Abstract
Sudden gains in psychotherapy are characterized by large and relatively stable decreases in psychiatric symptoms and have been associated with cognitive shifts in clients and shown to predict superior treatment outcomes in studies of depression and, to a lesser extent, anxiety disorders. The purpose of this study was to examine prevalence and impact of sudden gains during a transdiagnostic cognitive-behavioral group therapy (CBGT) for anxiety disorders, as well as the temporal relationship between sudden gains and cognitive changes. Data were used from two trials of transdiagnostic CBGT for anxiety disorders (n = 130). Criteria for determining sudden gains in anxiety symptoms were based upon previous research on sudden gains from trials of cognitive behavioral treatments for major depressive disorder. A total of 17 out of 98 (17.3%) clients experienced at least one sudden gain, with three clients showing two sudden gains during treatment. Three patients showing a sudden gain experienced a reversal of these gains, although one of these three had a subsequent second sudden gain. Clients experiencing sudden gains showed greater overall improvement following treatment than did clients who did not experience a sudden gain, with 65% of the sudden gainers' overall improvement accounted for by the sudden gain. Greater cognitive change in the pregain sessions was observed for clients with a sudden gain than those not showing a sudden gain. This finding lends support to the theory of cognitive mediation through CBGT in which substantial cognitive changes in pregain sessions lead to greater improvement overall.
The concept that psychotherapy clients may have periods of significant symptomatic relief within a short time period, termed Sudden Gains by Tang and DeRubeis (1999), has existed throughout the history of psychotherapy. Breuer and Freud (see Freud, 1955) wrote extensively regarding catharsis, the conscious awareness of unconscious or repressed conflicts resulting in sudden emotional release and problem resolution. Similarly, Eysenck (1981) and Fontenelle et al. (2000) describe sudden decreases in symptoms following planned and unplanned, respectively, intense conditioning experiences. Despite this, within behavioral and cognitive psychotherapy movements, sudden gains have received only recent attention.
Tang and DeRubeis (1999) reported the first intensive empirical investigation of sudden gains in symptom reduction during cognitive-behavioral therapy for depression. Using archival data of 61 depressed clients from two efficacy studies, Tang and DeRubeis examined session-by-session changes in Beck Depression Inventory (BDI; Beck & Steer, 1987) scores and identified 29 instances of sudden gains occurring among 24 clients. Tang and DeRubeis (1999) originally defined sudden gains by to the following criteria: “A sudden gain occurred between session N and session N + 1 if (a) the gain was at least 7 BDI points (BDIN − BDIN+1 ≥ 7); (b) the gain represented at least 25% of the pregain session's BDI score (BDIN − BDIN+1 ≥ 0.25 × BDIN); and (c) the mean BDI score of the three therapy sessions before the gain (sessions N − 2, N − 1, and N) was significantly higher than the mean BDI score of the three therapy sessions after the gain (sessions N + 1, N + 2, and N + 3) using a two-sample t test, with an alpha of .05” (Tang & DeRubeis, 1999; p. 895).
These criteria were later (Tang et al., 2005) rephrased as:
Absolute magnitude: The gain was at least 7 BDI points, BDIN − BDIN+1 ≥ 7.
Relative magnitude: The gain represented at least 25% of the pregain session's BDI score, BDIN − BDIN−1 ≥ .25 BDIN.
Relative to symptom fluctuation: The mean difference between the BDI scores of the 3 sessions before the gain and the 3 sessions after the gain was at least 2.78 times greater than the pooled standard deviations of these two groups BDI scores.
On average, these gains represented 51% of their total BDI reduction during treatment, and clients evidencing a sudden gain showed significantly lower BDI scores at post-treatment and 6- and 18-month follow-up periods than did clients who did not show a sudden gain during treatment. Sudden gains occurred throughout the 16-week treatment protocol, with a median and modal occurrence at session 5.Subsequent coding of session audiotapes by blind assessors suggested that during the session preceding the sudden gain, clients demonstrated substantial cognitive changes whereas significantly fewer signs of cognitive change were identified in sessions more distal to the sudden gain. Following the sudden gain, clients showed increased therapist alliance and continued signs of positive cognitive change. The exact mechanisms underlying the relationship between cognitive changes, sudden gains, and improved outcomes are unclear although it may be related to a number of factors, including: enhanced treatment motivation following sudden improvement or more complete modification of biased cognitive structures.
Since publication of the Tang and DeRubeis (1999) paper, others have replicated these findings across independent samples of depressed outpatients receiving CBT for depression. Tang, DeRubeis, Beberman, and Pham (2005) reported highly similar rates of sudden gains in an independent archival sample of cognitive therapy and cognitive-behavioral therapy for depression. Further, evidence of cognitive change in the pregain session was again observed. Hardy et al. (2005) reported similar, albeit less pronounced, results based on data from cognitive therapy for depression conducted in a non-research-driven community practice. In contrast, however, Busch and colleagues (2006) were unable to replicate these findings. Instead, they found that sudden gains did not predict better outcome, and that sudden gains occurred later in cognitive therapy for depression than previous studies have noted (median occurrence at session 10 of 20). Additionally, Busch et al. (2006) reported numerous instances of pre-treatment and first session gains, although it was unclear if these gains were similar to later sudden gains in terms of causal influence (e.g., expectancies, non-specific factors, cognitive change, etc.). Kelly, Roberts, and Ciesla (2005) also found discrepant results than that of Tang and DeRubeis (1999), in that there were no significant differences detected among sudden gainers and non-sudden gainers after 12 sessions of CBT for depression as measured by BDI scores. Kelly et al. (2005) found that those who experienced a sudden gain in the first third of treatment did have significantly greater symptom reduction and were more likely to be treatment responders than those who did not experience a sudden gain and those who did not experience an early sudden gain, when controlling for initial BDI scores. Kelly and colleagues (2005) also concluded that cognitive changes were not related to early sudden gains in their sample because cognitive techniques were not introduced until session seven in their protocol, suggesting that other mechanisms of change contribute to early success in treatment.
Given impact of the literature on sudden gains in depression, it is somewhat surprising that published research on sudden gains during cognitive-behavioral therapy for other mental or emotional disorders has been limited. To our knowledge, only two studies of sudden gains in CBT for anxiety disorders have been conducted to date. Using data from 107 clients with social phobia receiving exposure therapy or cognitive-behavioral therapy, Hofmann et al. reported an incidence of sudden gains of roughly 19%. No differences in treatment outcome, however, were observed between the clients with social phobia who did and did not display a sudden gain. Further, Hofmann et al. did not find evidence that cognitive changes preceded sudden gains at a rate higher than that observed in control sessions. Clerkin, Teachman, and Smith-Janik (2008) found evidence for sudden gains during CBT for panic disorder. The majority of the sudden gains occurred between the first and second sessions, with most of these individuals showing a reversal of gains followed by an eventual return to pre-reversal levels. Sudden gains occurring after the second session (n = 6, 14.0%) or later were associated with greater pre- to post-treatment changes in anxiety sensitivity, which the authors considered to be a proxy for cognitive change.
The current study sought to examine incidence and impact of sudden gains in a transdiagnostic cognitive-behavioral group therapy (CBGT) for anxiety, and to explore the relationship between sudden gains and cognitive changes in this population. It was anticipated that sudden gains would be apparent during CBGT for anxiety and would account for a sizable proportion of overall treatment gains. It was specifically hypothesized that, (1) those experiencing sudden gains would show superior outcomes than those not showing a sudden gain, and (2) during sessions prior to which a sudden gain occurred, participants would show greater cognitive change than did those not experiencing a sudden gain.
Method
Participants
Archival data from two trials of a transdiagnostic CBGT for anxiety disorders (Norton, 2008; Norton, in press) were examined for the current study. Norton (2008) reported data from 52 clients with an anxiety disorder who participated in an open trial of transdiagnostic CBGT for anxiety disorders. Norton (manuscript in press) provided data from 78 participants receiving transdiagnostic CBGT for anxiety in a randomized controlled trial by comparison to a relaxation/educational-supportive treatment (R/EST) condition. Both trials used the same structured treatment protocol (Norton & Hope, unpublished), inclusion and exclusion criteria, recruitment methods, and assessment protocols, with the only significant difference being the possibility of randomization to the R/EST condition in the second trial. Participants in the two samples did not differ significantly on any of the primary study variables, Fs = 0.07 – 1.81, ps = .183 – .789.
Participants (55.6% women) ranged in age from 18 to 71 years (M = 33.94, SD = 11.53), and were moderately racially diverse (60.3% Caucasian, 17.8% Hispanic, 11% African American, 5.5% Asian, 5.5% Other). Most were single, divorced, or widowed (59.2%), while the remainder were married or cohabitating. Participants had primary diagnoses of social anxiety disorder (n = 40, 42.1%), panic disorder with or without agoraphobia (n = 33, 34.8%), generalized anxiety disorder (n = 12, 12.6%), agoraphobia without history of panic (n = 3, 3.2%), anxiety disorder not otherwise specified (n = 3, 3.2%), specific phobia (n = 2, 2.1%), and obsessive-compulsive disorder (n = 2, 2.1%). Sixty-two percent of the sample met criteria for one or more comorbid Axis I diagnoses, including depressive disorders (n = 26), generalized anxiety disorder (n = 24), social phobia (n = 13), specific phobia (n = 10), panic disorder with or without agoraphobia (n = 8), obsessive-compulsive disorder (n = 4), substance abuse or dependence (n = 3), posttraumatic stress disorder (n = 2), body dysmorphic disorder (n = 2), and adjustment disorder (n = 1).
Of the total treatment initiator sample of 130, thirty-two did not have sufficient data to establish a sudden gain. Twelve only attended one session, three did not attend any consecutive sessions (needed to establish Criteria 1 and 2), and seventeen did not attend a sufficient number of consecutive or temporally close sessions to establish symptom fluctuation before and after the possible sudden gain (needed to establish Criterion 3). As a result, data from 98 clients were analyzed. Although participants were nested within group format, Norton (in press) indicated that group-level intra-class correlations were below thresholds reported by Muthén and Satorra (1995) as needing to be modeled.
Assessments
All participants received a structured diagnostic assessment at intake, using the Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV; Brown, Di Nardo, & Barlow, 1994) and were given a Clinician Severity Ratings (CSR) for each diagnosis. Participants completed the State-Trait Anxiety Inventory – state version (STAI-S; Spielberger, 1983) prior to the beginning of each session.
Anxiety Disorders Interview Schedule for DSM-IV
The Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV; Brown, Di Nardo, & Barlow, 1994) is a semi-structured diagnostic interview designed to assess the presence, nature, and severity of DSM-IV anxiety, mood, and somatoform disorders, as well as previous mental health history. A recent large scale analysis of the ADIS-IV offers strong support for the reliability of diagnoses using the ADIS-IV (Brown, Di Nardo, Lehman, & Campbell, 2001). Clinician Severity Ratings (CSR), a component of the ADIS-IV, are subjective clinician ratings to quantify the severity for each disorder diagnoses with the ADIS-IV. CSR range from 0 (not at all severe) to 8 (extremely severe/distressing). A CSR of 4 (moderate impairment) is generally considered the cut-off for a disorder of clinical significance (e.g., Heimberg et al., 1990). While diagnostic reliability data were not available from Norton (2008), Norton (in press) reported 86% diagnostic agreement from a random subset of 25% of the diagnostic interviews that were observed and rated by a second independent interviewer who was blind to diagnosis.
State-Trait Anxiety Inventory – State Version
The state form of the State-Trait Anxiety Inventory (STAI-S; Spielberger, Gorsuch, Luschene, Vagg, & Jacobs, 1993) is a 20-item measure designed to assess state anxiety. STAI-S items are scored on 1 (Not at all) to 4 (Very much so) scales, with a total score ranging from 20 to 80. The psychometric properties of the STAI-S are strong across multiple populations (Spielberger et al., 1993), and the measure has demonstrated sensitivity to anxiety treatment effects (e.g., Fischer & Durham, 1999). At the initial time-point (Session 1), the STAI-S was highly internally consistent in this sample (α = .948).
Patient Cognitive Change Scale – Anxiety (PCCS-A)
The original PCCS developed by Tang, Strunk, and DeRubeis (unpublished) and used in both Tang and DeRubeis (1999) and Tang et al. (2005) was obtained and modified to reflect anxiety-related thoughts and beliefs. Prior to analysis, PCCS-A scores were examined for possible confounding associations that might influence the results. Additional items were generated but discarded, as they directly tapped events that occurred in specific sessions (e.g., engaging in exposure). As such, the PCCS-A was computed only from Items 1 to 4 (1: Became aware of a belief, 2: Changed belief, 3: Became aware of a schema, 4: Changed a schema; average inter-item r = .72). Items were rated from DVDs of sessions using five-point (1–5) scales ranging from no progress to extraordinary progress.
A total of 42 individuals (31 non-sudden gainers, 11 sudden gainers) across 10 group sessions was rated. Ratings were attempted for all 17 individuals showing a sudden gain, although data from six sudden gainers were unavailable due to damaged DVD recordings. Rating for the 31 non-sudden gainers were made on clients in the same session and group as an individual showing a sudden gain, although raters were blind to which participant had experienced the sudden gain. Reliability of PCCS-A items between two independent raters was acceptable, with an average item correlation of r = .62. In cases where a client was rated more than once, only the first rating (if that individual showed no or two sudden gains) or the rating corresponding to the sudden gain session (for those rated during both sudden gain and non-sudden gain sessions) was used.
Definition of Sudden Gains
The following criteria, based on Tang et al. (2005), were implemented here to define a sudden gain:
Absolute magnitude: As discussed by Hofmann et al. (2006) several studies have established a sudden gain using Jacobson and Truax's (1991) reliable change index. Using STAI scores from the first session (α = .948, sd = 12.161), a reliable change index value of 7.90 was obtained, and subsequently rounded up to 8. Therefore, a potential sudden gain was defined by improvements of at least 8 points on the STAI.
Relative magnitude: Gains represented at least 25% of the pregain STAI score.
Relative to symptom fluctuation: Given the considerable variability that can be observed in session-by-session scores, sudden gains need to be sufficiently large in relation to fluctuations before and after the gain. Although concerns about autocorrelations and necessary magnitudes of gains (e.g., t(4) = 2.78 vs. 2.50) have been made, for the sake of consistency with the majority of the sudden gain literature, a critical t of 2.78 was used here. As such, the mean difference between the STAI-S scores of the three sessions before the gain and the three sessions after the gain (two sessions before or after session 3 and 10 respectively) was at least 2.78 times greater than the pooled standard deviations of these two groups of sessions' STAI-S scores.
Some (e.g., Busch et al., 2006; Gaynor et al, 2003) have developed strategies for evaluating early gains (i.e., gains occurring after the first session). However, the mechanisms of such early changes are unclear and may be related to treatment effects, non-specific effects, or simple relief over having initiated therapy. We, therefore, opted not to include early gains in our analyses.
Transdiagnostic Treatment Protocol
The transdiagnostic treatment protocol utilized in this study consisted of a 12-week schedule of CBGT that met for two hours per session on consecutive weeks. Groups were capped at 6 to 8 members and enrollment was closed, in that new participants would not be added to an existing group after the group was initiated. The treatment protocol is highly structured and followed a standardized set of therapeutic procedures (Norton & Hope, unpublished). The first session of treatment orients participants to the group format, group rules, and the structure of the treatment, as well as psychoeducational information regarding how and why anxiety disorders develop for some individuals. The next two sessions focus on educating members regarding the importance of thoughts, how anxious thinking typically involves negative automatic thoughts, and cognitive restructuring techniques. In the following six sessions, participants incrementally work up their individualized fear hierarchy by performing the cognitive restructuring techniques prior to an in–session exposure. Exposures are typically in vivo but sometimes include imaginal exposure depending upon the nature of the fear and feasibility of reproducing the feared situation. Participants are then asked to perform the exposure over the following week for homework. Sessions ten and eleven address more broad use of the cognitive restructuring techniques to extend to global patterns of negative automatic thinking related to their particular anxious style (e.g. recurrent perfectionistic patterns, chronically negative views of self, the world, or the future). The final session wraps up by reflecting on gains made in treatment, and discusses how to deal with stressors, lapses, and relapses. Other than differences in the specific exposure exercises employed (e.g., public speaking for a social phobia, interoceptive exercises for panic disorder, etc.), the treatment protocol is identical for individuals with different DSM-IV anxiety disorder diagnoses.
Results
Occurrences of Sudden Gains
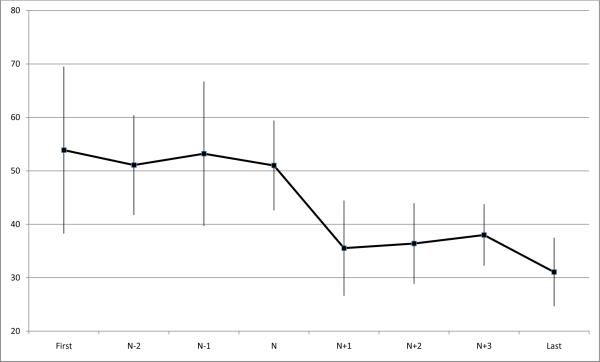
A total of 17 (17.3%) clients experienced at least one sudden gain, with three clients showing two sudden gains during the treatment. Thus, 20 sudden gains were identified across the 12-session treatment. Sudden gains were distributed across the sessions (median session number = 5), with three sudden gains after session 2, two after session 3, three after session 4, three after session 5, two after session 7, one after session 8, and three after session 10. The average magnitude of the sudden gains was 14.76 points (sd = 5.36) on the STAI-S (see Figure 1), accounting for 64.68% of the average gain of 22.82 (sd = 17.44) units by those who showed a sudden gain, and was unrelated to the timing/session of the gain2.
FIGURE 1.
Average sudden gain. State-Trait Anxiety Inventory-State version (STAI-S; X-axis) mean scores and SD (error bars) shown for First, N - 2, N - 1, N, N + I, N + 2, N + 3, and Last (Y-axis) are means of the corresponding sessions from the 17 sudden gains in our sample, with session N as the pregain session.
Sudden gains were observed across individuals with primary diagnoses of panic disorder (n = 8; 21.6% of panickers), social anxiety disorder (n = 7; 15.9%), and generalized anxiety disorder (n = 2; 16.7%), and diagnosis was unrelated to the occurrence, χ2 (2, n = 88) = 0.07, p = .966, or timing of a sudden gain, F (2,13) = 0.71, p = .511, among those with diagnoses of panic disorder, social anxiety disorder, or generalized anxiety disorder3. Participants who had a sudden gain showed significantly higher STAI scores at session 1 than did those not showing a sudden gain, F(1,79) = 4.48, p = .038. No difference in number of sessions attended emerged between those showing or not showing a sudden gain, F(1,97) = 2.64, p = .108.
Impact of Sudden Gains on Outcome
To examine the role, if any, of sudden gains on treatment outcomes, several indices of outcomes were utilized. First, final session STAI-S scores were used in isolation. Second, improvement scores were computed by subtracting the last available STAI-S from the first available STAI-S score. Third, outcome was measured using pre-treatment and post-treatment CSRs for those clients who completed treatment and returned for a post-treatment assessment.
In contrast to clients who did not show a sudden gain, those who did show a sudden gain had significantly lower last-available-session STAI-S scores, F (1,96) = 5.70, p = .019, and greater STAI-S improvement, F (1,96) = 14.83, p < .001. Repeated measures ANOVA using pre and post-treatment CSR scores for the primary diagnosis revealed a non-significant trend suggesting that participants showing a sudden gain (pre: M = 6.46, SD = 1.13; post: M = 3.82, SD = 1.72) improved to a greater degree than did those not showing a sudden gain (pre M = 5.73, SD = 1.01; post: M = 4.00, SD = 1.67), F (1,20) = 3.17, p = .09. The CSR data are limited, however, as they are based on a subset of clients who completed the post-treatment assessment. The occurrence of a sudden gain was not related to any demographic variables including participant age, race, sex, level of education, or performance on the Shipley Vocabulary Test (Zachary, 1986), all ps < .24.
Reversal of Sudden Gains
A sudden gain is seen as having reversed when a client reports an increase in symptoms of 50% or more of the sudden gain magnitude. Three clients (17.6%) showing a sudden gain experienced a reversal of a sudden gain, although one of these three had a subsequent second sudden gain. Although underpowered, analyses suggested no difference in outcomes between participants who did and did not experience a reversal of their sudden gain, Fs < 1.55, ps > .233.
Cognitive Change prior to Sudden Gains
One-way between-groups Analysis of Variance was used to compare cognitive change, as assessed using the modified PCCS-A, between those who did and did not show a sudden treatment gain. Consistent with the hypothesis that sudden gains would be preceded by cognitive changes, greater cognitive change was observed for clients with a sudden gain (M = 2.73, SD = 1.95) than those not showing a sudden gain (M = 1.05, SD = 1.67), F (1,29) = 6.35, p = .017.
Discussion
This study aimed to replicate and extend Tang and DeRubeis' (1999) original finding that depressed clients who experienced a large decrease in symptom severity in a single between-sessions interval, or sudden gain, had better improvement at the end of treatment than those who did not experience a sudden gain. Consistent with the first hypothesis, evidence generally indicated that those showing a sudden gain had better end-of-treatment outcomes than did those not showing a sudden gain. Further, those showing a gain of 8 points or greater but not meeting Criteria 2 (relative magnitude) or 3 (relative to symptom fluctuation) showed significantly less improvement than did those meeting all criteria for a sudden gain. The present study provides support for these findings in a mixed anxiety disordered sample that received twelve sessions of Cognitive Behavioral Group Therapy. Consistent with previous findings (Hofmann et al., 2006), no evidence for a specific session in which change occurred was found in this sample, as sudden gains occurred equally in the first half of treatment as the last half, and were dispersed intermittently throughout the sessions. Similar to Tang and DeRubeis' (1999) study, only a small number (n = 3) of sudden gainers in this study experienced a reversal of improvement, and one of the three experienced a second sudden gain. This suggests that changes made in these sessions are typically enduring, and 65% of the sudden gainers' overall improvement was accounted for by the sudden gain.
The finding that those experiencing a sudden gain tended to have higher session 1 anxiety scores was unexpected given previous findings. Of the sudden gains studies for depression, none of those reporting a comparison of pre-treatment BDI scores reported differences (Busch et al., 2006; Hardy et al., 2005; Tang & DeRubeis, 1999; Tang et al., 2002). However, studies examining sudden gains during treatment for anxiety are more mixed, with two studies (current study; Hofmann et al., 2006) suggesting higher pre-treatment scores for those showing sudden gains, while Clerkin et al. (2008) did not find pre-treatment differences between those showing sudden gains and those who did not. Future research should aim to clarify the extent to which these pre-treatment differences in anxiety symptoms are robust, and the extent to which they may be a function of differences in the measurement tools (i.e., all of the depression studies used the same instrument, while the anxiety studies all used different assessments), regression to the mean, or other factors.
Incidence of sudden gains found in the current study (17.3%) is similar to that reported by Hofmann et al. (2006) in their study of sudden gains in CBT for social phobia (19%), and that reported by Clerkin et al. (2008) in their study of CBT for panic disorder (14%). Interestingly, these estimates are considerably lower than those reported by 39%–46% in the studies of CBT for depression (Kelly et al., 2005; Tang & DeRubeis, 1999; Tang et al., 2005). It is wholly unclear why such differences have been observed, but several possible explanations exist. First, such discrepancy could relate to the malleability of depression versus anxiety disorder or to differences in the implementation of specific active ingredients in the treatments for anxiety and depression. These possibilities are supported by data reported by Howard, Kopta, Krause, and Orlinsky (1986) who demonstrated that clients with depression tended to show a faster and steeper dose-response curve than did clients with anxiety disorders. Alternatively, the discrepancy in the observed incidences of sudden gains may relate to aspects of the instruments used to define sudden gains. All of the studies reviewed here that examined sudden gains in depression utilized the same self-report instrument, the Beck Depression Inventory, to define sudden gains. Additional research using other instruments should be conducted. Furthermore, studies of sudden gains in anxiety and depression treatment should strive to use assessment beyond symptom frequency or intensity measures, including measures of disorder-specific features and indices of impairment and distress. Finally, research into sudden gains using “unified” CBT protocols for anxiety and depression (e.g., Barlow, Allen, & Choate, 2004; McEvoy & Nathan, 2007) may shed light on the different incidences of sudden gains.
Additionally, results indicated that, consistent with the second hypothesis, sudden gainers experienced greater cognitive change than non-sudden gainers. These findings lend support to Tang and DeRubeis' theory of cognitive mediation through CBGT in which substantial cognitive changes in the pregain sessions lead to greater improvement overall. Although ratings on the PCCS suggest that cognitive changes preceded the sudden gain session, it cannot be stated definitively that all improvements were due to cognitive shift alone. Additional factors that could potentially account for the sudden gains include regression toward the mean, spontaneous remission, environmental changes, or other non-cognitive therapeutic variables.
The finding of cognitive changes preceding sudden gains in CBT for anxiety disorders is consistent with Clerkin et al. (2008), but in contrast to Hofmann et al. (2006). Neither Clerkin et al. or Hofmann et al. utilized direct observational estimates of cognitive change; relying on changes on the Anxiety Sensitivity Index and Self Statement during Public Speaking Test, respectively, to infer cognitive change. In the current study, we followed the approach adopted by Tang and DeRubeis (1999; Tang et al., 2005) and had assessors who were blind to sudden gain status, observe and make ratings of cognitive change from video recordings of sessions. It is interesting that studies using direct observation consistently support the “cognitive change” hypothesis whereas those using change on self-report instruments (e.g., Kelly et al., 2005, Hofmann et al., 2006; but see Clerkin et al., 2008) typically do not. Future research is needed to explore and resolve which approach, if either, is producing more valid results.
Despite these results generally converging with previous studies, several limitations must be considered. First, no alternate explanations for the sudden gains beyond cognitive change were evaluated, and it is unclear if similar gains would be observed in non-cognitively oriented therapies. Second, some analyses were hampered by limited sample sizes. Finally, primary or comorbid diagnoses of OCD and PTSD were highly under-represented in this sample, so the extent to which these results may generalize to these populations remains unclear. Even so, the current study highlights the importance and impact of sudden symptom remission in CBT for anxiety disorders, and provides additional support for the hypothesis that such gains may be a function of earlier cognitive shifts.
Acknowledgments
The project described was supported by Grant Number K01MH073920 from the National Institute of Mental Health awarded to PJN. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Footnotes
Note: The Standard Deviations from the current sample were similar to those reported from normative samples by Speilberger et al., (1993)
Note: There were 54 incidents of STAI gains of 8 or greater that did not meet Criterion 2 or 3. However, participants with these gains showed significantly less post-treatment improvement, F = 7.36, p = .008, than did those meeting all sudden gain criteria.
Due to limited sample sizes, individuals with primary diagnoses of agoraphobia without history of panic, anxiety disorder not otherwise specified, specific phobia, and obsessive-compulsive disorder were not included in these analyses.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Beck Depression Inventory manual. Harcourt Brace; San Antonio, TX: 1987. [Google Scholar]
- Brown TA, Di Nardo PA, Barlow DH. Anxiety disorders interview schedule for DSM-IV (Adult Version) Graywind; Albany, NY: 1994. [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Busch AM, Kanter JW, Landes SJ, Kohlenberg RJ. Sudden gains and outcome: A broader temporal analysis of cognitive therapy for depression. Behavior Therapy. 2006;37:61–68. doi: 10.1016/j.beth.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Clerkin EM, Teachman BA, Smith Janik SB. Sudden gains in group cognitive-behavioral therapy for panic disorder. Behaviour Research and Therapy. 2008;46:1244–1250. doi: 10.1016/j.brat.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck HJ. Behavior therapy and the conditioning model of neuroses. International Journal of Psychology. 1981;16:343–370. [Google Scholar]
- Fisher PL, Durham RC. Recovery rates in generalized anxiety disorder following psychological therapy: An analysis of clinically significant change in the STAI-T across outcome studies since 1990. Psychological Medicine. 1999;29:1425–1434. doi: 10.1017/s0033291799001336. [DOI] [PubMed] [Google Scholar]
- Fontenelle L, Soares ID, Marques C, Rangé B, Medlowicz MV, Versiani M. Sudden remission of obsessive-compulsive disorder by involuntary, massive exposure. Canadian Journal of Psychiatry. 2000;45:666–667. [PubMed] [Google Scholar]
- Freud S. The standard edition of the complete psychological works of Sigmund Freud. Hogarth; London: 1955. [Google Scholar]
- Hardy GE, Cahill J, Stiles WB, Ispan C, Macaskill N, Barkham M. Sudden gains in cognitive therapy for depression: A replication and extension. Journal of Consulting and Clinical Psychology. 2005;73:59–67. doi: 10.1037/0022-006X.73.1.59. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Dodge CS, Hope DA, Kennedy CR, Zollo LJ, Becker RE. Cognitive behavioral group treatment for social phobia: Comparison with a credible placebo. Cognitive Therapy and Research. 1990;14:1–23. [Google Scholar]
- Hofmann SG, Schulz SM, Meuret AE, Moscovitch DA, Suvak M. Sudden gains during therapy of social phobia. Journal of Consulting and Clinical Psychology. 2006;74:687–697. doi: 10.1037/0022-006X.74.4.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard KI, Kopta SM, Krause MS, Orlinsky DE. The dose-effect relationship in psychotherapy. American Psychologist. 1986;41:159–164. [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kelly MAR, Roberts JE, Ciesla JA. Sudden gains in cognitive behavioral treatment for depression: When do they occur and do they matter? Behaviour Research and Therapy. 2005;43:703–714. doi: 10.1016/j.brat.2004.06.002. [DOI] [PubMed] [Google Scholar]
- McEvoy PM, Nathan P. Effectiveness of cognitive behaviour therapy for diagnostically heterogenous groups: A benchmarking study. Journal of Consulting and Clinical Psychology. 2007;75:344–350. doi: 10.1037/0022-006X.75.2.344. [DOI] [PubMed] [Google Scholar]
- Norton PJ. A comparison of transdiagnostic treatments for anxiety disorder: CBT and relaxation training. Behavior Therapy. doi: 10.1016/j.beth.2010.08.011. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton PJ. An open trial of a transdiagnostic cognitive-behavioral group therapy for anxiety disorder. Behavior Therapy. 2008;39:242–250. doi: 10.1016/j.beth.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Norton PJ, Hope DA. Anxiety treatment program: Therapist manual. unpublished. [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anxiety Inventory (STAI) Consulting Psychologists Press; Palo Alto, CA: 1983. [Google Scholar]
- Spielberger CD, Gorsuch RL, Luschene RE, Vagg PR, Jacobs GA. State-Trait Anxiety Inventory for adults. Mind Garden; Palo Alto, CA: 1993. [Google Scholar]
- Tang TZ, DeRubeis RJ. Sudden gains and critical sessions in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67:894–904. doi: 10.1037//0022-006x.67.6.894. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ, Beberman R, Pham T. Cognitive changes, critical sessions, and sudden gains in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 2005;73:168–172. doi: 10.1037/0022-006X.73.1.168. [DOI] [PubMed] [Google Scholar]
- Tang TZ, Strunk DR, DeRubeis RJ. Patient cognitive change scale. unpublished. [Google Scholar]