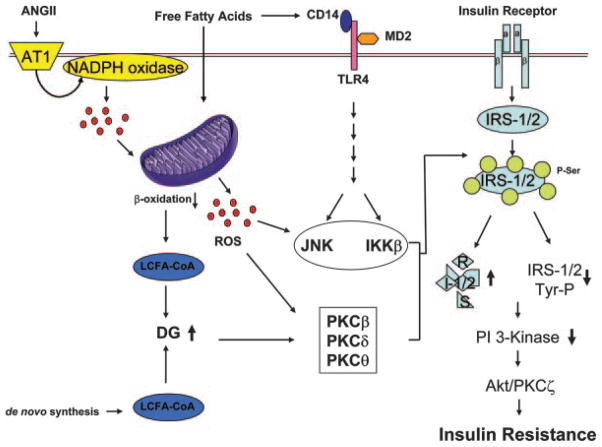
Figure 6.
Proposed molecular mechanism for insulin resistance caused by mitochondrial dysfunction. FFAs activate inflammatory signaling and reduce ATP production that contributes to mitochondrial dysfunction and accumulation of LCFA-CoA and DG. Accumulation of lipid metabolite activates PKCs (β, δ, and θ). ROS produced by NADPH oxidase by angiotensin II causes mitochondrial dysfunction. Conversely, mitochondrial dysfunction increases ROS production, which causes activation of serine/threonine kinases, including IKKβ, JNK, and PKCs, which increases serine phosphorylation of IRS proteins and subsequently results in insulin resistance. Increased serine phosphorylation of IRS-1/2 leads to decreased activity of insulin downstream signaling pathways, including PI3K, Akt, and PKCζ, which culminates in decreased glucose uptake, increased glucose production, and reduced vasodilation and insulin secretion. The reduced insulin responsiveness (insulin resistance) causes diabetes and cardiovascular diseases. PDK-1 indicates 3′-phosphoinositide-dependent protein kinase 1.