Abstract
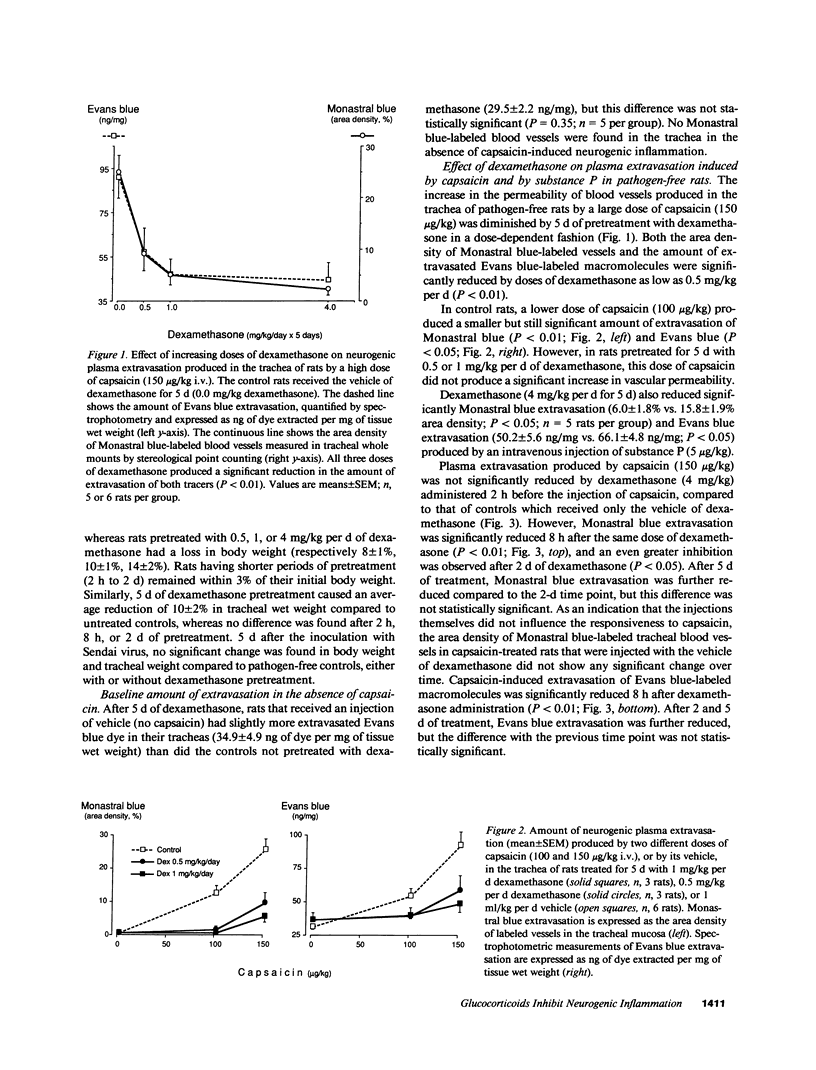
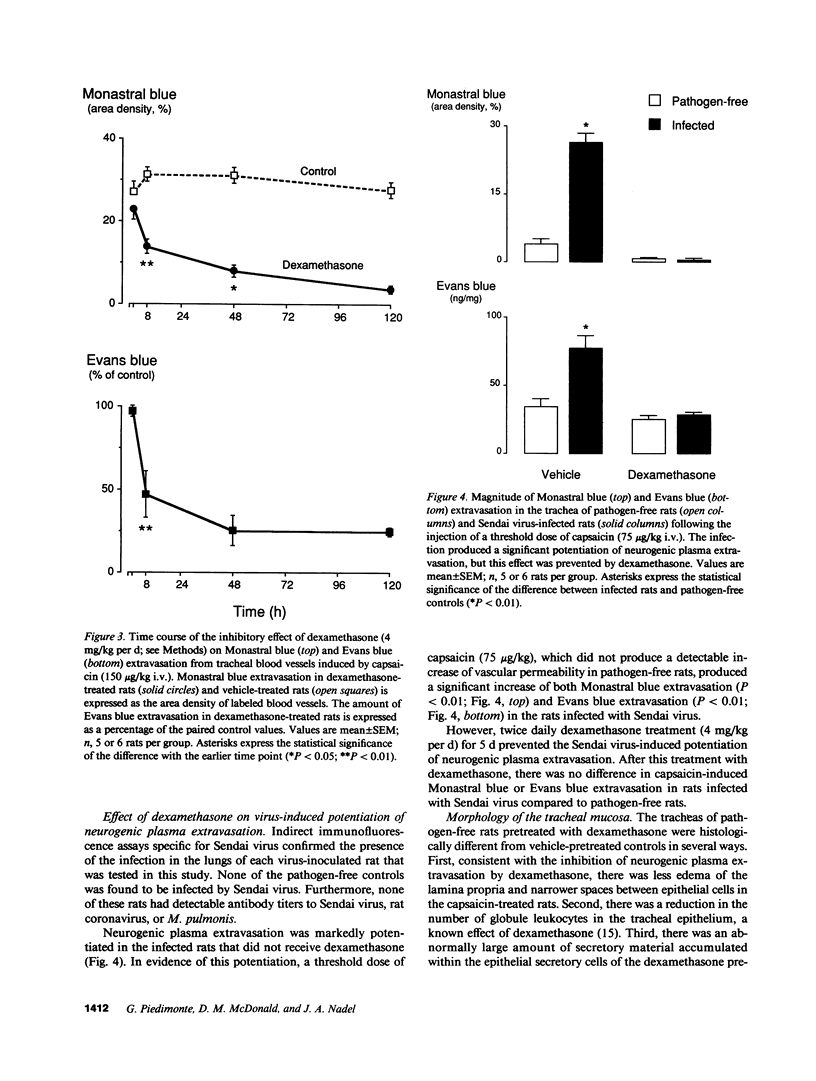
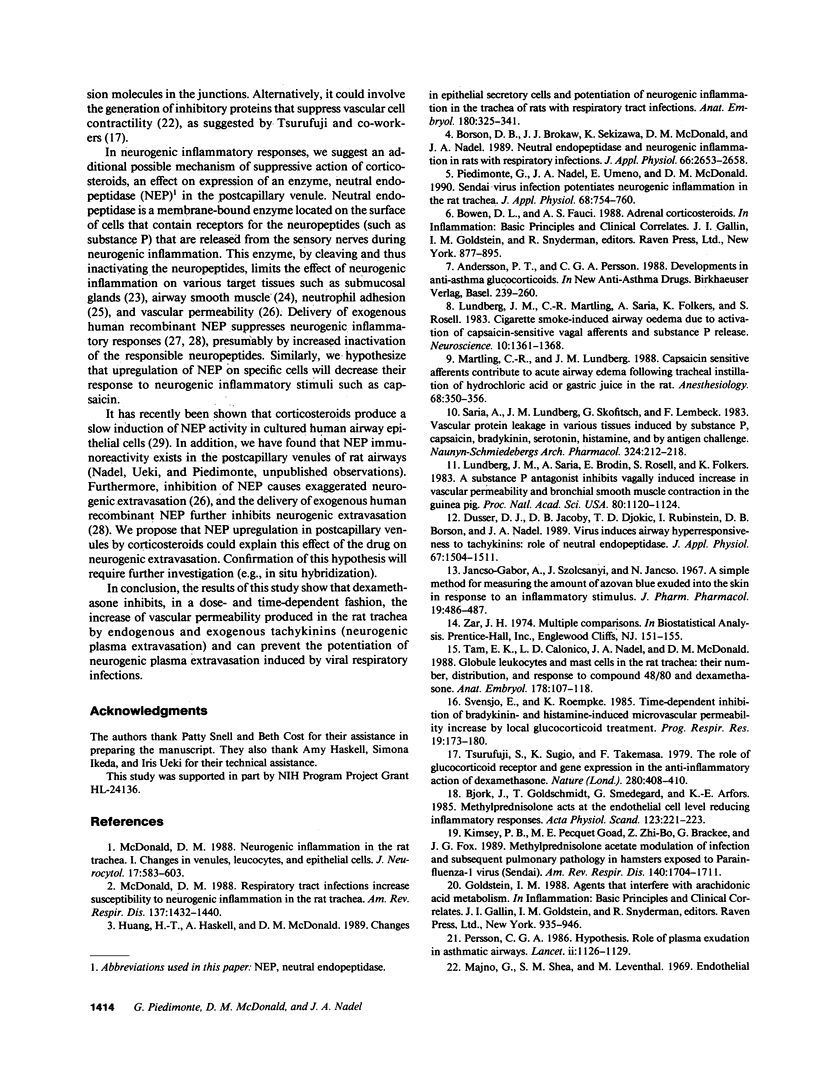
Capsaicin increases the permeability of blood vessels in the rat tracheal mucosa through a mechanism involving the release of tachykinins from sensory nerves. This capsaicin-induced increase in vascular permeability is potentiated by viral infections of the respiratory tract. The present study was done to determine whether this "neurogenic plasma extravasation" can be inhibited by glucocorticoids, to learn the time course of this inhibition, and to determine whether glucocorticoids can prevent the potentiating effect of viral respiratory infections on neurogenic plasma extravasation. Groups of pathogen-free F344 rats were treated with dexamethasone for 2 or 8 h (4 mg/kg i.p.) or 48 or 120 h (0.5-4 mg/kg per d i.p.). Another group of rats was treated with dexamethasone for 120 h following the intranasal inoculation of Sendai virus. The magnitude of plasma extravasation produced by capsaicin or substance P was assessed after this treatment by using Monastral blue pigment and Evans blue dye as intravascular tracers. We found that dexamethasone reduced, in a dose-dependent fashion, the magnitude of plasma extravasation produced in the rat trachea by capsaicin and substance P. Significant inhibition was produced by a dose of dexamethasone as small as 0.5 mg/kg i.p. The effect of dexamethasone had a latency of several hours and reached a maximum after 2 d of treatment. Furthermore, dexamethasone prevented the potentiation of neurogenic plasma extravasation usually present after 5 d of Sendai virus respiratory infection.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andersson P. T., Persson C. G. Developments in anti-asthma glucocorticoids. Agents Actions Suppl. 1988;23:239–260. doi: 10.1007/978-3-0348-9156-1_18. [DOI] [PubMed] [Google Scholar]
- Björk J., Goldschmidt T., Smedegård G., Arfors K. E. Methylprednisolone acts at the endothelial cell level reducing inflammatory responses. Acta Physiol Scand. 1985 Feb;123(2):221–224. doi: 10.1111/j.1748-1716.1985.tb07581.x. [DOI] [PubMed] [Google Scholar]
- Borson D. B., Brokaw J. J., Sekizawa K., McDonald D. M., Nadel J. A. Neutral endopeptidase and neurogenic inflammation in rats with respiratory infections. J Appl Physiol (1985) 1989 Jun;66(6):2653–2658. doi: 10.1152/jappl.1989.66.6.2653. [DOI] [PubMed] [Google Scholar]
- Borson D. B., Corrales R., Varsano S., Gold M., Viro N., Caughey G., Ramachandran J., Nadel J. A. Enkephalinase inhibitors potentiate substance P-induced secretion of 35SO4-macromolecules from ferret trachea. Exp Lung Res. 1987;12(1):21–36. doi: 10.3109/01902148709068812. [DOI] [PubMed] [Google Scholar]
- Dusser D. J., Jacoby D. B., Djokic T. D., Rubinstein I., Borson D. B., Nadel J. A. Virus induces airway hyperresponsiveness to tachykinins: role of neutral endopeptidase. J Appl Physiol (1985) 1989 Oct;67(4):1504–1511. doi: 10.1152/jappl.1989.67.4.1504. [DOI] [PubMed] [Google Scholar]
- Huang H. T., Haskell A., McDonald D. M. Changes in epithelial secretory cells and potentiation of neurogenic inflammation in the trachea of rats with respiratory tract infections. Anat Embryol (Berl) 1989;180(4):325–341. doi: 10.1007/BF00311165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jancso-Gabor A., Szolcsanyi J., Jansco N. A simple method for measuring the amount of azovan blue exuded into the skin in response to an inflammatory stimulus. J Pharm Pharmacol. 1967 Jul;19(7):486–487. doi: 10.1111/j.2042-7158.1967.tb08119.x. [DOI] [PubMed] [Google Scholar]
- Kimsey P. B., Goad M. E., Zhao Z. B., Brackee G., Fox J. G. Methyl prednisolone acetate modulation of infection and subsequent pulmonary pathology in hamsters exposed to parainfluenza-1 virus (Sendai). Am Rev Respir Dis. 1989 Dec;140(6):1704–1711. doi: 10.1164/ajrccm/140.6.1704. [DOI] [PubMed] [Google Scholar]
- Kohrogi H., Nadel J. A., Malfroy B., Gorman C., Bridenbaugh R., Patton J. S., Borson D. B. Recombinant human enkephalinase (neutral endopeptidase) prevents cough induced by tachykinins in awake guinea pigs. J Clin Invest. 1989 Sep;84(3):781–786. doi: 10.1172/JCI114236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundberg J. M., Martling C. R., Saria A., Folkers K., Rosell S. Cigarette smoke-induced airway oedema due to activation of capsaicin-sensitive vagal afferents and substance P release. Neuroscience. 1983 Dec;10(4):1361–1368. doi: 10.1016/0306-4522(83)90117-3. [DOI] [PubMed] [Google Scholar]
- Lundberg J. M., Saria A., Brodin E., Rosell S., Folkers K. A substance P antagonist inhibits vagally induced increase in vascular permeability and bronchial smooth muscle contraction in the guinea pig. Proc Natl Acad Sci U S A. 1983 Feb;80(4):1120–1124. doi: 10.1073/pnas.80.4.1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majno G., Shea S. M., Leventhal M. Endothelial contraction induced by histamine-type mediators: an electron microscopic study. J Cell Biol. 1969 Sep;42(3):647–672. doi: 10.1083/jcb.42.3.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martling C. R., Lundberg J. M. Capsaicin sensitive afferents contribute to acute airway edema following tracheal instillation of hydrochloric acid or gastric juice in the rat. Anesthesiology. 1988 Mar;68(3):350–356. doi: 10.1097/00000542-198803000-00005. [DOI] [PubMed] [Google Scholar]
- McDonald D. M. Neurogenic inflammation in the rat trachea. I. Changes in venules, leucocytes and epithelial cells. J Neurocytol. 1988 Oct;17(5):583–603. doi: 10.1007/BF01260988. [DOI] [PubMed] [Google Scholar]
- McDonald D. M. Respiratory tract infections increase susceptibility to neurogenic inflammation in the rat trachea. Am Rev Respir Dis. 1988 Jun;137(6):1432–1440. doi: 10.1164/ajrccm/137.6.1432. [DOI] [PubMed] [Google Scholar]
- Persson C. G. Role of plasma exudation in asthmatic airways. Lancet. 1986 Nov 15;2(8516):1126–1129. doi: 10.1016/s0140-6736(86)90533-7. [DOI] [PubMed] [Google Scholar]
- Piedimonte G., Nadel J. A., Umeno E., McDonald D. M. Sendai virus infection potentiates neurogenic inflammation in the rat trachea. J Appl Physiol (1985) 1990 Feb;68(2):754–760. doi: 10.1152/jappl.1990.68.2.754. [DOI] [PubMed] [Google Scholar]
- Rubinstein I., Iwamoto I., Ueki I. F., Borson D. B., Nadel J. A. Recombinant neutral endopeptidase attenuates substance P-induced plasma extravasation in the guinea pig skin. Int Arch Allergy Appl Immunol. 1990;91(3):232–238. doi: 10.1159/000235122. [DOI] [PubMed] [Google Scholar]
- Saria A., Lundberg J. M., Skofitsch G., Lembeck F. Vascular protein linkage in various tissue induced by substance P, capsaicin, bradykinin, serotonin, histamine and by antigen challenge. Naunyn Schmiedebergs Arch Pharmacol. 1983 Nov;324(3):212–218. doi: 10.1007/BF00503897. [DOI] [PubMed] [Google Scholar]
- Sekizawa K., Tamaoki J., Graf P. D., Basbaum C. B., Borson D. B., Nadel J. A. Enkephalinase inhibitor potentiates mammalian tachykinin-induced contraction in ferret trachea. J Pharmacol Exp Ther. 1987 Dec;243(3):1211–1217. [PubMed] [Google Scholar]
- Tam E. K., Calonico L. D., Nadel J. A., McDonald D. M. Globule leukocytes and mast cells in the rat trachea: their number, distribution, and response to compound 48/80 and dexamethasone. Anat Embryol (Berl) 1988;178(2):107–118. doi: 10.1007/BF02463644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsurufuji S., Sugio K., Takemasa F. The role of glucocorticoid receptor and gene expression in the anti-inflammatory action of dexamethasone. Nature. 1979 Aug 2;280(5721):408–410. doi: 10.1038/280408a0. [DOI] [PubMed] [Google Scholar]
- Umeno E., Nadel J. A., Huang H. T., McDonald D. M. Inhibition of neutral endopeptidase potentiates neurogenic inflammation in the rat trachea. J Appl Physiol (1985) 1989 Jun;66(6):2647–2652. doi: 10.1152/jappl.1989.66.6.2647. [DOI] [PubMed] [Google Scholar]


