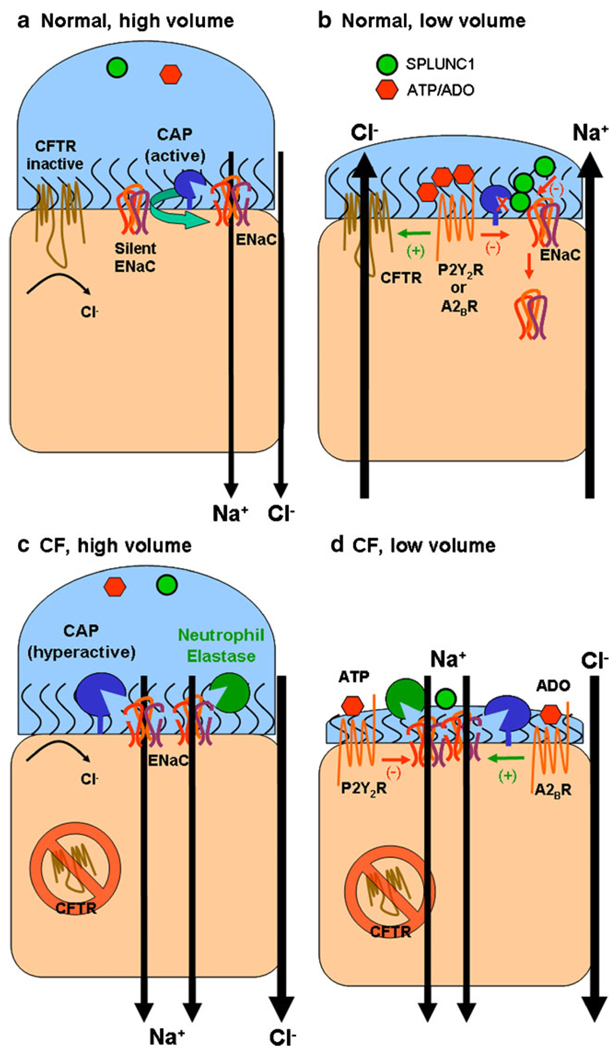
Fig. 4.
ENaC and ASL volume regulation. a In normal airways under high volume conditions, which may occur following glandular secretions, soluble inhibitors of ENaC proteolysis such as SPLUNC1 or purinergic inhibitors such as adenosine or ATP may be diluted to such an extent that ENaC is fully active, leading to Na+-led isotonic ASL absorption with Cl following through the paracellular pathway. Most non-cleaved, silent ENaCs are likely to be converted to cleaved active ENaCs by endogenous cell surface CAPs. Due to low levels of ATP and adenosine, CFTR and TMEM16A (not shown) are inactive and no Cl secretion occurs. b As ASL volume returns to steady-state levels, SPLUNC1 accumulates in the ASL in sufficient quantities to prevent the conversion of silent ENaCs to active ENaCs and SPLUNC1 may also reduce surface ENaC levels. Adenosine also accumulates to sufficient levels to activate CFTR (likely by stimulation of A2B adenosine receptors). This leads to a steady-state ASL height which approximates the height of outstretched cilia (7 µm). c High ASL volume conditions may occur in CF airways after inhalation of hypertonic saline. Under these conditions, Na+ absorption dominates, as in normal airways. d However, as ASL volume is reduced in CF airways, regulatory molecules such as SPLUNC1 are predicted to be ineffective at inhibiting ENaC, leading to an inappropriate reduction in ASL volume. In the absence of CFTR, active A2BR increases cAMP levels to stimulate rather than inactivate ENaC, further driving the reduction in ASL volume. Thus, unlike NL airways, CF airways are unable to make the switch from an absorbing to a secreting epithelia and ASL volume depletion results