Abstract
This study evaluated the effectiveness and treatment costs associated with a stepped care protocol of exposure and response prevention (EX/RP) for obsessive compulsive disorder (OCD). In the current open trial, patients (N = 14) began with self-directed EX/RP and minimal therapist guidance over the course of six weeks (Step 1). During this phase of treatment, no therapist-directed exposures were conducted. Those who did not respond optimally to Step 1 went on to Step 2, which consisted of 15 sessions of twice-weekly therapist directed exposures. Results of this study show promise for stepped care utilizing EX/RP for some patients with OCD, with a response rate of 88% and a 60% reduction on the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) score among treatment completers. Significant improvements were found in Y-BOCS from pre to post treatment for both Step 1 and Step 2 completers. Forty-five percent of participants (n = 5) responded following completion of Step 1, resulting in reduced cost of treatment among these participants. All participants who responded to Step 1 maintained acute gains during the brief follow-up period. Limitations include a small sample size and high attrition rate.
Keywords: Cost and cost analysis, Treatment outcomes, Bibliotherapy, Cognitive behavior therapy, Exposure therapy
Exposure and response prevention (EX/RP) is considered the psychosocial treatment of choice for OCD (Koran, Hanna, Hollander, Nestadt, & Simpson, 2007). EX/RP has consistently demonstrated superior results compared to pharmacotherapy, particularly in the area of relapse prevention (Abel, 1993; Van Balkom et al., 1994). In a study comparing EX/RP to clomipramine, for example, 62% of the sample and 86% of treatment completers who received therapist directed EX/RP were rated as responders, compared to 42% and 48% of those who received clomipramine (Foa et al., 2005). Further, although there are no studies directly comparing the long-term financial costs of EX/RP versus pharmacotherapy, it is likely that pharmacotherapy produces greater long-term costs than EX/RP, given the need for long-term maintenance with medication (Marks, 1997).
Despite empirical evidence for the efficacy of EX/RP, most individuals with OCD do not receive this treatment (Mancebo et al., 2006; Torres et al., 2007). Underutilization of EX/RP may be due to several factors, such as limited availability of clinicians trained to provide EX/RP, as well as the required time and financial commitment during the acute phase of the treatment. Although EX/RP may be less costly in the long run, it requires approximately 30 hours of direct clinician time and an estimated cost of $4370 (in 1995 dollars) over a relatively short period of acute treatment (several months)
In recent years, there has been considerable research on alternative forms of psychosocial treatments, including those for OCD, that aim to reduce cost, staff and patient burden, as well as increase treatment accessibility. Although these treatments are promising, not all individuals respond to these less restrictive forms of EX/RP. For example, in a study comparing computer guided versus clinician guided EX/RP, 38% of those who received computer guided EX/RP were rated as responders, compared to 60% of those in the therapist guided EX/RP group (Greist, Marks, Baer, Kobak, Wenzel, Hirsh, et al., 2002). Similarly, a randomized controlled trial comparing therapist directed EX/RP to self-directed EX/RP with bibliotherapy reported response rates of 65% and 25%, respectively (Tolin et al., 2007). Thus, a limitation of these less restrictive forms of EX/RP is that it leaves a substantial minority of patients that do not respond to the less restrictive EX/RP without adequate treatment. An alternative to these less restrictive forms of EX/RP is a stepped care approach. Stepped care refers to a self-correcting algorithm that is intended to provide the least restrictive and most effective treatment for each patient, potentially reducing time, cost, and associated patient and clinician burden of treatment.
To our knowledge, there has only been one published study utilizing EX/RP in a stepped care model for OCD. In a pilot study of stepped care EX/RP with 11 individuals with OCD (Tolin, Diefenbach, Maltby, & Hannan, 2005), patients began with bibilotherapy EX/RP (Step 1), followed by self-directed EX/RP with minimal therapist contact (Step 2) if they did not respond to the first step of treatment. Those who did not respond to Step 2 received traditional therapist-directed EX/RP for twelve 90-120 minute sessions (Step 3). Results of this study were promising, with comparable treatment efficacy and superior cost-effectiveness to previously published studies utilizing traditional EX/RP.
The aim of the present study was to examine the effectiveness and cost effectiveness of a refined stepped care treatment for OCD by condensing the original three step protocol into a two-step program of OCD treatment. We decided to condense the three step protocol to two steps, given that only a 3.5% reduction (d = .07) was observed in patients between Step 1 and Step 2 in the pilot study, suggesting that Step 2 provided minimal benefit to those who did not respond to Step 1. Combining the initial two steps condensed the time prior to therapist directed EX/RP to six rather than twelve weeks for those who did not respond to the minimal therapist contact condition. We also included a one month follow-up evaluation to examine sustainability of acute gains, a more detailed examination of the costs of treatment, and measurement of quality of life in addition to OCD symptoms.
Method
Participants
Fourteen participants with a primary diagnosis of OCD enrolled in the study. Inclusion criteria were: age 18 or older, primary DSM-IV-TR (American Psychiatric Association, 2000) diagnosis of OCD with a least one year symptom duration and moderate illness severity, as determined by a Yale-Brown Obsessive-Compulsive Scale (Y-BOCS; Goodman, Price, Rasmussen, Mazure, Delgado, et al., 1989; Goodman, Price, Rasmussen, Mazure, Fleischmann, et al., 1989) score of 16 or greater and Clinician’s Global Impression (CGI; Guy, 1976) score of 4 (“moderately ill”) or greater. Participants were stable on medication for at least one month and were not in concurrent psychotherapy, and had not already received an adequate trial of therapist-directed or self-directed EX/RP with bibliotherapy. Exclusionary criteria included any concurrent symptoms or diagnosis that required immediate attention and/or would interfere with the patient’s ability to engage in treatment, such as severe depression, serious suicidal or homicidal ideation, substance abuse/dependence, or lifetime diagnosis of a psychotic disorder, pervasive developmental disorder, or mental retardation. Table 1 depicts demographic and baseline data.
Table 1.
Sample Description (N = 14)
| N (%) | M (SD) | α | ICC | ||
|---|---|---|---|---|---|
| Female | 8 (57%) | ||||
| Age | 35 (11.08) | ||||
| Caucasian | 14 (100%) | ||||
| Employed full time | 3 (21.4%) | ||||
| Married | 4 (28.8%) | ||||
| Y-BOCS Total | 27.64 (4.30) | .87 | .71 | ||
| BDI – II total | 14.00 (7.08) | .80 | |||
| CGI Severity | 5.57 (.67) | ||||
| Sheehan Disability Scale |
5.86 (2.29) | .72 | |||
| Comorbid Diagnoses (At least one) |
6 (43%) | ||||
| Social Phobia | 5 (36%) | ||||
| GAD | 2 (14%) | ||||
| Dysthymic Disorder | 2 (14%) | ||||
| Specific Phobia | 1 (7%) | ||||
| Psychotropic medication |
Any | 9 (64.29%) | |||
| SRI* | 8 (57.14%) | ||||
| Benzodiazepines | 4 (28.57%) | ||||
Note. Y-BOCS = Yale-Brown Obsessive Compulsive Scale; BDI = Beck Depression Inventory - II; CGI = Clinician Global Impression Scale.
Measures
Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV; Brown, Di Nardo, Lehman, & Campbell, 2001)
The ADIS-IV was used to determine Axis I diagnoses. Reliability for the various DSM-IV categories contained in the ADIS-IV extends from good to excellent (with the exception of Dysthymic Disorder), with kappa coefficients ranging from .56 - .86 (Brown, et al., 2001). Raters for the present study were trained to criterion in the use of the ADIS-IV, with the requirement of 100% diagnostic match and within 1 point clinical severity rating with a previously-trained rater on three interviews. A subsample of three (21%) assessments were reviewed and rated by a second clinician. There was perfect interrater agreement for diagnosis of OCD and other anxiety disorders (қ = 1.0). There was one instance of diagnostic disagreement for a depressive disorder.
Yale-Brown Obsessive Compulsive Scale (Y-BOCS; Goodman, Price, Rasmussen, Mazure, Delgado, et al., 1989; Goodman, Price, Rasmussen, Mazure, Fleischmann, et al., 1989)
The Y-BOCS is a ten item clinician administered interview that assesses the severity of OCD symptoms. Evaluators for this study were trained to criterion to administer the Y-BOCS, with the requirement that they match within one point on each item and within two points on the total score with a previously-trained rater.
Clinical Global Impression Scale (CGI; Guy, 1976)
The CGI is commonly used in psychotherapy and pharmacotherapy trials to obtain clinician ratings of global symptom severity and symptom improvement. The severity subscale ranges from 1 (normal, not at all ill) to 7 (extremely ill) and the improvement subscale ranges from 1 (very much improved) to 7 (very much worse).
Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996)
The BDI-II is a 21 item self-report measure of depressive symptoms.
Sheehan Disability Scale (SDS; Leon, Shear, Portera, & Klerman, 1992)
The SDS is a self-report measure of impairment in psychosocial functioning. Participants indicate on an 11-point scale ranging from 0 (not at all) to 10 (very severely) how impaired they are in their work, social, and family functioning.
Procedure
Independent evaluations
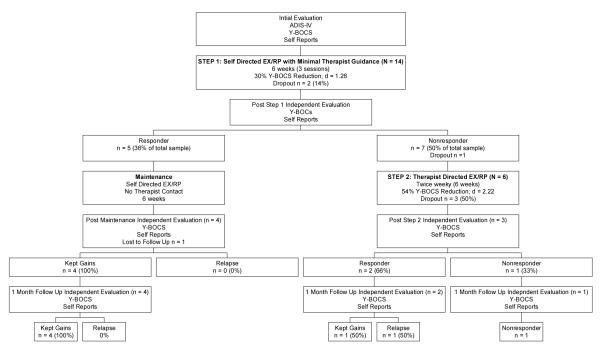
An independent evaluator (two licensed psychologists and two postdoctoral fellows supervised by licensed psychologists) who was not otherwise involved in the patient’s treatment conducted all evaluations. Figure 1 depicts the time points of the independent evaluations.
Figure 1.
Study Procedures & Treatment Outcome for Each Clinical Step
Note. All participants were requested to return for a one-month follow-up evaluation after the post Step 2 or post maintenance evaluation, including those who had prematurely discontinued their treatment through the study.
Responder Status
Criterion for determining response to each step of the treatment was created in order to determine whether participants should receive further treatment after Step 1 and to determine clinical response to each step. Responder status was based upon clinically significant change (CSC) (Jacobson & Truax, 1991), defined as the combination of reliable change (change that is significantly greater than would be expected by chance given the known test-retest reliability of the measure) and clinical change (a post-treatment score that is within 2 SD of the nonclinical mean). CSC on the Y-BOCS was thus operationalized as a reduction of 5 or more points plus a post-treatment score of 13 or less [this score is comparable to other definitions of clinical remission (Simpson, Huppert, Petkova, Foa, & Liebowitz, 2006) and is 3.4 SD below the pre-treatment mean in the present sample]. Relapse was defined as an occurrence in which a previous responder no longer met these criteria.
“Step Up” Criteria
Due to the infrequent (biweekly) clinician contact during Step 1, safety monitoring criteria were established to allow a “step up” to Step 2 treatment prior to the end of the six weeks of Step 1. Participants were instructed to contact their therapist if they experienced worsening of their OCD symptoms, increase in depressed mood, or any suicidal ideation. Based on this contact, the therapist would determine the need for a formal evaluation by the IE for the possibility of an early “step up.”
Treatment
Therapists in the study included licensed psychologists, and postdoctoral fellows and a graduate student who were supervised by licensed psychologists. All therapists received formal didactic training in providing EX/RP as well as the stepped care protocol and had experience providing EX/RP for OCD. During Step 1, participants met with their therapist for three sessions, each lasting 20-40 minutes, over the course of six weeks. During their initial session, participants were provided with a self-help EX/RP guide, “Stop Obsessing!” (Foa & Wilson, 2001) and reading guidelines for the next six weeks. The therapist also provided psychoeducation about the cognitive behavioral model of OCD, and the rationale and effectiveness of EX/RP. During the initial and subsequent two sessions, the therapist’s function was to provide support, problem-solve any difficulties related to and unrelated to OCD, enhance motivation, and provide recommendations on how to improve self-directed EX/RP. No therapist-directed exposures were conducted. Step 2 consisted of 12 sessions of therapist directed EX/RP, as outlined by Foa and Kozak (1997). Each session lasted 90-120 minutes.
Results
Missing Data
Data were analyzed using SPSS v. 15 with SPSS Missing Value Analysis v. 7.5 (SPSS, 1997). Examination of missing data on the Y-BOCS and CGI showed that 2 (14.3%) of patients were missing data at post-Step 1, 4 (28.6%) were missing data at post-Step 2, and 5 (35.7%) were missing data at 1-month follow-up. Examinations of skewness and kurtosis indicated that these variables were reasonably normally distributed; therefore, untransformed scores were used for imputation of missing values. Little’s Missing Completely at Random (MCAR; Little & Rubin, 1987) test was not significant for the Y-BOCS [χ2 (9) = 12.59, p = 0.182] or for the CGI [χ2 (14) = 15.16, p = 0.367], suggesting no non-random patterns to the missingness in the data, although it is acknowledged that power for this analysis was low.
Treatment Adherence and Competence
A psychologist otherwise uninvolved in the study or in the participant’s treatment evaluated a random selection of sessions (nine from Step 1 and six from Step 2). Therapist competence and adherence for both steps fell within the good to excellent ranges.
Treatment Outcome
Figure 1 illustrates treatment outcome for all assessment points2. Of the 14 patients who entered Step 1, two (14%) discontinued prematurely; one participant was lost to contact, and another reported withdrawing from the study due to dislike of completing questionnaires for research. One participant (7%) was “stepped up” to begin Step 2 prior to completing Step 1 due to an increase in OCD symptoms, according to the “step up” criteria described above. This participant, and five out of the six remaining Step 1 nonresponders (total n = 6) entered Step 2. Of these, three (50%) dropped out prior to completing Step 2. One participant withdrew due to a family crisis, another due to dislike of exposures; one participant was withdrawn due to needing a higher level of care, as he was minimally compliant with the study treatment and his OCD symptoms were exacerbating a pre-existing medical condition. One Step1 nonresponder dropped between Step 1 and Step 2.
To examine changes in OCD symptoms, we conducted one-way repeated measures ANOVAs for two primary outcome variables, the Y-BOCS total score and the clinician’s CGI severity rating, using the three time points (pre-treatment, post Step 2 or post maintenance for Step 1 responders, and one month follow-up). We conducted both completer and intent to treat analyses (replacing missing values using the regression method described above). Among treatment completers, there were significant differences in the Y-BOCS between the three assessment time points (Wilk’s Λ = .78, F[2, 5] = 29.6, p = .002, η2p = .92). Pairwise comparison with Bonferroni corrections revealed that there was significant reduction in the Y-BOCS from pre to post-treatment (p = .001) and from pre-treatment to one month follow-up (p = .016), but no significant differences from post-treatment to one-month follow-up (p > .05). Similarly, intent to treat (ITT) analyses found significant differences in the Y-BOCS across the three time points (Wilk’s Λ = .19, F[2, 12] = 25.04, p < .001, η2p = .81), with significant reductions from pre to post-treatment (p < .001) and pre-treatment to follow-up (p < .001) but not from post-treatment to follow-up (p = 1.0). For the clinician rated CGI severity rating, there were significant differences across the three time points for both treatment completers (Wilk’s Λ = .79, F[2, 5] = 28.99, p = .002, η2p = .92) and the ITT sample (Wilk’s Λ = .20, F[2, 12] = 24.12, p < .001, η2p = .80). Bonferroni-corrected pairwise comparisons found significant differences from pre to post treatment (p = .001), as well as from pre-treatment to follow-up (p < .001), on clinician rated CGI severity ratings. No significant differences were found from post-treatment to follow-up (p = 1.0).
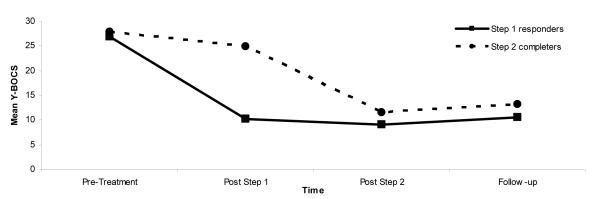
Overall, therefore, the stepped care protocol had a dropout rate of 50% and a CSC rate of 71% (ITT analysis) to 88% (completer analysis), with an average of 7 treatment sessions per treatment-responding patient. Mean reduction in Y-BOCS total score from pre to post treatment was 16.56 (SD = 5.64) or 60% among treatment completers and 14.08 (SD = 8.17) or 51% among the ITT sample. Eighty-eight percent (n =7) of treatment completers were rated as much improved or very much improved on the CGI at their last assessment. Figure 3 illustrates Y-BOCS scores at each assessment point by responder status to Step 1.
Figure 3.
Mean Y-BOCS Scores by Response to Clinical Steps
Note. Step 1 responders (n = 5; 36%); Step 2 completers (n = 3; 21%)
Quality of Life
Total scores on the SDS were used to examine any potential changes in quality of life from pre to post treatment and follow-up. Repeated measures ANOVA’s revealed significant differences in the SDS over time among treatment completers (Wilk’s Λ = .14, F[2, 5] = 15.00, p = .008, η2p = .86) and the intent to treat sample (Wilk’s Λ = .11, F[2, 12] = 47.94, p < .001, η2p = .89). Bonferroni-corrected pairwise comparisons of the SDS across the three time points (pre-treatment, post Step 2 or post maintenance, one-month follow-up) showed significant differences from pre to post treatment (p < .01) and from pre to follow-up (p < .01) but no differences between post treatment and follow-up. Results were equivalent with completer or intent to treat sample. Total scores on the SDS decreased from pre to post treatment, with an average pre-treatment score indicating moderate impairment in work, social, and family functioning (M = 5.57, SD = 2.23 for treatment completers; M = 5.87, SD = 2.29 for the intent to treat sample) and an average post-treatment score indicating mild impairment (M = 2.11, SD = 1.05 for treatment completers; M = 2.26, SD = 1.15 for the intent to treat sample).
Cost Analyses
Both the direct and indirect costs of treatment were calculated for each patient. Based on Medicare billing costs of $66.54 for a 20-30 minute session (90804) and $96.35 for a 45-60 minute session (90806), we calculated each Step 1 session to cost $66.54 and each Step 2 session to cost $192.70 (two 90806) (Centers for Medicare and Medicaid Services, 2007). Table 2 illustrates a breakdown of various cost differences between Step 1 and Step 2 responders. Using the Satterthwaite method (Satterthwaite, 1946) to account for differences in variance between Step 1 and Step 2 responders, we found the differences in both the direct (t1 = 68.5, p < .001, one tailed) and total cost (t1 = 9.7, p < .03, one tailed) between Step 1 and Step 2 responders to be statistically significant. The average Step 1 responder spent 32 fewer hours in treatment, waiting for treatment, or driving to and from treatment compared to Step 2 responders. Therapists spent 20 hours less for each Step 1 responder compared to Step 2 responders. With an estimated 12- month prevalence of 1% (Kessler, Chiu, Demler, & Walters, 2005) and a 42% response rate to Step 1, nationwide savings of offering a Stepped Care program may translate to $2.9 billion (direct treatment costs) to $3.9 billion (direct and indirect cost of treatment) annually in the U.S.
Table 2.
Differential Costs between Step 1 and Step 2 Responders
| Average Cost for Step 1 Responder |
Average Cost for Step 2 Responder |
Difference in Cost | |
|---|---|---|---|
| Patient direct cost | $112 | $992 | $879a |
| Payer direct cost | $87 | $1487 | $1400a |
| Total direct cost | $200 | $2479 | $2279a |
| Patient indirect cost | $88 | $731 | $643 |
| Provider Indirect cost | $48 | $168 | $120b |
| Total Cost | $335 | $3378 | $3042b |
Note. Patient direct cost = deductible and coinsurance paid by patient; Payer direct cost = cost of session paid by third party payer (e.g. Medicare, commercial insurance); Total direct cost = the combination of patient and payer direct costs; Patient indirect cost = indirect costs of participating in treatment including lost wages and travel costs*, provider indirect costs = Labor cost not reimbursed by insurance, such as preparing for session, and cost of travel for off-site sessions; Total cost = Total cost of treatment including all direct and indirect costs to patient, payer, and provider
p < .05,
p < .01
one tailed test using Satterhwaite method to account for differences in variance in costs between Step 1 and Step 2 responders
Lost wages associated with treatment were calculated by totaling the amount of time each patient spent in treatment sessions, traveling to and from treatment, and waiting for treatment sessions and multiplying the sum by the median U.S. hourly wage in 2008 of $15.57 (Bureau of Labor Statistics, 2009). For calculation of travel costs to and from treatment sessions, we utilized the 2008 standard mileage rate of 19 cents per mile for medical related mileage (Internal Revenue Service, 2009).
In order to examine the cost effectiveness of the entire Stepped Care protocol, we calculated a cost effectiveness ratio by dividing the cost of treatment by the degree of change in total Y-BOCS score at post treatment (post Step 2 or post maintenance). This method of calculating a cost effectiveness ratio has been used in previous stepped care studies (Otto, Pollack, & Maki, 2000; Tolin, et al., 2005) to examine not only the cost of treatment, but also as it relates to efficacy. Cost effectiveness ratios were derived for both the intent to treat and completer sample to address the impact of attrition on cost effectiveness. Among treatment completers, this yielded cost effectiveness ratios of $12 in direct treatment costs and $23 in total costs per 1% change and $43.97 in direct costs and $62.74 in total costs per 1 point change on the Y-BOCS. Among the intent to treat sample, cost effectiveness ratios were $17 in direct treatment costs and $26 in total costs per 1% change and $63.02 in direct costs and $95.63 in total costs per one point change on the Y-BOCS. Thus, the cost effectiveness ratio in this study was superior than that reported in the previous stepped care study (Tolin, et al., 2005), with a cost effectiveness ratio of $103.06 in direct costs per Y-BOCS point among treatment completers. The cost effectiveness ratios of both stepped care studies were superior than that of other studies of therapist directed EX/RP, which ranged from $116 (McLean et al., 2001) to $241 (Abramowitz, Foa, & Franklin, 2003) per change in one Y-BOCS point in direct costs.
Discussion
Results of this study show promise for a stepped care protocol of EX/RP for OCD, with a response rate of 88% and a 60% reduction in Y-BOCS total score among treatment completers. The response rate in this study was comparable to a previously published study of therapist-directed EX/RP (86%) (Foa, et al., 2005) as well as the response rate (86%) of the previous stepped care study (Tolin, et al., 2005). The response rate to Step 1 in this study was similar to the combined response rates of Step 1 (bibliotherapy only) and Step 2 (self-directed EX/RP with minimal therapist contact) in our previous pilot study. Thus, it appears as though combining the first two steps from the pilot study (bibliotherapy with therapist supported EX/RP) produces similar results while reducing the length of time required to achieve symptom improvement for some participants. Further, the cost effectiveness ratio of this trial was superior than that of the pilot study, suggesting that a two step protocol may be financially superior to a three step protocol. Improvements following treatment were also evident in a measure of quality of life with the SDS, suggesting that improvements associated with treatment translated to positive changes in major life functioning areas (work, family, social functioning).
The response rates of this stepped care study, as well as the previously published pilot study were superior to those reported in other studies of minimal therapist EX/RP (Greist, Marks, Baer, Kobak, Wenzel, Hirsch, et al., 2002; Kenwright, Marks, Graham, Franses, & Mataix-Cols, 2005; Tolin, et al., 2007). Unlike other minimal therapist EX/RP studies, participants in this study who did not respond to treatment after Step 1 received therapist directed EX/RP. Thus, the stepped care protocol of this study may account for the superior results compared to other studies that only utilized self-directed or minimal therapist EX/RP.
A stepped care protocol has many advantages that were highlighted in this study. Because the stepped care protocol is self-correcting, each patient only receives the least restrictive and effective amount of treatment. By reducing the burden associated with EX/RP, both financially as well as the time commitment for treatment, a stepped care program may be more acceptable to patients. Furthermore, by reducing the providers’ burden of providing effective treatment (time required to treat each patient), each practitioner trained in EX/RP will be able to see more patients with OCD.
There are limitations to this study and the stepped care method of EX/RP. The small sample size, with only seven treatment completers, significantly limits the generalizability of the results. As this was a small open trial, we cannot compare the effectiveness or cost effectiveness of stepped care treatment to standard EX/RP. Furthermore, a longer follow-up period is needed to evaluate the risk of relapse following stepped care treatment compared to standard EX/RP.
Another limitation of this study is the relatively high attrition rate (50%), which was substantially higher compared to the Foa et al. (2005) study (28%) as well as the pilot stepped care study (37%). Most participants cited reasons for withdrawing from the study that appeared unrelated to the stepped care protocol. One participant who withdrew during Step 2, however, reported feeling discouraged about not responding to Step 1. It is possible that nonresponse to Step 1 treatment or the delay in receiving Step 2 may increase attrition among those who do not respond to Step 1. Again, a randomized controlled trial comparing attrition rates among those assigned to a stepped care protocol or standard EX/RP is needed to address this issue.
Despite some limitations, stepped care appears to be a promising approach in improving the cost, acceptability, and accessibility of EX/RP for OCD. A significant proportion of patients (36%) responded following Step 1 and did not require more intensive (Step 2) treatment. Identification of pre-treatment factors, such as presence of social anxiety and poorer general mental health, as was identified as indicators for poor response to self-help for panic disorder (Baillie & Rapee, 2004), can further refine stepped care EX/RP by matching each patient to the least restrictive/costly and effective treatment.
Acknowledgments
This study was funded by the National Institute of Mental Health. We would like to thank our consultants for their contribution to the study: Dr. Edna Foa, for developing the treatment manuals and providing assistance in the refinement of the stepped care protocol; Dr. Suzanne Gleason for statistical analyses related to costs of treatment; Dr. Stewart Agras for assistance in revising the treatment manual and design of the stepped care protocol; Dr. Linda Frisman, for assistance in improving minority recruitment; Dr. Ralitza Gueorguieva for statistical analyses. We also thank Dr. Suzanne Meunier for serving as an independent rater, Dr. Melissa Norberg for serving as a study therapist, and Christina Ryan for her assistance with the study.
Footnotes
One participant reported reading another self-help book for OCD while in Step 1. A participant who declined Step 2 treatment reported increasing the dosage of her SSRI as well as initiating psychotherapy during the follow-up period. These participants were not excluded from analyses.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abel JL. Exposure with response prevention and serotonergic antidepressants in the treatment of obsessive compulsive disorder: a review and implications for interdisciplinary treatment. Behaviour Research and Therapy. 1993;31(5):463–478. doi: 10.1016/0005-7967(93)90127-g. [DOI] [PubMed] [Google Scholar]
- Abramowitz JS, Foa EB, Franklin ME. Exposure and ritual prevention for obsessive-compulsive disorder: effects of intensive versus twice-weekly sessions. Journal of Consulting and Clinical Psychology. 2003;71(2):394–398. doi: 10.1037/0022-006x.71.2.394. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th Text Revision ed Author; Washington, DC: 2000. [Google Scholar]
- Baillie AJ, Rapee RM. Predicting who benefits from psychoeducation and self help for panic attacks. Behaviour Research and Therapy. 2004;42:513–527. doi: 10.1016/S0005-7967(03)00157-8. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory. 2nd ed Psychological Corporation, Harcourt, Brace; San Antonio, TX: 1996. [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110(1):49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics . Occupational Empolyment and Wages Summary, 2008. United States Department of Labor; Washington, D.C.: 2009. [Google Scholar]
- Centers for Medicare and Medicaid Services . Revised 2007 Medicare Part B Physician and Nonphysician Practitioner Fee Schedule. First Coast Service Options, Inc.; Jacksonville, FL: 2007. [Google Scholar]
- Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, et al. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. American Journal of Psychiatry. 2005;162(1):151–161. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- Foa EB, Wilson R. Stop obsessing!: How to overcome your obsessions and compulsions. Bantam Books; New York: 2001. [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, et al. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Archives of General Psychiatry. 1989;46(11):1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry. 1989;46(11):1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Greist JH, Marks IM, Baer L, Kobak KA, Wenzel KW, Hirsch MJ, et al. Behavior therapy for obsessive-compulsive disorder guided by a computer or by a clinician compared with relaxation as a control. Journal of Clinical Psychiatry. 2002;63(2):138–145. doi: 10.4088/jcp.v63n0209. [DOI] [PubMed] [Google Scholar]
- Greist JH, Marks IM, Baer L, Kobak KA, Wenzel KW, Hirsh MJ, et al. Behavior therapy for Obsessive-Compulsive Disorder guided by a computer or clinician compared with relaxation as a control. Journal of Clinical Psychiatry. 2002;63(2):138–145. doi: 10.4088/jcp.v63n0209. [DOI] [PubMed] [Google Scholar]
- Guy W. U.S. Government Printing Office; Washington, DC: Assessment manual for psychopharmacology. 1976
- Internal Revenue Service United States Department of the Treasury; Washington, DC: Standard Mileage Rate, 2008. 2009
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kenwright M, Marks I, Graham C, Franses A, Mataix-Cols D. Brief scheduled phone support from a clinician to enhance computer-aided self-help for obsessive-compulsive disorder: randomized controlled trial. Journal of Clinical Psychology. 2005;61(12):1499–1508. doi: 10.1002/jclp.20204. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koran LM, Hanna GL, Hollander E, Nestadt G, Simpson HB. Practice guideline for the treatment of patients with obsessive-compulsive disorder. American Journal of Psychiatry. 2007;164(7 Suppl):5–53. [PubMed] [Google Scholar]
- Leon AC, Shear MK, Portera L, Klerman GL. Assessing impairment in patients with panic disorder: The Sheehan Disability Scale. Social Psychiatry and Psychiatric Epidemiology. 1992;27:78–82. doi: 10.1007/BF00788510. [DOI] [PubMed] [Google Scholar]
- Little RJ, Rubin DB. Statistical analysis with missing data. Wiley; New York: 1987. [Google Scholar]
- Mancebo MC, Eisen JL, Pinto A, Greenberg BD, Dyck IR, Rasmussen SA. The brown longitudinal obsessive compulsive study: treatments received and patient impressions of improvement. Journal of Clinical Psychiatry. 2006;67(11):1713–1720. doi: 10.4088/jcp.v67n1107. [DOI] [PubMed] [Google Scholar]
- Marks I. Behaviour therapy for obsessive-compulsive disorder: a decade of progress. Canadian Journal of Psychiatry. 1997;42(10):1021–1027. doi: 10.1177/070674379704201002. [DOI] [PubMed] [Google Scholar]
- McLean PD, Whittal ML, Thordarson DS, Taylor S, Sochting I, Koch WJ, et al. Cognitive versus behavior therapy in the group treatment of obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology. 2001;69(2):205–214. [PubMed] [Google Scholar]
- Otto MW, Pollack MH, Maki KM. Empirically supported treatments for panic disorder: costs, benefits, and stepped care. Journal of Consulting and Clinical Psychology. 2000;68(4):556–563. [PubMed] [Google Scholar]
- Satterthwaite FW. An Approximate Distribution of Estimates of Variance Components. Biometrics Bulletin. 1946;2:110–114. [PubMed] [Google Scholar]
- Simpson HB, Huppert JD, Petkova E, Foa EB, Liebowitz MR. Response versus remission in obsessive-compulsive disorder. Journal of Clinical Psychiatry. 2006;67(2):269–276. doi: 10.4088/jcp.v67n0214. [DOI] [PubMed] [Google Scholar]
- SPSS I. SPSS Missing Value Analysys 7.5. Chicago, IL: 1997. [Google Scholar]
- Tolin DF, Diefenbach GJ, Maltby N, Hannan SE. Stepped care for obsessive-compulsive disorder: A pilot study. Cognitive and Behavioral Practice. 2005;12:403–414. [Google Scholar]
- Tolin DF, Hannan S, Maltby N, Diefenbach GJ, Worhunsky P, Brady RE. A randomized controlled trial of self-directed versus therapist-directed cognitive-behavioral therapy for obsessive-compulsive disorder patients with prior medication trials. Behavior Therapy. 2007;38(2):179–191. doi: 10.1016/j.beth.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Torres AR, Prince MJ, Bebbington PE, Bhugra DK, Brugha TS, Farrell M, et al. Treatment seeking by individuals with obsessive-compulsive disorder from the british psychiatric morbidity survey of 2000. Psychiatric Services. 2007;58(7):977–982. doi: 10.1176/ps.2007.58.7.977. [DOI] [PubMed] [Google Scholar]
- Van Balkom A, Van Oppen P, A. V, van Dyck R, Nauta M, Vorst H. Meta-analysis on the treatment of OCD: Comparsion of antidepressants, behaviour therapy and cognitive therapy. Clinical Psychology Review. 1994;14:359–381. [Google Scholar]