Abstract
This study evaluates two mechanical properties, tensile strength and tear strength, of maxillofacial materials reinforced with functional polyhedral silsesquioxane (POSS) nanoparticles at 0.0, 0.5, 1.0, 2.0, and 5.0% (mass/mass) loading. Adding POSS was found to significantly affect the overall tensile strength and extensibility of the maxillofacial material. Significant differences were found in mean peak load (p = .050) and extension before failure (p = .050), respectively, between concentrations of 0% and 5%. For tear resistance, a significant difference was observed in mean load (p = .002) between concentrations of 1% and 5%. Significant differences were also observed in extension before failure between concentrations of 0% and 1% (p = .002) and between 0% and 2% (p = .002). Increased resistance to tensile or shearing stresses could lead to greater clinical longevity. The following results suggest that functional nanoparticles can be used to improve properties without compromising clinical handling.
1. Introduction
Silicone elastomers are used in maxillofacial restorations due to their ease of fabrication and realistic appearance.We added the highlighted parts in the addresses. They have properties that are important for human maxillofacial prosthetics such as elasticity, esthetics, heat, and chemical stability [1–3]. When adequately cured, silicone elastomers resist absorbing organic materials that lead to bacterial growth and so with simple cleaning are relatively safe and sanitary compared to other materials [4].
Chemically, maxillofacial materials are formed from the catalyzed reaction between a silane (–SiH) rich polysiloxane component and vinyl (–CH=CH2) rich polysiloxane component [5]. The resulting thermoset is chemically and biologically inert [6]. Toxicological studies have shown silicone materials to have a very low order of toxicity [2]. Studies have shown that such materials are both nontoxic and nonallergenic making them suitable for facial prosthetics [4].
Unfortunately, silicone elastomers have certain deficiencies that reduce the clinical longevity of the prostheses. The main reasons for mechanical failure in maxillofacial prostheses include tensile and tearing loads, respectively [7]. Improving tensile strength and tear strength will lead to longer lasting maxillofacial restoratives. The focus of this work is to determine if the addition of nanoscale reinforcing agents will improve the mechanical properties of maxillofacial materials.
Studies have been done to address the mechanical deficiencies by adding reinforcing agents to the materials. However, reinforcing agents or fillers will increase the rigidity or Young's modulus of a maxillofacial material. Young's modulus is the slope of the elastic region in a stress-strain curve and is conventional referred to as the stiffness of a material. Increasing Young's modulus will decrease the flexibility of the prosthesis and processability of the uncured resin. One such example is the addition of nylon material to the silicone material to make the prostheses more durable [2]. Other materials such as the durable silicone SE-4524U (General Electric, Waterford, NY) have been evaluated and showed a high resistance to tearing. However, this formulation was excessively heavy material and does not readily accept extrinsic coloration [8]. Methacrylated silicones have demonstrated improved peel strength when bonded with a variety of bonding agents [5].
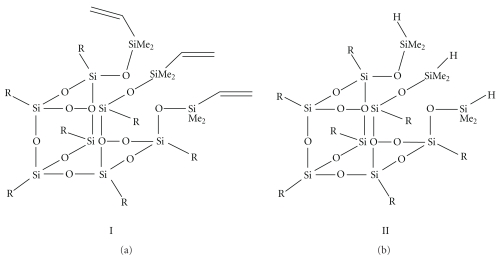
A new approach that has the potential to improve polymeric materials is the use of polyhedralsilsesquioxanes (POSSs) as a reinforcing agent. POSSs are a nanoscale organic-inorganic hybrid (Figure 1) containing a 1.5 nm silica cage with eight pendant organic groups. Recent methodologies have allowed for the large-scale production of POSS materials with functional organic groups such as methacrylate, vinyl, epoxy, and silane [9, 10]. The solubility of a POSS molecule is determined by the organic groups attached to the silica cage. Many POSS molecules are capable of forming homogeneous mixtures with polymeric resins. For example, POSS with mono-, di-, and tri-methacrylate functionalities are commercially available and are soluble in methacrylate-based resin systems such as methyl methacrylate or dental resins.
Figure 1.
POSS materials used in the study. I = trivinyl-POSS and II = trisilane-POSS.
Conceptually, a POSS molecule with polymerizable functionalities could be used to form nanocomposites with a high degree of adhesion between the organic and inorganic phases. Soluble mixtures of POSS and resins behave as if they were a single-phase material. Recent work has shown that POSS materials with pendant methacrylate groups can be used to improve the properties of dental polymer systems used in restorative materials [11]. Other research groups have shown that the addition of POSS to elastomers improves mechanical properties [12–14].
The purpose of this in vitro study is to compare the effect of various concentrations of POSS on the tensile strength and tear resistance of a silicone elastomer used for maxillofacial materials. A tri-vinyl (I) and tri-silane (II) POSS were added to the vinyl rich and silane rich components, respectively, as shown in Table 1. The null hypothesis is that the addition of the POSS will have no effect on the tensile or tear properties of a silicone maxillofacial material.
Table 1.
Composition of experimental samples.
| Sample Label | Modified Part A* | Modified Part B* | ||
|---|---|---|---|---|
| Tris(Dimethylvinyl) | Factor II | Tris(Dimethylsilane) | Factor II | |
| Isobutyl-POSS(I) | A-2000 | IsobutylPOSS(II) | B-2000 | |
| 0.0% POSS | 0.00 g | 45.00 g | 0.00 g | 45.00 g |
| 0.5% POSS | 0.23 g | 44.77 g | 0.23 g | 44.77 g |
| 1.0% POSS | 0.45 g | 44.55 g | 0.45 g | 44.55 g |
| 2.0% POSS | 0.90 g | 44.10 g | 0.90 g | 44.10 g |
| 5.0% POSS | 2.25 g | 42.75 g | 2.25 g | 42.75 g |
*Modified part A is a mixture of vinyl-POSS (I) and Factor II Part A in ratios shown in columns 2 and 3. Modified part B is mixture of silane-POSS (II) and Factor II Part B in ratios shown in columns 4 and 5. Modified Part A and Modified Part B are mixed in a 1 : 1 ratio to give modified maxillofacial materials in concentrations shown in column 1.
2. Material and Methods
2.1. Summary of the Methods
Briefly, trivinyl POSS (I) was mixed with the vinyl rich Factor II, part A and trisilane POSS (II) was mixed with the silane rich Factor II, part B in the appropriate weight ratios. The trivinyl POSS-modified part A, was mixed with the trisilane POSS-modified part B along with thixo and cured in a dumbbell or trousers mold. The tear strength and tensile strength were then evaluated on a universal testing machine. The results were analyzed for statistically significant differences between different loadings of POSS.
2.2. Materials
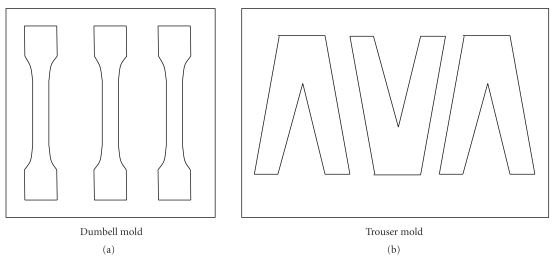
The maxillofacial materials Factor II A-2000 Part A, Factor II A-2000 Part B, and Factor II Thixo were purchased from Factor II (Lakeside, AZ). The Tris(dimethylvinyl) isobutyl-POSS and Tris(dimethylsilane) isobutylPOSS were purchased from Hybrid Plastics (Hattiesburg, MS) and used without further purification. The dumbbell and trouser molds were made from aluminum according to ASTM standards D412 and D624 [15, 16] for the testing of maxillofacial materials (Figure 2).
Figure 2.
sample molds for the dumbell and trouser specimens.
2.3. Formulation of Samples
Table 1 shows the formulation of the POSS modified maxillofacial materials used in the study. The procedure for formulation and mixing is as follows. In a 60 mL cup designed for the speed mixer, Factor II Part A was mixed with the Tris(dimethylvinyl) isobutylPOSS (I, Figure 1) in the ratios described in Table 1 to form modified Part A. This mixture was heated at 55°C for fifteen minutes to promote miscibility. The cup was closed and placed in a SpeedMixer (Hauschild 59075, Hamm, Germany) for 2 minutes at 3000 rpm. The mixture was then cooled in a refrigerator for one hour to prevent spontaneous curing. An identical procedure was used to formulate Factor II Part B with the Tris(dimethylsilane) isobutylPOSS (II, Figure 1) to form modified Part B.
The modified Part A (15 g) and the modified Part B (15 g) were placed in a mixer cartridge with six drops of Factor II Thixo. The cartridge is designed to allow the extrusion of the materials after mixing. The components were then speed mixed for one minute at 1000 rpm and mixed material extruded.
2.4. Fabrication of Samples
The appropriate (dumbbell or trouser) mold (Figure 2) was placed on a thick glass slab and the maxillofacial material was extruded into the mold. Another thick glass slab was placed on top of the mold and was clamped into place. The mold was placed into a preheated oven set at 80°C for 4 hours. After curing, the mold was removed and set aside to allow cooling. When cool, the clamps were removed and the mold was separated.
Once the glass slabs were removed, the samples were carefully removed and labeled. Each sample was checked for defects along the areas that would receive stress during the testing process. Samples that had visible defects were discarded prior to testing. The useable samples were tested using a universal testing machine (Instron Corp. 4204, Canton, MA).
Dumbbell-shaped pieces were attached to the universal testing machine using custom made clamps. The samples were tested until failure at an extension rate of 500 mm/min [17] and the peak load, failure load, and extension were measured. Trouser-shaped samples were tested in a similar manner. The samples were attached to the universal testing machine using the custom made clamps. The samples were tested until failure at an extension rate of 250 mm/min [5]. The tear strength test measured two variables: load at failure, and extension.
2.5. Statistical Analysis
For the tensile strength test, three (3) one-way analysis of variance (ANOVA) procedures were carried out to statistically compare the mean load scores, extensions, and peak loads of the fabricated silicone elastomers across five different concentrations of POSS incorporated in the material (0%, 0.5%, 1%, 2%, and 5%). For the tear resistance test, two (2) one-way analysis of variance (ANOVA) procedures were carried out to statistically compare the mean load scores and extensions of the fabricated silicone elastomers across the same five concentrations of POSS incorporated in the material.
In each case where an ANOVA procedure found an overall significant difference in the means of a particular variable, a post hoc Tukey's multiple comparisons were carried out to identify and rank those particular concentrations of POSS whose mean results were found to be different. All ANOVA tests were conducted at significance level 0.05; Tukey's multiple comparisons were conducted at an overall level of 95% for simultaneous confidence intervals.
3. Results
Results of the experiments are summarized in Tables 2 and 3. The mean load at failure featured a marginally significant difference across the five levels of POSS concentrations at the .05 significance level (p = .050). Tukey's multiple comparison procedure indicated a significant difference (.01 < p < .05) for the pairwise comparison of concentration levels 0% and 5%. The corresponding analysis for mean extension yielded an overall significant difference (p = .039) and a specific significant difference (.01 < p < .05) between concentration levels 0% and 5%. The data for mean peak load indicated an overall significant difference (p = .033) but no significant differences for pairwise comparisons were detected.
Table 2.
Tensile strength of silicone elastomers with various concentrations of POSS.
| % POSS | Sample Size | Mean Failure Load (SD)* (N) | Mean Extension (SD) * (mm) | Mean Peak Load (SD)** (N) |
|---|---|---|---|---|
| 0.0 | 4 | 33.2 (7.0)b,c | 169.9 (26.5)d,e | 167.2 (25.4)g,h |
| 0.5 | 6 | 29.2 (5.0)b | 181.7 (8.8)e | 178.7 (11.9)h |
| 1.0 | 6 | 27.2 (4.0)b | 183.1 (17.1)e | 178.7 (13.5)h |
| 2.0 | 6 | 29.2 (2.5)b | 200.3 (23.3)e | 198.8 (23.3)h |
| 5.0 | 5 | 24.4 (0.6) a,b | 211.0 (26.1)e,f | 206.8 (26.1)h,i |
*Concentration levels with means that are statistically significantly different are given different letters. Means with the same letters were not found to be significantly different. Groups are ranked in alphabetical order from lowest to highest in terms of their means. **The results comparing concentration levels 0.0% and 5.0% are marginally significantly different.
Table 3.
Tear resistance of silicone elastomers with various concentrations of POSS.
| % POSS | Sample Size | Mean Load (SD)* (N) | Extension (SD) * (mm) |
|---|---|---|---|
| 0.0 | 6 | 47.9 (11.1)b,c | 146.2 (13.0)d |
| 0.5 | 5 | 47.2 (6.5)b,c | 173.7 (17.3)de |
| 1.0 | 6 | 50.0 (10.2)c | 194.5 (13.3)e |
| 2.0 | 6 | 35.7 (3.8) a,b | 185.3 (26.1)e |
| 5.0 | 4 | 29.3 (5.0)a | 161.6 (21.3)de |
*Concentration levels with means that are statistically significantly different are given different letters. Means with the same letters were not found to be significantly different. Groups are ranked in alphabetical order from lowest to highest in terms of their means.
Based on these results we reject the null hypothesis that the addition of POSS does not affect mean extension and conclude that there is a difference between the 5% concentration level versus control. We also reject the null hypothesis that the addition of POSS has no effect on the tensile strength properties (although tests were unable to detect specific pairwise differences.) The null hypothesis that POSS has no effect on tear properties of a maxillofacial material was also rejected with differences found between concentration levels 1% and 5%.
4. Discussion
Siloxane polymers are viscoelastic in nature exhibiting properties of both a rigid elastic material and a viscous solid. As shown in Figure 3, the stress-strain curve of viscoelastic materials contains elements of elastic and rubbery materials. Viscoelastic materials have an elastic region characterized by mostly reversible deformation, a yield point, and a rubbery region characterized by mostly permanent deformation, followed by a break or failure point.
Figure 3.
Idealized stress-strain curves for elastic, viscoelastic, and rubbery materials.
Viscoelastic materials can display a wide range of properties. The greater the yield point is, the more resistant a material is to permanent deformation, and a large rubbery region indicates high toughness or the ability to absorb mechanical energy before failure. As stated previously, maxillofacial materials need to able to withstand large instantaneous forces such as tearing and continuous low-level forces from daily use. Clearly, improving the resistance to deformation and increasing toughness would increase clinic longevity.
The addition of filler particles such as POSS to a polymer matrix should result in a stronger, stiffer, less flexible material. This should be characterized by an increase in Young's modulus and yield point but a reduced rubbery plateau region. While maxillofacial materials are strengthened, as measured by mean peak load, by the addition of POSS, there is no statistically significant decrease in the extension at failure. Interestingly, the data suggest that the extension is increased with POSS loading. This effect is not statistically significant in the tensile test though the 1% and 2% samples in the tear test have significantly increased extension compared to control. Maintaining or increasing extension with increased filler loading seems to run contrary to the idea that the addition of fillers will result in a more rigid material. However, it does suggest that POSS may have a plasticizing effect on polymer matrixes. The significant increase in extension prior to failure is also observed in the tear test.
Though the mechanism is not clear, POSS monomers may provide the most significant reinforcement in elastomeric or viscoelastic materials. The work in this paper expands on work by others [12–14] to determine if POSS can be used to reinforce elastomeric maxillofacial materials. Previous work has demonstrated relatively modest gains from POSS reinforcement in stiff or elastic polymers and composites at low levels of loading [11]. However, in the maxillofacial materials we tested that the reinforcing effect is seen in both the elastic and viscoelastic regions of the stress-strain curve and at relatively high levels of loading. The increase in yield strength should provide increased resistance to tearing forces and increase in strain until failure is an indication of toughness, which will increase resistance to forces due to everyday handling.
We also note that while the sample means for the peak load in the tensile test were found to differ among various concentrations of POSS, only one individual pair of means were detected to be different, and only at a very marginal level (concentration level 0% being lower than concentration level 5%). While this result seems paradoxical, it is a well-known statistical result that such a conclusion can occur with small sample sizes and somewhat large variability in the response variable, such as we have here (see columns 2 and 3 of Table 2). This causes a reduction in the power of the statistical test. Further experiments with larger sample sizes would help to clarify the issue. Color stability and long-term environmental stability are also areas that have received significant attention in the literature and will be considered in future work [6, 18–22].
5. Conclusions
POSS monomers have the ability to provide reinforcement to maxillofacial materials and potentially to other elastomeric systems. The POSS loading had a significant effect on the tear and tensile properties of the maxillofacial materials. However the relatively small sample sizes reduced the power of the experiment and the ability to detect differences between groups.
Acknowledgment
The authors would like to thank Mr. Carl Kipp, College of Dentistry, The Ohio State University, for the manufacture of the molds and clamps for the mechanical analysis.
References
- 1.Bellamy K, Limbert G, Waters MG, Middleton J. An elastomeric material for facial prostheses: synthesis, experimental and numerical testing aspects. Biomaterials. 2003;24(27):5061–5066. doi: 10.1016/s0142-9612(03)00412-5. [DOI] [PubMed] [Google Scholar]
- 2.Kanter JC. The use of RTV silicones in maxillofacial prosthetics. The Journal of Prosthetic Dentistry. 1970;24(6):646–653. doi: 10.1016/0022-3913(70)90101-0. [DOI] [PubMed] [Google Scholar]
- 3.Taylor RL, Liauw CM, Maryan C. The effect of resin/crosslinker ratio on the mechanical properties and fungal deterioration of a maxillofacial silicone elastomer. Journal of Materials Science: Materials in Medicine. 2003;14(6):497–502. doi: 10.1023/a:1023451812658. [DOI] [PubMed] [Google Scholar]
- 4.Curtis JM, Colas A. Medical applications of silicones. In: Ratner BD, Hoffman AS, Schoen FJ, Lemons JE, editors. Biomaterials Science: An Introduction to Materials in Medicine. London, UK: Elsevier; 2004. pp. 697–707. [Google Scholar]
- 5.Lai JH, Wang LL, Ko CC, DeLong RL, Hodges JS. New organosilicon maxillofacial prosthetic materials. Dental Materials. 2002;18(3):281–286. doi: 10.1016/s0109-5641(01)00050-1. [DOI] [PubMed] [Google Scholar]
- 6.Eleni PN, Krokida MK, Frangou MJ, Polyzois GL, Maroulis ZB, Marinos-Kouris D. Structural damages of maxillofacial biopolymers under solar aging. Journal of Materials Science: Materials in Medicine. 2007;18(9):1675–1681. doi: 10.1007/s10856-007-3027-4. [DOI] [PubMed] [Google Scholar]
- 7.Udagama A, Drane JB. Use of medical-grade methyl triacetoxy silane crosslinked silicone for facial prostheses. The Journal of Prosthetic Dentistry. 1982;48(1):86–88. doi: 10.1016/0022-3913(82)90052-x. [DOI] [PubMed] [Google Scholar]
- 8.Lewis DH, Castleberry DJ. An assessment of recent advances in external maxillofacial materials. The Journal of Prosthetic Dentistry. 1980;43(4):426–432. doi: 10.1016/0022-3913(80)90215-2. [DOI] [PubMed] [Google Scholar]
- 9.Lichtenhan JD. Polyhedral oligomeric silsesquioxanes: building blocks for silsesquioxane-based polymers and hybrid materials. Comments on Inorganic Chemistry. 1995;17(2):115–130. [Google Scholar]
- 10.Provatas A, Matisons JG. Silsesquioxanes: synthesis and applications. Trends in Polymer Science. 1997;5(10):327–332. [Google Scholar]
- 11.Gao F, Tong Y, Schricker SR, Culbertson BM. Evaluation of neat resins based on methacryplates modified with methacryl-POSS, as potential organic-inorganic hybrids for formulating dental restoratives. Polymers for Advanced Technologies. 2001;12(6):355–360. [Google Scholar]
- 12.Fu BX, Hsiao BS, White H, et al. Nanoscale reinforcement of polyhedral oligomeric silsesquioxane (POSS) in polyurethane elastomer. Polymer International. 2000;49(5):437–440. [Google Scholar]
- 13.Liu L, Tian M, Zhang W, Zhang L, Mark JE. Crystallization and morphology study of polyhedral oligomeric silsesquioxane (POSS)/polysiloxane elastomer composites prepared by melt blending. Polymer. 2007;48(11):3201–3212. [Google Scholar]
- 14.Pan G. Reinforcement of siloxane elastomers with poss based fillers. University of Cincinnati; 2003. M.S. thesis. [Google Scholar]
- 15.A.S.T.M.S. West Conshohocken, Pa, USA: American Society for Testing and Materials; 2006. D412, Standard Test Methods for Vulcanized Rubber and Thermoplastic Elastomers-Tension. [Google Scholar]
- 16.A.S.T.M.S. West Conshohocken, Pa, USA: American Society for Testing and Materials; 2007. D624, Standard Test Method for Tear Strength of Conventional Vulcanized Rubber and Thermoplastic Elastomers. [Google Scholar]
- 17.Dootz ER, Koran A, Craig RG. Physical properties of three maxillofacial materials as a function of accelerated aging. The Journal of Prosthetic Dentistry. 1994;71(4):379–383. doi: 10.1016/0022-3913(94)90098-1. [DOI] [PubMed] [Google Scholar]
- 18.Gary JJ, Huget EF, Powell LD. Accelerated color change in a maxillofacial elastomer with and without pigmentation. Journal of Prosthetic Dentistry. 2001;85(6):614–620. doi: 10.1067/mpr.2001.114683. [DOI] [PubMed] [Google Scholar]
- 19.Kiat-Amnuay S, Johnston DA, Powers JM, Jacob RF. Color stability of dry earth pigmented maxillofacial silicone A-2186 subjected to microwave energy exposure. Journal of Prosthodontics. 2005;14(2):91–96. doi: 10.1111/j.1532-849X.2005.00017.x. [DOI] [PubMed] [Google Scholar]
- 20.Kiat-Amnuay S, Mekayarajjananonth T, Powers JM, Chambers MS, Lemon JC. Interactions of pigments and opacifiers on color stability of MDX4-4210/type A maxillofacial elastomers subjected to artificial aging. Journal of Prosthetic Dentistry. 2006;95(3):249–257. doi: 10.1016/j.prosdent.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 21.Polyzois GL, Tarantili PA, Frangou MJ, Andreopoulos AG. Physical properties of a silicone prosthetic elastomer stored in simulated skin secretions. The Journal of Prosthetic Dentistry. 2000;83(5):572–577. doi: 10.1016/s0022-3913(00)70017-5. [DOI] [PubMed] [Google Scholar]
- 22.Tran NH, Scarbecz M, Gary JJ. In vitro evaluation of color change in maxillofacial elastomer through the use of an ultraviolet light absorber and a hindered amine light stabilizer. Journal of Prosthetic Dentistry. 2004;91(5):483–490. doi: 10.1016/S002239130400112X. [DOI] [PubMed] [Google Scholar]