasc Ultrasound. 2008;16:29–32. [Google Scholar]