When the American Medical Association (AMA) began in 1847, one of its primary intentions was to improve medical education.1 At this time there was disagreement among both educators and practitioners as to how medical doctors should be taught and how diplomas should be granted. Some argued that the course of medical education, which weighed heavily on an apprenticeship model, was too short and needed to be increased. “These resolutions declared a four months college term too short for an adequate course of lectures on all the branches of medical science, and the standard of education, both preliminary and medical, required by the schools previous to the granting of their diplomas, altogether too low; while the union of the teaching and licensing power in the college faculties was represented as impolitic, and constantly liable to abuse.’′1 As well, there was a call for greater standards in the approach to medical education. Davis writes, “The standard of preliminary or preparatory education should be greatly elevated, or, rather, a standard should be fixed, for there is none now, either in theory or in practice.’′1
At this time, medicine had not yet become a science-based profession. The practice of “regular” medicine was based on “…bloodletting, purging, (and) emetics,’′2 medical procedures that are now recognized as causing patients more harm than good.3 Concurrently, there was a movement in America to embrace science as the solution to many problems facing the world.4 This scientific movement would help to drive the medical reform that the Flexner report would later demand.
Thought to have begun in 1895, chiropractic provided a holistic and drugless alternative to the methods that medicine offered to achieve health. It was in 1897 that Daniel David Palmer, chiropractic's founder, first advertised teaching his method of healing. Chiropractic was to be taught at the School of Magnetic Cure “for the purpose of teaching how to get well and keep well without taking poisonous drugs.’′5 In these early years, the term of instruction was 3 months and was based primarily on an apprenticeship method of training. Similar to medicine, after a course of instruction, diplomas were granted confirming that the recipient was trained in chiropractic. At this time, chiropractic was only a fledgling group of practitioners, not a profession. It had no organizational structure and did not have governmental or other external support. In its first 10 years, only a handful of schools were producing chiropractic graduates and an educational curriculum had not yet formally been developed. Though new chiropractic schools sprang up in just a few years, they were primarily proprietary in nature, thus competing against each other instead of collaborating.5 Similar to most medical schools, the chiropractic curricula in the late 1890s were not based in science. Whether or not the chiropractic educators and advocates at the time were aware, chiropractic was heading on a collision course with the reform of organized medicine.
Just before the turn of the century, medical education was still struggling with identity and standardization. Medical schools were in a state of disarray. Medical programs were proprietary in nature with a primary motivation for personal financial gain instead of professional advancement. Standards were still not common among the medical schools and some thought the standards for students to enter the schools were still too low. Science was not included in the medical programs and some were slow to transition away from the traditional methods of purging and bloodletting. Much needed to transpire before medicine would become the juggernaut of the 20th century.
Berliner states that “The institutionalization of scientific medicine began in the United States in 1893 with the opening of the Johns Hopkins Medical School.’′4 By 1901, when the Rockefeller Institute of Medical Research was formed, Johns Hopkins was still the only medical school in the United States that taught students using the scientific method.4 As science was being embraced in medical education, there was a greater focus on the causation of disease. With this transition, unfortunately the concepts of whole-body health and healing began to disappear. Any profession that may have focused on a holistic approach, such as chiropractic, may have been marginalized in this environment. According to Berliner4:
With the new paradigm of scientific medicine, the body began to be conceptualized in terms of systems unrelated to other systems of the body. And although specialization had been present in the context of whole-body medicine, specialization under scientific medicine began to emphasize individual systems or organs to the exclusion of the totality of the body.
The embrace of scientific medicine may have been one of several reasons that medical curricula fractioned the study of medicine into systems and parts instead of honoring the patient as a whole.
In the early 1900s, chiropractic was still attempting to obtain a foothold in its method, cultural acceptance, and approach to education. Some chiropractic schools began to offer correspondence courses, which D.D. Palmer, among others, strongly criticized. In contrast, some other chiropractic programs were lengthening their didactic education and evidence of basic sciences and broadened clinical treatment methods were seen in advertisements for their programs. For example, founded in 1903, the American School of Chiropractic and Nature Cure is credited with developing the first structured curriculum consisting of 4 terms of 5 months each.5 The Palmer College of Chiropractic in Portland, founded in 1908, advertised that it offered 2 years (9 months per year), which included “…minor surgery, obstetrics, forensic jurisprudence, and a full course of dissection.’′5 Although it is not clear how similar these programs were compared to some of the medical schools at the time, the environment in the pre-Flexner report era left many health care programs to govern themselves, since standards were still being developed. Unfortunately, what growth was present in chiropractic education was neither coordinated nor could it keep up with the trends that the medical profession was beginning to address in an organized manner.
Even though the AMA was developing a strong influence in cultural authority in the United States, there was dissatisfaction among the AMA leaders about the state of medical education. In 1904, the AMA created the Council on Medical Education (CME). The CME performed periodic evaluations of medical schools that had minimal consequences. In 1909, the CME published a model medical curriculum.2 The curriculum that they recommended had a total of 4100 hours; 1970 of these were focused on the basic sciences. According to Barzansky and Gevitz,2 although the medical curricula looked similar on paper, “It was in the amount and quality of lab teaching that they differed most markedly.” However, there was not enough impetus to make changes from within the medical profession; thus, the AMA searched for a strong imposing force from the outside to facilitate the change.3, 4
In 1908, the AMA's CME proposed to the Carnegie Foundation a study on medical education with the hopes of gaining greater influence in this process and “to hasten the elimination of medical schools that failed to adopt the CME's standards.’′3 The Carnegie Foundation hired Abraham Flexner, an educational theorist,3 to complete the study. Flexner himself was not medically trained nor was he trained as a researcher; instead he received a bachelor's degree from Johns Hopkins and was thus considered a layman.4 The CME gave Flexner the data that they had been collecting on medical schools prior to his study, which may have biased his report.2 In less than 2 years, Flexner observed 155 institutions of medical education in the United States and Canada and drafted his report. He relied on many documents generated from the AMA and it is not certain how much influence the AMA had in the drafting of the final version of his study.2 In 1910, Abraham Flexner's report, Medical Education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching, was published with the intention of transforming medical education.6 Most would agree that his report accomplished, or at least influenced, this goal.
Flexner's report included harsh evaluations of the majority of medical schools at the time. His comments ranged from criticizing the schools' proprietary nature that generated an overabundance of ill-educated doctors who risked the health of the public, to the lack of adequate training and poor scientific foundation. “Men get in, not because the country needs the doctors, but because the schools need the money" and “…it is idle to talk of1 real laboratory work for students so ignorant and clumsy. Many of them, gotten through advertising, would make better farmers.’′6
Barzansky and Gevitz summarize the seven major recommendations that Flexner included in his report2:
To reduce the number of poorly trained physicians;
To reduce the number of medical schools from 155 to 31 (by the time the report was published schools had already decreased to 131);
To increase the prerequisites to enter medical training;
To train physicians to practice in a scientific manner;
To engage the faculty in research;
To have medical schools control clinical instruction in hospitals; and
To strengthen state regulation of medical licensure.
Flexner's primary emphasis on the structure of a medical curriculum was the first 2 years focusing on basic sciences followed by 2 years of clinical studies. However, other topics were described in the report, including descriptions of what he felt the ideal program should include, discussion of the ethical responsibility of hospitals to focus on patient health instead of doctors' financial prosperity, postgraduate education programs that transform themselves from being tools to fix incompetent doctors to providing advanced education, and the instrumental role of state boards in transforming medical education. The transformation extended to many areas of health care education. Whether these were intended or unintended consequences, most agree that the changes were dramatic.
Barzansky and Gevitz suggest that some have overstated the importance of the Flexner report since medical education reform was progressing even before Flexner's project began.2 Thus, Flexner's report merely helped to consolidate a desired but already occurring process to improve medical education and practice. They suggest that2
His most significant accomplishments were in helping to take away control of hospitals and of medical education, especially clinical education, from the practicing medical profession and to bring it under the authority of academic bureaucracy, and in raising, at least in science subjects, the intellectual and academic requirements for medical school matriculation. Surely these things were going to happen as a consequence of multiple factors already in motion, but Flexner was able to crystallize them, to make them coalesce, to focus them into a recognizable movement with direction and momentum, and to shape the form of clinical education for the years that followed.
The Flexner report seemed to have a substantial impact on medical schools. Within 20 years after the report's publication, the original 131 medical schools from 1910 were reduced to 76, although not 31 as Flexner originally suggested. There was a decrease in graduates but this trend reversed in the following decades (Fig. 1, A and B). After the report, there was an increase in basic sciences and laboratory courses, and increased requirements for students entering school. Entrance requirements also evolved during the first third of the century. In 1904 more than 95% of the medical schools only required a high school education to enter. By 1929, 100% of all medical programs required at least 2 years of college education.2 Although many medical schools closed after the publication of the report, the report was only one of many factors.7 Other factors may have included the AMA's efforts to control health care through political methods and licensing laws.7 State licensing board exams were primarily based on basic sciences and were designed to limit graduates from nonscientific schools from becoming licensed.4, 8 Since licensing boards were controlled by the AMA, exams were designed to discriminate against nonmedical practitioners. This likely had a negative impact on those chiropractic programs that were in the initial stages of development at this time.
Figure 1.
(A) The initial decline but rise of medical students in North America from 1910 to 1930 (adapted from Barzansky and Gevitz2). (B) The decline in the number of medical schools in North America from 1910 to 1930 (adapted from Barzansky and Gevitz2).
The changes occurring after the report not only affected medical education but also the law which governed the practice of medicine and therefore other health care practices. In the early 1900s, the medical practice laws were just beginning to be modified and challenged by the chiropractic profession. As the profession was being persecuted by those in medicine who were trying to protect their field of practice, legal and legislative changes began to evolve that required recognition of the right to practice chiropractic. Oftentimes in order to establish these rights, chiropractic was required to demonstrate that it was a separate and distinct profession from medicine, with the theory that doctors of chiropractic should not be prosecuted for practicing medicine without a license. As well, licensing laws were developed for various health care practices and would incorporate the principles of the Flexner report, such as to include basic science education. These changes in basic science requirements and other criteria would transform chiropractic curricula. Up until these requirements were put into place, many chiropractic programs were underdeveloped. Because of the changes in the licensing boards, due to the Flexner report or other influences, chiropractic schools were pressed to change their curricula in order for their graduates to be licensed in various states.
In 1917, at the Palmer Lyceum, the first efforts were made to standardize chiropractic education.5 This may have been an attempt to address the increasing pressure from licensure laws through the chiropractic institutions. The International Association of Chiropractic Schools and Colleges (IACSC) was formed, with 19 member colleges. One of the purposes of the IACSC was “…to unify and standardize the conceptions of Chiropractic leaders as to what Chiropractic actually is, and to determine what should be conceived to be a standard Chiropractic education…’′5 However, the IACSC did not last long, apparently due to lack of support and interest, though other educational organizations formed in its place in later years.
Though the Flexner report is lauded by some as one of the most important transformational events in medical education in the last century, not all outcomes from this document were necessarily positive. There was a loss of support and a reduced objective view of some of the other health professions (ie, osteopathy, chiropractic, naturopathy) that were developing at the time. Since the study leading up to the report was driven by the AMA, there was an effort to reduce or eliminate the professions that were not aligned with the “regular” medical paradigm. Beck suggests that “The AMA sought to eliminate schools that failed to adopt this rigorous brand of systematized, experiential medical education.’′3 As well, some of the modern negative effects on clinical practice attributed to the Flexner report have included that the standardization of medical education has had a negative effect on family medicine, created medical elitism, and reduced the number of medical doctors wishing to serve in underserved areas.3 These are areas that the medical profession still struggles to address.
Movement toward an emphasis on basic sciences demonstrated that medicine was embracing science as its foundation instead of the earlier dogma of bleeding and purging. The disciplines of “pathology, bacteriology, and clinical microscopy” were considered bases for the scientific method, and therefore were emphasized in the new medical curricula. The drive for scientific instead of dogmatic methods was a primary theme running through the Flexner report. However, by 1925 there was new criticism of the developing medical curricula; it was observed that the basic sciences were not being taught in a clinically relevant manner. The complaint included that there was too much emphasis on details that had little or no clinical relevance.2 As well, there was criticism that basic and clinical courses were taught in isolation without much integration into the rest of the curriculum.2 It seems that the Flexner report helped to bring the basic sciences into medical education but it was not able to suggest effective methods by which they should be taught. As medical education still struggles with this predicament, the other health professions influenced by Flexner, such as chiropractic, have suffered the same fate.
Although only medical schools were included in Flexner's study, chiropractic was briefly mentioned in a section of the report discussing medical sects. “The chiropractics, the mechano-therapists, and several others are not medical sectarians, though exceedingly desirous of masquerading as such; they are unconscionable quacks, whose printed advertisements are tissues of exaggeration, pretense, and misrepresentation of the most unqualifiedly mercenary character.’′6 It was apparent that Flexner was not in support of chiropractic or other health care professions and was positioning medicine to be at the center of the health care model. Thus, it would be up to the chiropractic profession to improve its own educational programs without the financial support from external entities such as the Carnegie Foundation.
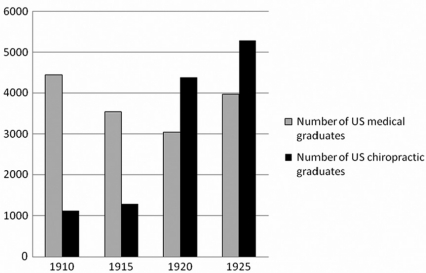
One agent for change in chiropractic education, John J. Nugent, DC, followed Flexner's example beginning in 1935. After the Flexner report, new chiropractic colleges continued to open and produce graduates in an unchecked environment (Fig. 2). Liberally borrowing from Flexner's concepts of educational reform, Nugent, the first Director of Education for the National Chiropractic Association (NCA),9 reported to the NCA in 1950 that its Council on Education had been constructed in chiropractic by following the structure of other professional accrediting bodies and remarked on “the close parallel of the pattern which we used in building our schools to that followed by Dr. Abraham Flexner in building the medical schools.”
Figure 2.
A comparison of the number of medical versus chiropractic graduates in the years after the Flexner report based on data from Barzansky and Gevitz2 and Keating et al.5 If these numbers are accurate, it is a possible reason why organized medicine may have felt threatened.
Based on his personal inspections of chiropractic schools of the time, Nugent led efforts to reduce the number of for-profit chiropractic schools into fewer not-for-profit colleges with higher entrance standards and standardized curricula.10 Similar to Flexner's report, Nugent's message included merging smaller schools, enhancing and standardizing the curricula, making all schools nonprofit, and improving facilities and clinical education. This did not make Nugent a popular man in the chiropractic profession. However, Nugent personally oversaw the negotiations culminating in the reduction of 51 private schools considered to be of inferior quality to 8 NCA-approved nonprofit colleges.9 Nugent was successful in his attempts at early chiropractic educational reform.
The standard medical education format that chiropractic colleges mimicked in their early years, and for the most part continue to do so, includes the first years focusing on basic sciences (anatomy, physiology, pathology, etc) and the later years focusing on clinical topics (diagnosis, clinical practice methods). It is interesting to note that a study comparing chiropractic and medical education in the mid-1990s showed strong similarities in medical and chiropractic education based on number of hours and subjects taught, such as hours of course work in basic science and clinical courses.11 Coulter et al.11 concluded that
Considerable commonality exists between chiropractic and medical programs. Regarding the basic sciences, these programs are more similar than dissimilar, both in the types of subjects offered and in the time allotted to each subject. The programs also share some common areas in the clinical sciences.
So if one of the original reasons for the Flexner report's basic science requirement was meant to eliminate other professions, it appears not to have done so in the case of chiropractic.
Though Flexner's report influenced chiropractic, we unfortunately seem to be stuck in an educational model that in 1910 was meant to transform medical education from dogma to science. Being stuck in such a model, we are burdened with outdated requirements and we struggle to focus our curricula on what is most important: clinical competencies and how we can best produce ideal chiropractic healers. For education in general, there continues to be too much focus on the number of hours our students are sitting warming seats in the classroom and the tallies of topical content (eg, memorization of facts unrelated to clinical practice), which may no longer be relevant to modern-day practice. Instead we should be considering if our students have mastered the knowledge, skills, and attitudes that are required to deliver safe and effective chiropractic health care.
For the first half of the 20th century, this Flexner-influenced educational model seemed to do well to support medical knowledge and skills, which were considerably more limited compared to today's standards. Back in the 1930s and 1940s, the knowledge base was much smaller; antibiotics were just being discovered, diagnostic imaging was in its infancy, and surgical techniques were focusing on gross methods of saving lives instead of the finesse we see in today's operating theaters. However, as medical science and practice methods have grown, little evolution has occurred within medical education to parallel these changes. The old model of basic sciences and clinical sciences was engrained so deeply that it has been a herculean effort to make even small changes in the whole of medical education. A greater focus is now being taken in medical education and national associations to recognize that medical education should be more aligned with current learning theories and methods and better match the knowledge, skills, and attitudes that medical practitioners should achieve in order to practice safely and successfully.12 The Carnegie Foundation has published its follow-up to the original Flexner report, Educating Physicians: A Call for Reform of Medical School and Residency (http://www.carnegiefoundation.org), which states that “Fundamental change in medical education will require new curricula, new pedagogies and new forms of assessment.” The report suggests that continued reform should include standardization of learning outcomes and assessment of competencies over time; promotion of learners' ability to work collaboratively with other health professionals; inclusion of formal instruction in ethics and reflective practice; development of a spirit of inquiry as individuals and in health care teams; and to be more intentional about selection and development of medical educators.
It is praiseworthy that the medical profession is working toward evolving their educational approach. At the moment, it seems that there are few efforts in chiropractic education on a profession-wide level to revisit the core curriculum and ascertain where there is need for improvement based on the needs of the 21st century. Although there has been an increase in data-based studies in the past decade13 and some efforts at curriculum reform at a few chiropractic colleges, no great efforts have transpired to move the profession as a whole beyond the traditional curriculum format that Flexner proposed in 1910 and Nugent championed later in chiropractic. It may be that our infrastructure, like medicine, is so burdened by this antiquated format that it is difficult to transcend it. For example, the National Board of Chiropractic Examiners (NBCE) exams are currently structured so that chiropractic students must take NBCE part I (ie, basic sciences) prior to taking part II and III (ie, clinical sciences). Because NBCE certification is required to practice in the United States, this tends to limit how a chiropractic college may improve its curriculum. If a chiropractic college wished to deliver a curriculum in a modular or integrated manner (eg, musculoskeletal system would be taught with the combination of anatomy and physiology, in addition to diagnosis and management and clinical application), this would delay students from being allowed to sit for the NBCE part I exam until very late in their curriculum. Thus, changing only delivery or how many hours are dedicated to a particular topic is likely not enough to transform chiropractic education.
Most of the standards for health care and health care education from 1910 no longer apply to our current situation in 2010. The methods of diagnosis and treatment that have evolved and the health care infrastructure are dramatically different than 100 years ago. As well, education has transformed. It is recognized that sitting in a classroom taking didactic lecture for 6 months, or for any length of time, is not necessarily effective. It is likely that Flexner's report was intended for its time and not to transcend beyond its original purpose, which was to transform medical education and eliminate schools that were not science based. We should revere his efforts to improve health care education, and for the positive influence on the chiropractic profession, but not carve the outdated concepts in stone at the expense of what we currently know about best practices in education and health care. We must rise above the standard old models of medical curricula and prepare to meet the needs of our current learners and the future health care environment.
As chiropractic continues to evolve as a profession, our educational foundation must evolve as well, not only in content, but in methods of delivery. We should consider both the challenges and benefits of abandoning an antiquated system and plan to develop a new system that better serves our students and our patients. We should not wait for an external force to influence our destiny, but instead collaborate to improve chiropractic education for our next 100 years.
Conflict of Interest
No funding was received for writing this article.
References
- 1.Davis NS. In: History of the American Medical Association from its organization up to January 1855. Butler SW, editor. Philadelphia: Lippincott, Grambo and Co; 1855. [Google Scholar]
- 2.Barzansky B, Gevitz N. Beyond Flexner: medical education in the twentieth century. Westport: Greenwood Press; 1992. [Google Scholar]
- 3.Beck AH. The Flexner report and the standardization of American medical education. JAMA. 2004;291(17):2139–40. doi: 10.1001/jama.291.17.2139. [DOI] [PubMed] [Google Scholar]
- 4.Berliner HS. A larger perspective on the Flexner report. Int J Health Serv. 1975;5(4):573–92. doi: 10.2190/F31Q-592N-056K-VETL. [DOI] [PubMed] [Google Scholar]
- 5.Keating JC, Callender AK, Cleveland CS. A history of chiropractic education in North America. Davenport: Association for the History of Chiropractic; 1998. p. 151. [Google Scholar]
- 6.Flexner A. Bulletin 4. New York: Carnegie Foundation for the Advancement of Teaching; 1910. Medical education in the United States and Canada: a report to the Carnegie Foundation for the advancement of teaching. [PMC free article] [PubMed] [Google Scholar]
- 7.Banta D. Medical education: Abraham Flexner—a reappraisal. Soc Sci Med. 1971;87:655–61. doi: 10.1016/0037-7856(71)90015-1. [DOI] [PubMed] [Google Scholar]
- 8.Gevitz N. “A coarse sieve”: basic science boards and medical licensure in the United States. J Hist Med Allied Sci. 1988;43(1):36–63. doi: 10.1093/jhmas/43.1.36. [DOI] [PubMed] [Google Scholar]
- 9.Wardwell WI. Chiropractic: history and evolution of a new profession. St. Louis: Mosby Year Book; 1992. pp. 141–3. [Google Scholar]
- 10.Gibbons RW. Chiropractic's Abraham Flexner: the lonely journey of John J. Nugent, 1935–1963. Chiropr Hist. 1985;5:44–51. [PubMed] [Google Scholar]
- 11.Coulter I, Adams A, Coggan P, Wilkes M, Gonyea M. A comparative study of chiropractic and medical education. Altern Ther Health Med. 1998;4(5):64–75. [PubMed] [Google Scholar]
- 12.Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education 100 years after the Flexner report. N Engl J Med. 2006;355(13):1339–44. doi: 10.1056/NEJMra055445. [DOI] [PubMed] [Google Scholar]
- 13.Johnson CD, Green BN. Trends in articles published over the past 20 years in The Journal of Chiropractic Education: country of origin, academic affiliation, and data versus nondata studies. J Chiropr Educ. 2008;22(1):4–11. doi: 10.7899/1042-5055-22.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]