Abstract
Pain secondary to instability in total knee arthroplasty (TKA) has been shown to be major cause of early failure. In this study, we focused on the effect of instability in TKA on the proximal tibiofibular joint (PTFJ). We used a robotics model to compare the biomechanics of the PTFJ in the native knee, an appropriately balanced TKA, and an unbalanced TKA. The tibia (n=5) was mounted to a six-degree of freedom force/torque sensor and the femur was moved by a robotic manipulator. Motion at the PTFJ was recorded with a high resolution digital camera system. After establishing a neutral position, loading conditions were applied at varying flexion angles (0, 30, and 60°). These included: internal/external rotation (0 Nm, ± 5 Nm), varus/valgus (0 Nm, ± 10 Nm), compression (100 N, 700 N), and posterior drawer (0 N, 100 N). With respect to anterior displacement, external rotation had the largest effect (coefficient = 0.650; p < 0.0001). Polyethylene size as well as the interaction between polyethylene size and flexion consistently showed substantial anterior motion. Flexion and mid-flexion instability in TKA have been difficult to quantify. While tibiofemoral kinematics is the main aspect of TKA performance, the effects on adjacent tissues should not be overlooked. Our data show that PTFJ kinematics are affected by the balancing of the TKA.
Keywords: proximal tibio-fibular joint, total knee arthroplasty, kinematics, instability
Introduction
Total knee replacement is one of the most efficacious interventions available for the improvement of general health related quality of life. This success has made the procedure one of the fastest growing practices in the United States with estimates of growth approaching 600% by the year 20301. Recently, more attention has focused on the failures of total knee replacement with great concentration on improving joint kinematics, range of motion, and function and quality of life2.
A higher percentage of arthroplasty patients describe significant limitations in function compared to age and gender matched peers3. Pain and instability in total knee arthroplasty (TKA) have been shown to be major causes of early failure2, 4. One cause of what has previously been described as “unexplained pain” is now believed to be pain secondary to instability of the TKA5, 6. Instability may generate abnormal mechanical stress in the anatomic tissues potentially causing pain, and also requires muscles and tendons to dynamically stabilize a knee that is not able to be statically stabilized through proper tension throughout the arc of motion in the periarticular soft tissues. Here we focus on the effect of instability in TKA on the proximal tibiofibular joint (PTFJ) and introduce a surrogate model to quantify instability in TKA.
The PTFJ is an articulation located in the posterolateral corner of the knee which serves as the attachment site for many structures that function in stabilizing the joint. These structures include the lateral collateral ligament, the fabellofemoral ligament, the arcuate ligament, the popliteofibular ligament, the popliteus muscle, and the biceps femoris tendon insertion. Lambert7 suggested that the fibula may be a channel for dissipation of torsional stresses in the ankle. We believe that the fibula has a similar role in the knee joint, acting as a shock absorber for excessive stresses and playing an integral role in maintaining stability through its soft tissue attachments.
Previous studies of the PTFJ have focused little attention on its role in overall knee joint mechanics. We have studied the motion of the fibula in relation to the tibia in the native knee using a manual loading system8. In this study, several millimeters of translational motion (1-3 mm) were observed mainly during rotational and varus loading, corresponding to common physiologic motions (i.e., gait, stair climbing)8. These anteroposterior movements observed were large considering the relatively small size of the PTFJ (less than 10 mm), and may account for substantial soft tissue strain in the surrounding tissues ultimately resulting in pain.
The objective of this study was to use robotic testing to define the biomechanics of the PTFJ in the native knee, and compared it with the motion of the PTFJ in an appropriately balanced TKA and unbalanced TKA. We hypothesize that normal motion of the fibula in relation to the tibia is a reproducible finding in properly balanced TKA when compared to the native knee, but abnormal kinematics would be found in an improperly balanced TKA.
Methods
Five fresh frozen serologically tested cadaveric lower limb specimens (mid femur to ankle) were tested with knee and syndesmosis intact. The specimens were thawed overnight and under went testing the following morning. The tibia was mounted vertically to a custom designed fixator with three bicortical cannulated bone screws and then fixed to a six degree of freedom force/torque sensor (SI-1500-240, ATI Industrial Automation, Apex, NC) mounted rigidly to a crossbeam. The femur was cut 10 cm proximal to the joint line, potted in Woods metal, and placed in a custom mount on a robotic manipulator (Rotopod R2000, Parallel Robotics System, Hampton, NH) (Figure 1). Two markers were implanted on the tibia and head of the fibula at the PTFJ and motion was recorded using two high resolution digital camera systems similar to what we have described in a previous publication8 (Scorpion IEEE-1394, Point Grey Research Inc., Vancouver, BC).
Figure 1.

Specimen mounted to robotic manipulator.
A knee joint coordinate system was established using a MicroScribe coordinate measuring machine (Immersion Corporation, San Jose, CA). After establishing a neutral position (position of knee with 0 forces or moments) at each of three flexion angles (0, 30, 60 degrees), loading conditions were applied: internal/external rotation (0 Nm, ± 5 Nm), varus/valgus (0 Nm, ± 10 Nm), compression (100 N, 700 N), and posterior drawer (0 N, 100 N), resulting in 108 test combinations of loading conditions. Three dimensional forces were load controlled using proportional-integral-derivative control of the robot motion to achieve force target while recording changes in the knee kinematics.
Specimens were initially tested in their native state. A medial parapatellar arthrotomy was performed and anatomically repaired to control for its possible effects on subsequent testing of specimens following TKA. The specimens were taken through an initial run of the protocol prior to data collection, to allow for tissue creep. Specimens were frequently sprayed with saline solution to help preserve soft tissue integrity.
A TKA was then performed on each specimen by an orthopaedic surgeon using a Triathlon total knee (Stryker Orthopaedics, Mahwah, NJ). A tensiometer was used to achieve a well-balanced knee. In order to allow for subsequent decreases in polyethylene thickness to test an increasing pattern of TKA instability, the tibia was resected until a 13 mm polyethylene insert (at a minimum) was needed to appropriately balance the knee. The epicondylar axis was used to establish appropriate femoral component rotation. Components were cemented in the usual fashion and the patella was not resurfaced. All surgeries were performed by the same surgeon (HHL).
Once implanted, the specimens were tested in one of three states, well balanced and two conditions of varying laxity created by sequential 2-3 mm reductions in polyethylene thickness. Testing was carried out in a randomly selected order to minimize any bias from order effects.
The video data were digitized and transformed using custom software and the image analysis toolbox from MATLAB (The MathWorks, Natick, MA). These data measure the anterior-posterior (A-P), and medial lateral (M-L) displacement of the fibular head relative to the tibia. Statistical analysis was performed using stepwise regression methods (forward selection with replacement). The experimental design used to define the tests performed on the specimens permitted the investigation of main and curvilinear effects of loading variables and implant conditions, as well as all linear and curvilinear two factor interactions. All analysis was done using SAS version 9.2 software.
Results
Data for each specimen were plotted and analyzed visually for stability based on scatter. As a result of this analysis dummy variables to account for ordinary specimen-to-specimen differences were included in the analysis. Variables found to have a significant correlation (p < 0.05) with PTFJ motion are summarized in Appendix 1. While specimen-to-specimen differences were statistically significant their inclusion in the model served only to reduce the residual error of the final model. Since the same effects were significant with or without the effect of specimen differences the final models were built without including terms (dummy variables) to account for specimen effects.
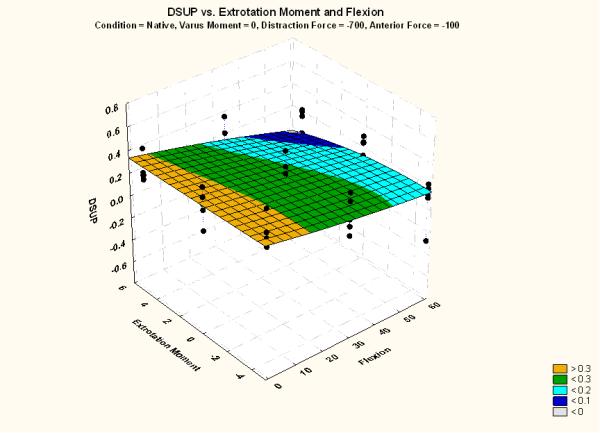
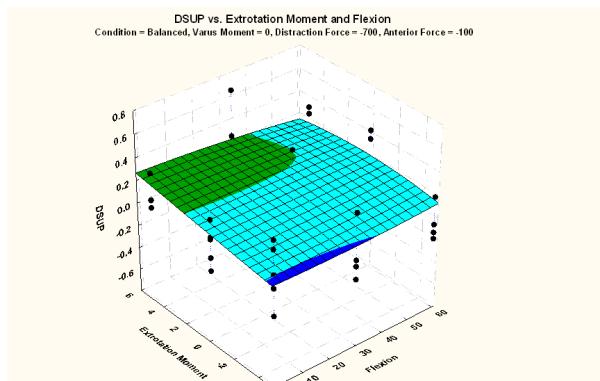
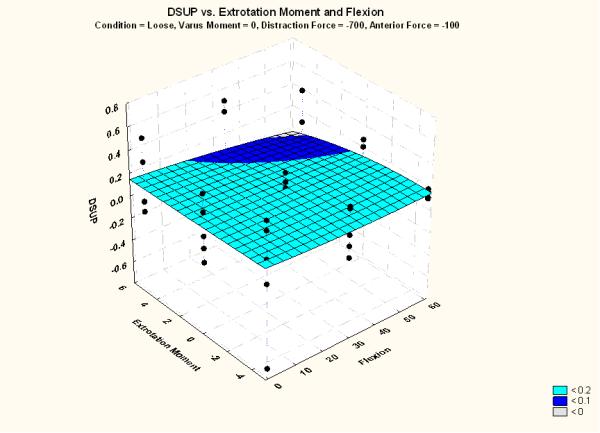
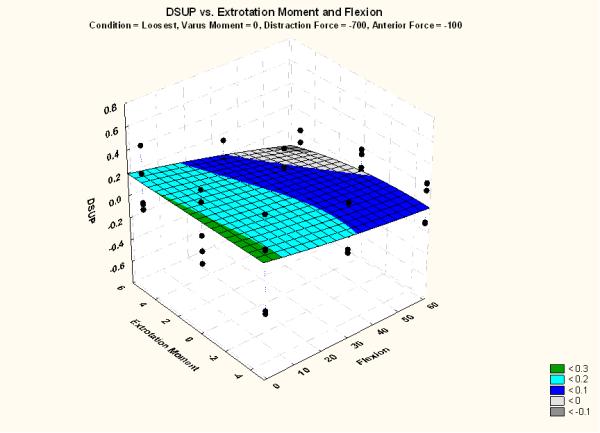
Stepwise multiple regression models for anterior and superior motion of the PTFJ are detailed in Appendix 2 and Appendix 3, respectively. Cells highlighted in yellow indicate the variables with the most influence on displacement for a unit change in the respective value. With respect to anterior displacement, external rotation had the largest effect on motion. Figure 2 illustrates the effect of flexion and external rotation on anterior displacement, while holding constant the other variables (i.e. varus moment = 0 Nm; compression = 700 N; posterior drawer = 100 N). Over a 1 mm decrease in motion was measured in all 4 conditions as external rotation changed from 5 Nm to −5 Nm. The pattern revealed by the posterior motion (i.e., < 0) is most pronounced in both unbalanced TKA conditions (Figure 2C and 2D). If external rotation is held constant (at 5 Nm), the effect of flexion and varus moment on anterior motion is observed as is shown in Figure 3. The thickness of the polyethylene (i.e., condition) as well as the interaction between polyethylene thickness and varus moment consistently show substantial effect on anterior motion (Figure 3; Appendix 2).
Figure 2.
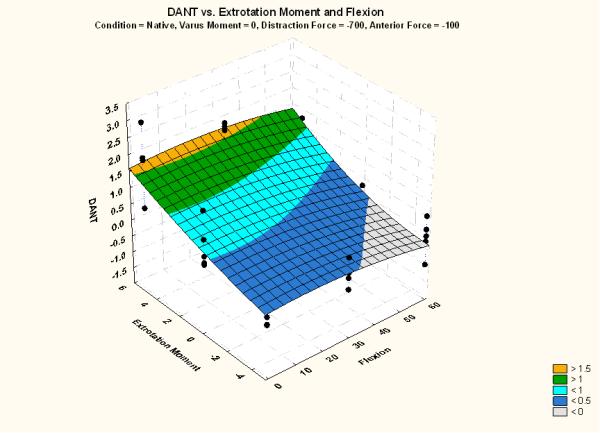
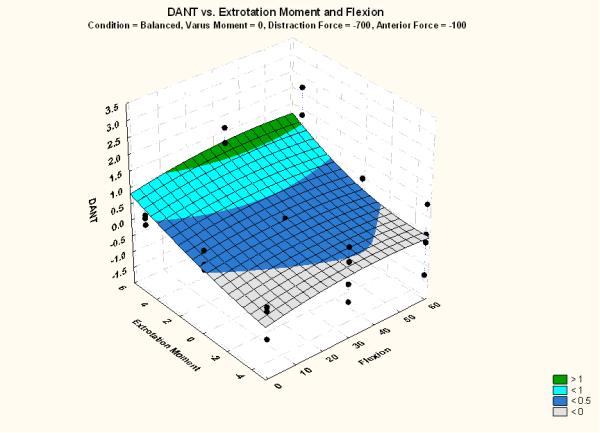
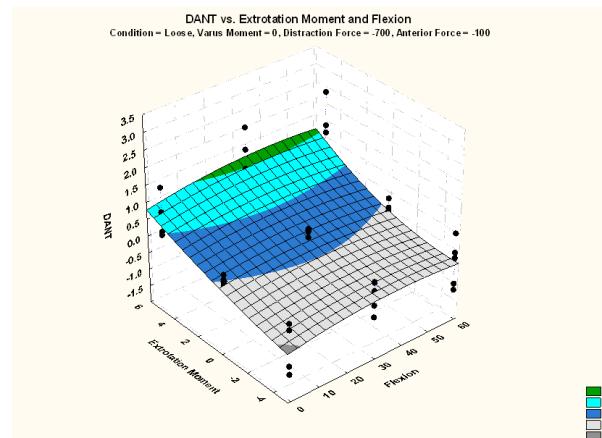
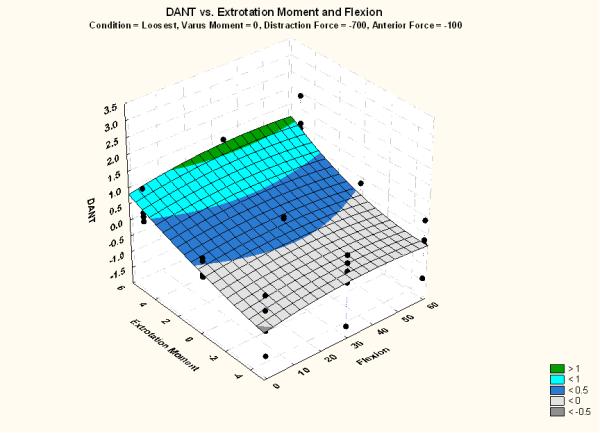
Effect of flexion and external rotation on anterior motion for (A) native knee, (B) balanced TKA, (C) loose condition TKA, and (D) loosest condition TKA. Other variables held constant (varus moment = 0 Nm; compression = 700 N; posterior drawer = 100 N).
Figure 3.
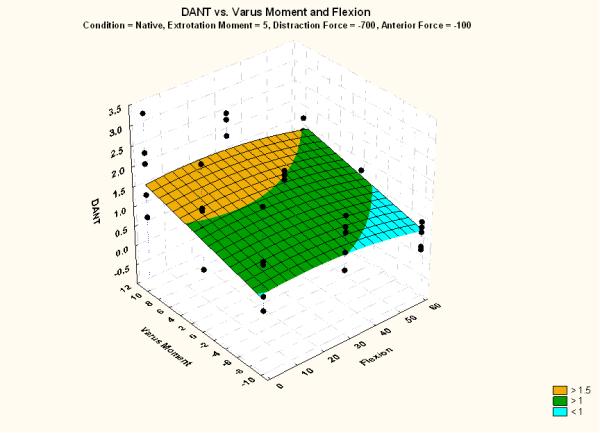
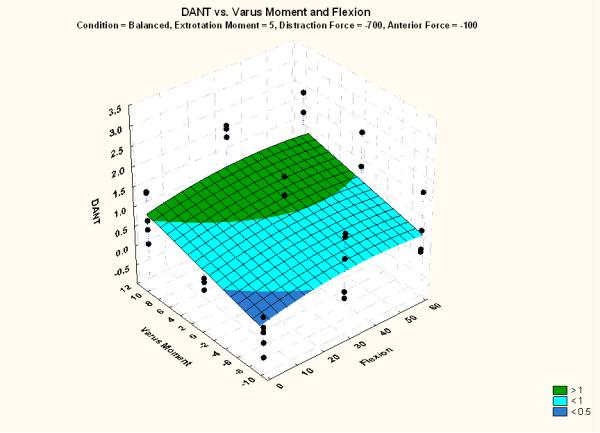
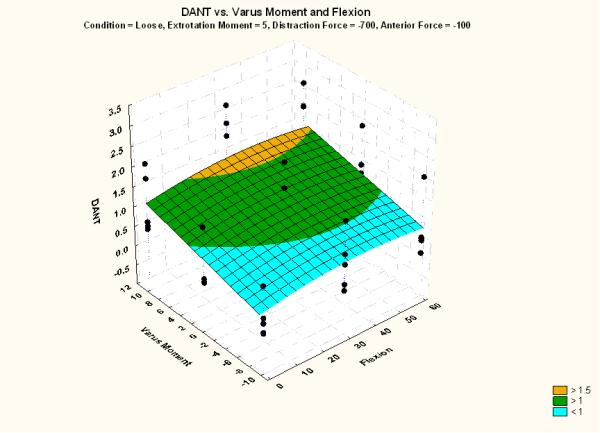
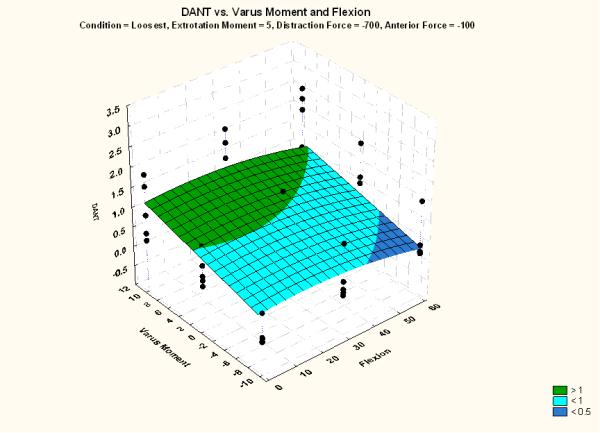
Effect of flexion and varus moment on anterior motion for (A) native knee, (B) balanced TKA, (C) loose condition TKA, and (D) loosest condition TKA. Other variables held constant (varus moment = 5 Nm; compression = 700 N; posterior drawer = 100 N).
Figure 4 highlights the effect of flexion and external rotation on superior displacement, while holding constant the other variables (i.e. varus moment = 0 Nm; compression = 700 N; posterior drawer = 100 N). Inferior motion (i.e., < 0) was rarely observed in the native (Figure 4A) and balanced TKA specimens (Figure 4B), while this motion increased as polyethylene thickness decreased (Figure 4C and 4D). Superior displacement was most affected by posterior drawer, with greater motion observed under 100 N (Appendix 3).
Figure 4.
Effect of flexion and external rotation on superior motion for (A) native knee, (B) balanced TKA, (C) loose condition TKA, and (D) loosest condition TKA. Other variables held constant (varus moment = 0 Nm; compression = 700 N; posterior drawer = 100 N).
Results of the simulated weight bearing (700 Nm compression) showed that motion was dampened when compared with the 100 Nm loading condition. More fibular motion was observed when torque was applied in external rotation in all conditions. Posterior displacement of the fibular head was often seen in unbalanced knees, but never in the native or balanced knee. Motion at the PTFJ, as measured by a marker in the fibular head relative to the tibia, was affected by polyethylene thickness, but not equally at all flexion angles. Unbalanced knees consistently demonstrated greater motion at the PTFJ than appropriately balanced knees.
Discussion
Failures of TKA have an annual cost of $1.5 billion dollars in the Unites States alone9. Additionally, the cost of both physical and mental suffering for patients who have the procedure is unquantifiable and represent an average indirect cost (i.e., lost labor/productivity) of $10,500 USD10. These failures can be divided into three main categories; iatrogenic causes, such as malalignment, extensor mechanism disruption, etc, the second category is infection while the third would be inadequate prosthetic design. Instability and abnormal kinematics are most commonly affected by the first and third of these categories. With improved designs attempting to more appropriately mimic tibiofemoral motion, we may expect to see improved function. Additionally, with more knowledge of soft tissue balancing, our hope is to see a reduction in iatrogenic instability. With a reproducible, validated model of knee instability, we may lay a foundation to better understand causes of instability and present a platform for better implant designs.
Flexion and mid-flexion instability in TKA have been difficult to quantify. Abnormal kinematics have been linked to pain and the need for revision. While tibiofemoral kinematics is the main aspect of TKA performance, the effects on adjacent tissues should not be overlooked. The PTFJ is the site of insertion for several important anatomic structures and experiences significant mechanical forces during daily activities11. Here we have shown that PTFJ kinematics are affected by the balancing of the TKA. Our data illustrate that motion is changed not only quantitatively, but also qualitatively resulting in pathologic motion relative to the native knee.
There are several novel attributes to the testing. First, this cadaveric model allowed for any combined 3D force and moment loading of the joint, including compression to simulate weight bearing. Second, we collected data on motion of an understudied joint in both the A-P and M-L planes in total knee replacement building off of the pilot work we have completed with native knees. Finally, we believe that this may serve as the foundation for better quantifiying instability and serves as a model to examine knee kinematics.
Recent efforts to improve patient function and satisfaction have focused on both knee design as well as surgical approaches with the goal being quicker recovery and TKAs with more normal kinematics. We believe that we have succeeded in creating a reproducible model of motion of the PTFJ after TKA. It is our hope that this model will provide the basis for future studies on the quantification of instability in TKA. This model may aid in the understanding of pain following TKA and may be used in the design of more anatomic kinematics in total knee prosthetics.
Supplementary Material
Acknowledgements
We acknowledge Stryker Corporation and the U.S. National Institutes of Health (NIAMS Core Center Grant #1P30 AR-050953) for financial support. Image analysis was performed by Elliott Lorenz. Dr. Barsoum would like to report the following disclosures: Research support from Stryker Orthopaedics, Zimmer, Salient Surgical Technologies, Brand X, LLC., and Cool Systems, Inc.; Royalties from Exactech, Wright Medical, and SS White; Company equity in Otismed; Consultant with Stryker Orthopaedics, Wright Medical, and SS White.
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB. Does total knee replacement restore normal knee function? Clin Orthop Relat Res. 2005;431:157–165. doi: 10.1097/01.blo.0000150130.03519.fb. [DOI] [PubMed] [Google Scholar]
- 4.Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:315–318. doi: 10.1097/00003086-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 5.Mont MA, Serna FK, Krackow KA, Hungerford DS. Exploration of radiographically normal total knee replacements for unexplained pain. Clin Orthop Relat Res. 1996;331:216–220. doi: 10.1097/00003086-199610000-00030. [DOI] [PubMed] [Google Scholar]
- 6.Firestone TP, Eberle RW. Surgical management of symptomatic instability following failed primary total knee replacement. J Bone Joint Surg Am. 2006;88(Suppl 4):80–84. doi: 10.2106/JBJS.F.00825. [DOI] [PubMed] [Google Scholar]
- 7.Lambert KL. The weight-bearing function of the fibula. A strain gauge study. J Bone Joint Surg Am. 1971;53:507–513. [PubMed] [Google Scholar]
- 8.Scott J, Lee H, Barsoum W, van den Bogert A. The effect of tibiofemoral loading on proximal tibiofibular joint motion. Journal of Anatomy. 2007;211:647–53. doi: 10.1111/j.1469-7580.2007.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.HCUP Databases (Nationwide Inpatient Sample) Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality. 1998-2005.
- 10.Gupta S, Hawker GA, Laporte A, Croxford R, Coyte PC. The economic burden of disabling hip and knee osteoarthritis (OA) from the perspective of individuals living with this condition. Rheumatology. 2005;44:1531–1537. doi: 10.1093/rheumatology/kei049. [DOI] [PubMed] [Google Scholar]
- 11.LaPrade RF, Tso A, Wentorf FA. Force measurements on the fibular collateral ligament, popliteofibular ligament, and popliteus tendon to applied loads. Am J Sports Med. 2004;32:1695–1701. doi: 10.1177/0363546503262694. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


