Abstract
The treatment of displaced calcaneal fractures remains controversial. Early surgical management to restore articular congruence and the structural function of the calcaneus is widely accepted as the best way to avoid the negative consequences of malunion. Concerns remain however regarding the best approach for reducing and maintaining reduction of these complex fractures, while minimizing the risk of surgical complications. The potential for serious wound complications is a major concern, particularly breakdown of the lateral calcaneal skin flap with the extensile lateral approach. Various approaches have been developed to try and balance the need for direct reduction of the articular surface while minimizing the potential for wound complications. Palmer originally described a laterally based approach through the sinus tarsi for direct visualization of the articular surface for reduction. He and others have found this approach to be useful and reasonably safe. At times, however, it may be necessary to extend the limits of a small incision over the sinus tarsi to treat adjacent fractures or to aid reduction in more complex fractures. In addition, a limited sinus tarsi incision without elevation of the lateral calcaneal skin flap does not allow for plate fixation, a notable advantage of the extensile lateral approach, particularly in gaining reduction of the body of the calcaneus. The authors have used an extended sinus tarsi approach to include placement of plate percutaneously beneath the lateral calcaneal skin flap through a sinus tarsi approach, and to treat adjacent fractures and soft tissue injuries. A clinical series of 13 patients (including 7 chronic smokers and 1 with diabetes and vascular disease) with closed displaced intra-articular calcaneal fractures (Sanders types II and III) were treated by open reduction and internal fixation via this approach. Adjacent fractures were treated through the same incision. Two patients developed wound complications. No wound complications occurred in smokers.
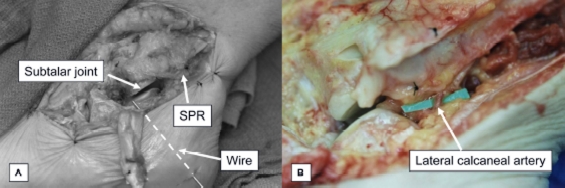
The vascular anatomy of the lateral calcaneal artery related to this approach was also studied with 16 cadaver legs. The lateral calcaneal artery (LCA) passed within 2 mm of the superior border of floor of the Superior Peroneal Retinaculum (SPR) at the midline of the peroneal sheath.
By avoiding dissection through the deep portion of the SPR, the lateral calcaneal artery can be protected, thus preserving the blood supply to the lateral calcaneal skin flap.
INTRODUCTION
Calcaneal fractures have long been recognized as a source of significant disability and remain one of the most difficult articular fractures to treat. There has historically been debate over the best approach for treating these fractures.1,4 The goal of operative treatment of calcaneal fractures is to obtain the best possible reduction of the articular surfaces and restoration of the architecture of the non-articular portions of the bone, and to hold this reduction with stable internal fixation.5,6 These goals must be balanced with the need to minimize the operative risks, especially the risk of wound healing complications. Operative and non-operative management have both been suggested for the acute treatment of calcaneal fractures, however it is generally accepted that in most cases operative treatment of displaced calcaneal fractures is warranted in order to avoid the negative consequences of malunion.2,6 Operative management can consist of reduction through an extensile open incision, limited incision or percutaneous techniques. Both lateral and medial approaches have been described, but the lateral approach allows direct exposure of the articular surface, while the medial approach is limited to reduction of the body. Various internal fixation techniques have been described, but a laterally based plate is commonly accepted to give the most rigid fixation.7,8 Since displaced calcaneus fractures present with various degrees of comminution and soft tissue trauma, it is advantageous for the calcaneal fracture surgeon to have a variety of methods of treatment to balance minimizing risks of wound complications against obtaining the best reduction possible.9
The widely used lateral approach to the calcaneus, described by Letournel2 and popularized by Zwipp,4 Atkins,10 Benirschke,11 and Sanders,6 has been termed, the extensile lateral approach. This approach provides excellent direct exposure of the calcaneal body as with the medial approach while also providing direct exposure of the articular surface. The wide exposure allows the surgeon to place a lateral plate which gives rigid control of the body reduction with lag screw fixation through the plate into the medial sustentacular fragment. This provides for reduction of the body fragment medially, even when extensive comminution of the lateral wall is present.2,6 This exposure relies on developing a lateral calcaneal flap that is supplied by the LCA which is the terminal branch of the peroneal artery.12 One drawback of this approach is the potentially catastrophic wound complications that can result in the need for a soft tissue flap, or rarely below-the-knee amputation.13 Gupta et al. reported a series of patients who underwent open reduction and internal fixation of the calcaneus with a modification of the Palmer incision.14 This modified incision differed from the one that Palmer described by being placed more dorsally and oriented more longitudinally like a typical approach to the sinus tarsi. This provided good exposure of the posterior facet, and unlike Palmer who used structural bone graft to support the articular reduction, they used internal fixation, consisting of interfragmentary compression screws. The authors obtained satisfactory reductions and minimal wound complications.
We describe an extensile sinus tarsi based approach, for open reduction of displaced calcaneal fractures that the senior author (J.F.) began using in 1999 based on the technique described by Gupta et al. for higher risk patients or those with concomitant fractures that could be addressed simultaneously. It affords placement of a lateral plate subcutaneously by using retrograde subperiosteal elevation of the lateral calcaneal skin flap. Screw fixation into the body of the calcaneus is gained by percutaneous screw placement posteriorly. In this way, direct reduction and rigid plate fixation is achieved as with the typical extensile lateral approach. The advantage of this approach is that it can be easily and safely extended to address other injuries. Proximally, the approach can be extended to include a directly lateral approach to the distal tibia, fibula and syndesmosis, which we have previously described.15 Distally the talus, calcaneocuboid joint and cuboid are easily accessed, without undue risk to the sural or superficial peroneal nerve. The protection of the lateral calcaneal artery is important to the success of the approach, as with the extensile lateral incision, and we also present a cadaver study to highlight the anatomy of the LCA relative to this surgical approach.
CONICAL CASE SERIES
We retrospectively reviewed thirteen patients who had undergone open reduction and lateral plate fixation without bone graft of closed displaced intraarticular calcaneus fractures using an extensile sinus tarsi approach. This approach was chosen at the discretion of the senior author (J.F.) in cases of patients at higher risk for wound complications such as smokers or those with concomitant injuries that could be treated from a lateral approach. The surgeries were all performed by the senior author (J.F.) between February 1999 and June 2002. During the same time period, the senior author used the extensile lateral approach for isolated calcaneal fractures in other patients not deemed as high risk for wound complications.
Preoperative computed tomography scans were obtained in all patients. Fractures were classified according to the classification system described by Sanders.6 Six patients had type II-A fractures, three patients had type II-B fractures, three patients had type III-AB fractures, one patient had a type III-AC fracture.
There were 12 males and one female with an average age of 45.1 years (range from 26-71 years). The mechanism of injury was a fall from a height in eight patients, motor vehicle accidents in three patients and snowmobile accidents in two patients. Seven patients were chronic smokers (average 1.5 packs per day). All were counseled to stop smoking. One patient had diabetes and vascular disease, with lateral calcaneal fracture dislocation impacted into the lateral ankle gutter.
Fixation was obtained using the following plates with screws: An Ace/Depuy titanium calcaneal perimeter plate in six patients, a Synthes calcaneal or cervical H-plate in five patients, and a Synthes 2.7 mm reconstruction plate in one patient. One patient had a calcaneal anterior process fracture with calcaneal-cuboid subluxation fused with a large staple.
Operative Technique
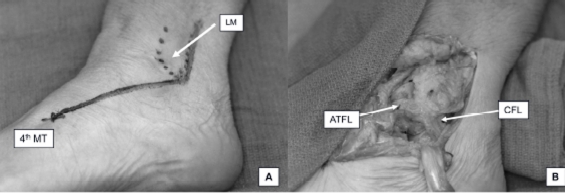
For exposure of an isolated calcaneal fracture, the patient is positioned either in full lateral or semi-lateral position with a hip bump. A skin incision is made longitudinally beginning 3cm above the tip of the lateral malleolus along the posterior border of the distal fibula. At the tip of the fibula, the incision is directed toward the base of the fourth metatarsal. This is carried distally to the level of the calcaneal-cuboid joint. The incision lies in a plane between the superficial peroneal nerve and the sural nerve. In this manner, both nerves can be left untouched within the subcutaneous fat. The dorsal communicating branch of the sural nerve may cross the field distally but is usually small in size and easily retracted. In some circumstances, the branch might be more proximal in the field and if necessary, it can be sharply transected near the point at which it branched from the sural nerve. The incision is deepened by mobilizing the sinus tarsi fat pad dorsally. The intermediate root of the inferior extensor retinaculum (IER) can be released too to gain better exposure of the fracture line passing obliquely through the angle of Gissane. The extensor digitorum brevis (EDB) muscle is sharply elevated off of the anterior process with the lateral root of the IER, and reflected dorsally and distally.
The peroneal tendons are retracted laterally between the superior peroneal retinaculum and IPR and the inferior peroneal retinaculum is released off of the bone to expose the lateral calcaneal wall down to the anterior process. The subcutaneous tissues overlying the peroneal tendons are left untouched which also preserves the sural nerve. With the anterior calcaneus and sinus tarsi exposed, the peroneal tendons below the SPR are retracted with a freer elevator placed along the lateral wall of the calcaneus and sharp dissection is used to perform retrograde subperiosteal elevation of the soft tissues off of the lateral calcaneus and proceeding to the tuberosity. Insertion of a broad elevator can enhance the retraction by placing the soft tissues under tension thus facilitating sharp elevation off of the lateral wall of the calcaneus. Care is taken to make sure that the elevator is not placed into the fracture, but lateral to the lateral wall fragment. The CFL can be transected initially when oriented more vertically. When the calcaneal insertion is elevated with the entire lateral calcaneal soft tissue flap, it remains in its anatomic relationship to the surrounding soft tissues and later reduces back to the calcaneus. It can later be re-approximated with a single stitch if desired. We have not done this uniformly. The SPR is opened if it requires repair or if inspection of the peroneal tendons warrants this. An anatomic repair can be performed. Care is taken to avoid any dissection of the floor of the SPR. Our cadaveric study shows that this inherently protects the LCA, which passes deep to and just along the proximal border of the SPR.
At this point, excellent direct visualization of the articular surface of the posterior facet is possible. Tilting the bed into Trendelenberg position and allowing the foot to invert over a cloth bump aids in visualizing the subtalar joint. The interosseous talo-calcaneal ligament (ITCL) could be transected, which allows the medial articular fragment to be better visualized by tipping into varus. This can aid visualization of the articular surface, but we avoid this in most cases because of the importance of this ligament as a primary stabilizer of the subtalar joint. It is possible that joint instability may result and could add to the chance of post-traumatic arthritis. A 4.5mm Shantz pin or a half ring with crossed tensioned olive wires can be used for traction and control of the tuberosity. The fracture is mobilized, comminution and interposed soft tissues are debrided and provisional reduction of the articular surface and body is held with K-wires. The fracture is typically reduced from anterior to posterior. The anterior process is reduced to the sustentaculum fragment, the lateral articular fragment(s) are reduced and pinned and the tuberosity is loosely reduced and provisionally pinned from posteriorly with pins into the sustentaculum or anterior process. An initial lag screw is placed across the posterior facet fracture lagging the joint fragments. Satisfactory articular reduction is gained and confirmed clinically and fluoroscopically with lateral, axial heel and Broden's views. Next a lateral plate is placed beneath the internally elevated soft tissue flap, and directly fixed to the anterior calcaneus and the articular fragments. The plate is not contoured and the lateral wall fragment typically reduces into the body of the calcaneus with lagging of the plate to the stable medial fragment. This creates a smooth lateral surface which is less likely to create impingement on the peroneal tendons. The screws for fixation to the tuberosity are placed percutaneously. Fluoroscopy can be utilized, but a small right angle hemostat can also be used to localize the holes for the percutaneous screws by visualizing the holes in the plate directly with retraction of the lateral soft tissues. Once the fixation is complete and final fluoroscopic or x-ray images obtained, the wound is thoroughly irrigated and the EDB and sinus tarsi fat pad reduced and sutured with absorbable sutures. The CFL can be repaired if desired. The skin is closed in two layers with 3-0 or 4-0 absorbable sutures and the skin with Nurolon. A gauze dressing is placed with a bolster, and a dressing of ABD pads is placed over the foot and ankle with an A-0 style splint16 using modest molding over the lateral wall to augment compression. The heel portion of the foot plate is left long to suspend the heel.
After the second case in the series, which was complicated by a wound hematoma, a small closed suction drain was placed into the wound and brought out dis-tally. The drain in our series was removed 24-48 hours postoperatively and wounds were examined on the second postoperative day. We currently do not suture the drains and we remove them at 24 hours through the dressing. Exposure and reductions are performed under tourniquet control.
All patients begin motion once the incision is well healed and the sutures are removed, which is usually 2 V2 - 3 weeks postoperatively. They remain non-weight bearing for 10-12 weeks.
RESULTS
Clinical case series
Four patients underwent ORIF with concurrent primary subtalar arthrodesis. Three were smokers and had fractures types III-AB, III-AC. In these cases, the articular surface damage was deemed to be too severe to warrant ORIF alone. Six patients underwent concurrent peroneal sheath and/or tendon reconstruction, six patients underwent concomitant lateral ankle ligament reconstruction, two patients underwent concurrent open reduction and internal fixation (ORIF) of a talar neck and head fracture respectively, and two patients underwent concurrent ORIF of fibular fractures.
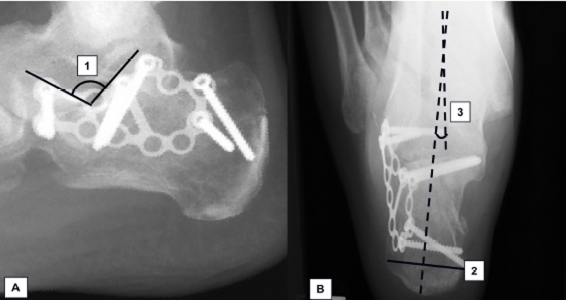
The average length of follow-up time was 19 (range from 2-41) months, excluding one patient who underwent subsequent below-knee amputation six weeks post-operatively. Of those patients who did not undergo primary subtalar arthrodesis, postoperative radiographs with Broden's views revealed articular reduction within two millimeters. Postoperative measurement of Bohler's angle averaged 29 (range 25-36) degrees and Gissane's angle averaged 131 (range 122-150) degrees (Figure 1). These angles were in the ranges of normal population.17,18
Figure 1.
Post-operative lateral and hindfoot alignment views demonstrating restoration of the calcaneus. (A) 1; Crucial angle of Gissane (B) 2; Calcaneal width 3; Tibio-Calcaneal angle.
Eleven patients healed their soft tissues uneventfully by three weeks. One patient had peripheral vascular disease and diabetes with a severely displaced lateral calcaneal fracture-dislocation into the lateral gutter of the ankle joint with significant fibular comminution. The patient had normal pain sensation and was given the option of surgery due to the severe injury to both the ankle and subtalar joints. This patient's postoperative course was complicated by wound dehiscence and infection, which was salvaged with a below-knee amputation. One patient sustained a lateral wound dehiscence due to a hematoma. It healed uneventfully after surgical debridement, closure and subsequent local care. After this episode, a medium hemovac drain was placed intra-operatively in all remaining patients with no subsequent wound healing complications.
Cadaveric Study of the Lateral Calcaneal Artery in Relation to the Modified Sinus Tarsi Approach
Sixteen lower extremity cadaver specimens were obtained through the University of Michigan Medical School Anatomic Donations program. The popliteal artery was cannulated with intravenous tubing and the arterial system was manually injected with silicone-based dye solution after cleansing with saline solution. Specimens were frozen overnight after allowing the dye to disseminate and consolidate.
After allowing the specimens to thaw, the extensile sinus tarsi approach was performed. The superficial portion of the SPR was divided, but the deep portion was preserved. The anterior flap was mobilized to the ankle to facilitate the photographic demonstration of the anatomy. After transection and removal of the peroneal tendons within the tendon sheath, the superior border of the deep fibers of the superior peroneal retinaculum was identified (Figure 2). The floor of the peroneal tendon sheath above the superficial peroneal retinaculum was transected longitudinally and the underlying posterior peroneal artery branch, or lateral calcaneal artery (LCA) was identified (Figure 3).
Figure 2.
Lateral ankle and hindfoot with incision markings for extensile sinus tarsi approach (A). Lateral Malleolus (LM) is dashed line. Lateral ankle ligaments and subtalar joint with peroneal tendons reflected.(B).
Figure 3.
(A) Deep dissection of lateral ankle and hindfoot. Posterior facet of calcaneus is exposed after release of the CFL. Markers denote proximal border of superior peroneal retinaculum. Note wire passed subcutaneously indicating extent of subperiosteal elevation that can be performed for lateral plate fixation. (B) Identification of lateral calcaneal artery deep to deep fibers of superior peroneal retinaculum. A marker is positioned at the posterior border of distal fibula indicating the surperior margin of the floor of the SPR.
Three measurements were made to define the location and orientation of the LCA relative to the superior border of the deep portion of the SPR. The first was the distance from the superior margin of the floor of the SPR, at the fibular attachment, to the point where the LCA emerged from the posterior margin of the fibula. The second measurement was made at the midline of the floor of the SPR. The third measurement was taken where the LCA crossed the posterolateral margin of the SPR.
The LCA was seen to consistently emerge from the posterior lateral edge of the fibula proximally and course distally behind the deep portion of the peroneal tendon sheath superior to the SPR. Three orientations of the LCA were noted as it passed distally: vertical, oblique and horizontal.
The LCA was found to emerge from the posterior fibular border an average of 10.6 (range from 2 to 23) millimeters proximal to the superior border of the deep fibers of the SPR. At the midline of the peroneal sheath, the average distance from the LCA to the SPR was 2.0 (range from 0 to 4) millimeters. In all specimens, the LCA traversed directly posterior to the lateral border of the deep portion of the SPR.
DISCUSSION
Various other open approaches have been described in treating calcaneus fractures. They include the extensile lateral approach, medial approach,19 combined lateral and medial approach,20 sinus tarsi approach21 and limited posterolateral approach.22 Palmer in 1948 initially described his lateral sinus tarsi approach with structural bone grafting beneath the depressed articular fragment.3 Essex-Lopresti in 1952 used a small sinus tarsi incision to elevate depressed joint fragments with Steinman pin fixation.1 These authors highlighted the value of direct access to the articular fracture for reduction.
The essential principles of reduction have endured. The goal of treatment is to achieve anatomic reduction of the articular surface of the subtalar joint and reduction of the tuberosity. With improvements in implants over time, rigid fixation with plates and screws has replaced bone grafting and percutaneous pinning as the usual method of maintaining reduction, with many authors favoring a lateral plate fixation.
Good to excellent clinical results have been published in patients undergoing open reduction and internal fixation with the extensile lateral approach, however high wound complication rates are reported.13,23,24 They include superficial epithelial necrosis, full-thickness skin sloughing, deep purulent infections and osteomyelitis. In a retrospective study by Abidi and Conti et al., risk factors included single layered closure, high body mass index, extended time between injury and surgery, and smoking.23 Folk et al. found that smoking, diabetes, and open fractures all increase the risk of significant wound complications and are cumulative.13
Past anatomic studies supported the conclusion that division of the LCA can lead to ischemia of the lateral calcaneal skin flap. It extended distally curving around the lateral malleolus and anteriorly supplying the posterior and inferior portions of the fasciocutaneous flap of the extensile lateral approach. Freeman et al. described in a study that the LCA passed at a mean of 31 mm. posterior to the lateral malleolus on a line from it to the insertion of the calcaneal tendon, at an average of 15 mm. anterior to the tendon.25 Borrelli et al. studied the vascularity of the lateral calcaneal flap and concluded that the lateral calcaneal artery was found to be responsible for the majority of the blood supply to the corner of the flap.12 They found that it emerged from the deep fascia of the leg 15 mm proximal to the tip of the lateral malleolus and 33 mm posterior to the posterior edge of the fibula and 11.5 mm anterior to the anterior edge of the Achilles tendon. They stated that the posterior vertical portion of the typical extensile lateral incision placed the LCA at risk to injury, which could lead to possible wound complications.
In a similar fashion we found the LCA to be at risk with this extended sinus tarsi approach if at the proximal edge of the floor of the SPR. The description of the relationship of the LCA to the SPR provides an identifiable landmark for this extended sinus tarsi approach. By avoiding dissection through the deep portion of the SPR, the LCA can be protected, thus preserving the blood supply to the lateral calcaneal skin flap. We have found that it is not clinically necessary to extend the deep dissection this far proximally as the exposure of the posterior subtalar articular surface is excellent with division of the CFL alone. It could be tempting, however, to carry the deep dissection farther proximally as it would provide even wider access to this area.
In conclusion, the extended sinus tarsi approach provides good exposure to the calcaneus for reduction and fixation and also provides exposure for concomitant treatment of injuries to the lateral ankle and talus. The incision can be extended to allow access to the distal tibia and fibula, talus and the lateral column of the foot.
Acknowledgments
The senior author (J.F.) would like to thank his fellowship director and mentor, Elly Trepman M.D. for introducing him to the modified Palmer approach, which formed the basis of this extended technique. Dr. Trepman is the senior author on the paper by Gupta et al.
REFERENCES
- 1.Essex-Lopresti P. The mechanism, reduction technique, and results in fractures of the os calcis. Br J Surg. 1952;39:395–419. doi: 10.1002/bjs.18003915704. [DOI] [PubMed] [Google Scholar]
- 2.Letournel E. Open treatment of acute calcaneal fractures. Clin Orthop Relat Res. 1993:60–67. [PubMed] [Google Scholar]
- 3.Palmer I. The mechanism and treatment of fractures of the calcaneus; open reduction with the use of cancelhus grafts. J Bone Joint Surg Am. 1948;30A:2–8. [PubMed] [Google Scholar]
- 4.Zwipp H, Tscherne H, Wulker N. [Osteosynthesis of dislocated intraarticular calcaneus fractures] Unfallchirurg. 1988;91:507–515. [PubMed] [Google Scholar]
- 5.Gould N. Lateral approach to the os calcis. Foot Ankle. 1984;4:218–220. doi: 10.1177/107110078400400416. [DOI] [PubMed] [Google Scholar]
- 6.Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraar-ticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993:87–95. [PubMed] [Google Scholar]
- 7.Hall MC, Pennal GF. Primary subtalar arthrodesis in the treatment of severe fractures of the calcaneum. J Bone Joint Surg Br. 1960;42-B:336–343. doi: 10.1302/0301-620X.42B2.336. [DOI] [PubMed] [Google Scholar]
- 8.Noble J, McQuillan WM. Early posterior subtalar fusion in the treatment of fractures of the os calcis. J Bone Joint Surg Br. 1979;61:90–93. doi: 10.1302/0301-620X.61B1.422642. [DOI] [PubMed] [Google Scholar]
- 9.Carr JB. Surgical treatment of intra-articular calcaneal fractures: a review of small incision approaches. J Orthop Trauma. 2005;19:109–117. doi: 10.1097/00005131-200502000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Eastwood DM, Langkamer VG, Atkins RM. Intra-articular fractures of the calcaneum. Part II: Open reduction and internal fixation by the extended lateral transcalcaneal approach. J Bone Joint Surg Br. 1993;75:189–195. doi: 10.1302/0301-620X.75B2.8444935. [DOI] [PubMed] [Google Scholar]
- 11.Benirschke SK, Sangeorzan BJ. Extensive intraarticular fractures of the foot. Surgical management of calcaneal fractures. Clin Orthop Relat Res. 1993:128–134. [PubMed] [Google Scholar]
- 12.Borrelli J, Jr., Lashgari C. Vascularity of the lateral calcaneal flap: a cadaveric injection study. J Orthop Trauma. 1999;13:73–77. doi: 10.1097/00005131-199902000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Folk JW, Starr AJ, Early JS. Early wound complications of operative treatment of calcaneus fractures: analysis of 190 fractures. J Orthop Trauma. 1999;13:369–372. doi: 10.1097/00005131-199906000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Gupta A, Ghalambor N, Nihal A, Trepman E. The modified Palmer lateral approach for calcaneal fractures: wound healing and postoperative computed tomographic evaluation of fracture reduction. Foot Ankle Int. 2003;24:744–753. doi: 10.1177/107110070302401003. [DOI] [PubMed] [Google Scholar]
- 15.Femino JE, Vaseenon T. The direct lateral approach to the distal tibia and fibula: a single incision technique for distal tibial and pilon fractures. Iowa Orthop J. 2009;29:143–148. [PMC free article] [PubMed] [Google Scholar]
- 16.Müller ME, Allgöwer M, Arbeitsgemeinschaft für Osteosynthesefragen . Berlin; New York: In Springer-Verlag; 1991. Manual of internal fixation : techniques recommended by the AO-ASIF Group; p. 750. pp. xxviii, p. [Google Scholar]
- 17.Rogers LF. New York: In Churchill Livingstone; 2002. Radiology of skeletal trauma; p. 2. v. (xii, 1406, 1430 p.) [Google Scholar]
- 18.Wulker N, Stephens M, Cracchiolo A. An atlas of foot and ankle surgery. St. Louis, Mo. London: Mosby; Martin Dunitz; 1998. [Google Scholar]
- 19.Burdeaux BD. Calcaneus fractures: rationale for the medial approach technique of reduction. Orthopedics. 1987;10:177–187. doi: 10.3928/0147-7447-19870101-29. [DOI] [PubMed] [Google Scholar]
- 20.Stephenson JR. Surgical treatment of dis placed intraarticular fractures of the calcaneus. A combined lateral and medial approach. Clin Orthop Relat Res. 1993:68–75. [PubMed] [Google Scholar]
- 21.Ebraheim NA, Elgafy H, Sabry FF, et al. Sinus tarsi approach with trans-articular fixation for displaced intra-articular fractures of the calcaneus. Foot Ankle Int. 2000;21:105–113. doi: 10.1177/107110070002100203. [DOI] [PubMed] [Google Scholar]
- 22.Weber M, Lehmann O, Sagesser D, Krause F. Limited open reduction and internal fixation of displaced intra-articular fractures of the calcaneum. J Bone Joint Surg Br. 2008;90:1608–1616. doi: 10.1302/0301-620X.90B12.20638. [DOI] [PubMed] [Google Scholar]
- 23.Abidi NA, Dhawan S, Gruen GS, et al. Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures. Foot Ankle Int. 1998;19:856–861. doi: 10.1177/107110079801901211. [DOI] [PubMed] [Google Scholar]
- 24.Shuler FD, Conti SF, Gruen GS, Abidi NA. Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures: does correction of Bohler's angle alter outcomes? Orthop Clin North Am. 2001;32:187–192. doi: 10.1016/s0030-5898(05)70202-9. x. [DOI] [PubMed] [Google Scholar]
- 25.Freeman BJ, Duff S, Allen PE, et al. The extended lateral approach to the hindfoot. Anatomical basis and surgical implications. J Bone Joint Surg Br. 1998;80:139–142. doi: 10.1302/0301-620x.80b1.7987. [DOI] [PubMed] [Google Scholar]