Abstract
Bedside ultrasound interrogation of the thorax can aide the clinician in determining the cause of the respiratory dysfunction. Often plain radiographs are not sufficient to differentiate pathology. We present a case in which bedside ultrasound defined the pathology without the need for further imaging.
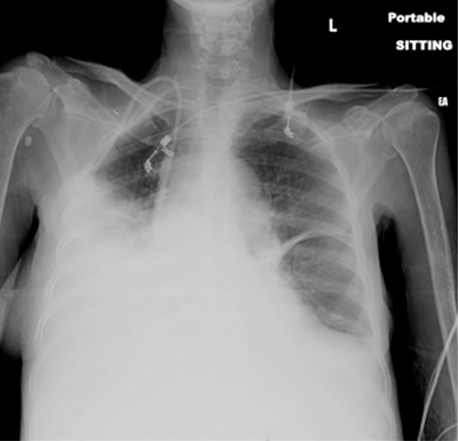
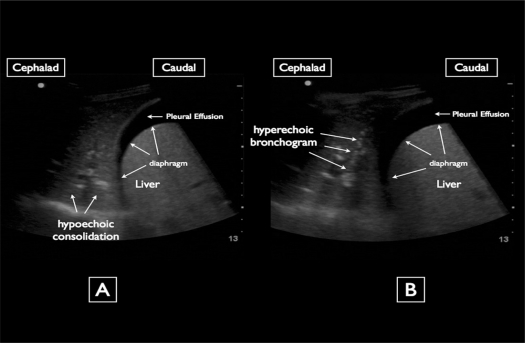
A 60-year-old female with a history of esophageal cancer, status-post radiation and chemotherapy, was transferred from a skilled nursing facility to the emergency department for shortness of breath. On exam, the patient was found to be cachectic and have oxygen desaturations to the mid 80s with minimal movement, bilateral rhonchi, and an ascitic abdomen. A portable chest radiograph (Figure 1) was officially read as bilateral pleural effusions, which were greater on the right side than the left. Ultrasounds of the right lower thorax (Figure 2 A and B) are shown above.
Figure 1.
Portable upright chest radiograph reveals bilateral pleural effusion.
Figure 2.
A) Ultrasound of the right lower thorax. B) Ultrasound of the right lower thorax.
When a chest radiograph shows an opaque hemithorax, ultrasound of the thorax can be useful for deciphering the underlying etiology and morphology.1, 2 Sonographically normal lung is identified by sliding at the pleural-pulmonary interface and reverberation and comet tail artifacts produced by the air inside the lungs.3 Compared to normal lung, consolidation on ultrasound has a relatively hypoechoic heterogeneous echotexture.2 Because consolidation appears isoechoic with the liver it has been referred to as lung “hepatization.” The margin around the consolidation as it abuts normal aerated lung is blurred and irregular. Consolidation on ultrasound also contains air bronchograms analogous to air bronchograms seen on chest radiograph. Sonographic air bronchograms appear as multiple hyperechoic millimeter-long, lentil-shaped air inlets or as hyperechoic branching tubular structures within the consolidated lung parenchyma.2,4 A moderate amount of literature exists detailing the utility of ultrasound for the detection of pulmonary consolidation, with ultrasound demonstrating a higher level of sensitivity than both auscultation and chest radiography.3,5
On ultrasound, atalectasis also contains air bronchograms and can look similar to consolidation. However, air bronchograms in atalectasis look more crowded and parallel to one another.5 Atalectasis also tends to appear biconcave and be found floating in a large pleural effusion.2 Pleural effusions on ultrasound appear as anechoic or hypoechoic areas between the visceral and parietal pleura.4
In this case, the ultrasound revealed that the opaque hemithorax on chest radiograph was not a large pleural effusion necessitating thoracentesis, but instead a large area of consolidation with a concomitant small effusion. Empiric antibiotic therapy was immediately initiated, and further imaging was cancelled.
Footnotes
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENES
- 1.Yu CJ, Yang PC, et al. Ultrasound study in unilateral hemithorax opacification: image comparison with computed tomography. Am Rev Respir Dis. 1993;147:430–434. doi: 10.1164/ajrccm/147.2.430. [DOI] [PubMed] [Google Scholar]
- 2.Gehmacher O, Mathis G, et al. Ultrasound imaging of pneumonia. Ultrasound in Med & Biol. 1995;21:1119–1122. doi: 10.1016/0301-5629(95)02003-9. [DOI] [PubMed] [Google Scholar]
- 3.Lichtenstein D, Goldstein I, et al. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004 Jan;100(1):9–15. doi: 10.1097/00000542-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Reissig A, Kroegel C. Sonographic diagnosis and follow-up of pneumonia: a prospective study. Respiration. 2007;74:537–547. doi: 10.1159/000100427. [DOI] [PubMed] [Google Scholar]
- 5.Parlamento S, Copetti R, Di Bartolomeo S. Evaluation of lung ultrasound for the diagnosis of pneumonia in the ED. Am J Emerg Med. 2009 May;27(4):379–384. doi: 10.1016/j.ajem.2008.03.009. [DOI] [PubMed] [Google Scholar]